Chronic Mesenteric Ischemia Is: A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recent Advances in Surgery the Blind-Loop Syndrome After Gastric
Recent advances in surgery Conducted by ALFRED BLALOCK, M.D. The blind-loop syndrome after gastric operations ince the earliest reports by Whitees time, several examples of the blind-loop ANATOMIC CONFIGURATION OF BLIND LOOPS Various examples of gastrointestinal blind and Wangensteen;O a side-arm loop has been employed as in Fig. 1, A, in which the loop is arranged so as to be self-filling. The side loop arrangement is the one which most 849 850 Recent advances in surgery Surgery ;.$ Nouernbcr 1961 & ad cumulated from observations on lesions at differing sites in the gastrointestinal tract. The principles involved apply, with varia- tions, to blind loops at all levels. The best- known feature of the blind-loop syndrome is megaloblastic anemia, which is due to dis- ruption of vitamin BI2 absorption. Normally, dietary vitamin B12 (Castle's extrinsic fac- tor) is absorbed after an incompletely under- stood interaction with intrinsic factor (Fig. 3, A), a mucoprotein secreted by the gastric rnu~osa.*~In man, the principal site of B,, absorption is the ileum.7* Vitamin B,, deficiency can develop by a number of alternative mechanisms. Rarely loops which have caGsed the blind-loop- syndrome.- is there dietary deficiency of this nutritional A, Anastomosis with formation of a self-filled stagnant loop, B, with jejunal diverticulosis, C, factor. Commonly, as in pernicious anemia with intestinal strictures, D, after enteroenteros- (Fig. 3, B) or after total gastrectomy,Sgthere tomies or fistulas, and E, after gastric operation. is absent intrinsic factor due to gastric atrophy or the absence. of the stomach, re- resembles a blind loop which develops after spectively. -

Tissue Responses to Ischemia
PERSPECTIVE SERIES Tissue responses to ischemia SERIES INTRODUCTION Tissue ischemia: pathophysiology and therapeutics Gregg L. Semenza Institute of Genetic Medicine, The Johns Hopkins University School of Medicine, CMSC-1004, 600 North Wolfe Street, Baltimore, Maryland 21287-3914, USA. Phone: (410) 955-1619; Fax: (410) 955-0484; E-mail: [email protected]. This issue of the JCI contains the first articles in a Per- has been the preconditioning phenomena that have spective series that focuses on ischemia, the major been demonstrated in virtually every organ, including cause of mortality in the developed world. The specific the heart and brain. Thus, exposure of an organ or tis- mechanisms and consequences of ischemia differ in sue to one or more brief episodes of ischemia will pro- each tissue or organ, which reflects differences in vide protection against subsequent prolonged ischemia anatomy and physiology. For this reason, the series has that would otherwise result in infarction. The precon- been organized to include articles on cerebral (Dennis ditioning stimulus provides an immediate but short- Choi and colleagues), myocardial (Sandy Williams and lived “first window” of protection, which occurs over a Ivor Benjamin), and skeletal muscle (Jeff Isner) period of minutes to hours and requires the altered ischemia, as well as discussions of ischemia in epithe- activity of pre-existing proteins, as well as a delayed but lial tissues (Sanjay Nigam and colleagues) and hypox- sustained “second window” of protection, which per- ia-induced pulmonary vascular remodeling (Norbert sists over a period of hours to days and depends on new Voelkel and Rubin Tuder). In each case, the authors protein synthesis. -

Medullary Ischemia: Clinical and Radiological Approach
Edorium J Radiol 2021;7:100018R02MT2021. THIAM et al. 1 www.edoriumjournalofradiology.com ORIGINALCASE REPORT ARTICLE PEER REVIEWEDOPEN | OPEN ACCESS ACCESS Medullary ischemia: Clinical and radiological approach Mbaye THIAM, Khalifa Ababacar MBAYE, Rokhaya DIAGNE, Amath FALL, Khadiatou Ndiaye DIOUF, Sokhna BA ABSTRACT doi: 10.5348/100018R02MT2021CR Introduction: Spinal cord infarction is a serious neurovascular emergency due to its short-, medium-, and long-term complications. INTRODUCTION Case Report: A 54-year-old patient with no previous history or particular condition hospitalized for an acute Medullary infarction is a serious neurovascular spinal cord injury, with magnetic resonance imaging emergency due to its short-, medium-, and long-term (MRI) showing medullar ischemia without any etiology complications. Spinal cord ischemia is under-diagnosed found. The evolution was marked by a good motor in our continent due to the difficult accessibility of evolution. magnetic resonance imaging (MRI), which is the Conclusion: Medullary infarction is a serious pathology examination of choice for the diagnosis of spinal cord under-diagnosed in our context because of the difficult vascular damage, and also due to its clinical similarities accessibility of MRI. with acute spinal cord injury (inflammatory damage, vascular malformation, spinal bleeding). The etiologies Keywords: Ischemia, MRI, Spinal cord are numerous and heterogeneous such as traumatic causes, arterial dissection, hypotension, atherosclerosis, toxicity, fibrocartilage embolization, sub-renal abdominal How to cite this article aneurysm repair, epidural anesthesia, and vasculitis THIAM M, MBAYE KA, DIAGNE R, FALL A, [1, 2]. We describe the clinico-radiological aspects of a DIOUF KN, BA S. Medullary ischemia: Clinical 54-year-old female patient diagnosed with spinal cord and radiological approach. -
Gait Variability Patterns Are Altered in Healthy Young Individuals During the Acute Reperfusion Phase of Ischemia-Reperfusion Sara A
University of Nebraska at Omaha DigitalCommons@UNO Journal Articles Department of Biomechanics 11-2010 Gait Variability Patterns are Altered in Healthy Young Individuals During the Acute Reperfusion Phase of Ischemia-Reperfusion Sara A. Myers University of Nebraska at Omaha, [email protected] Nicholas Stergiou University of Nebraska at Omaha, [email protected] Iraklis Pipinos University of Nebraska Medical Center Jason Johanning University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unomaha.edu/biomechanicsarticles Part of the Biomechanics Commons Recommended Citation Myers, Sara A.; Stergiou, Nicholas; Pipinos, Iraklis; and Johanning, Jason, "Gait Variability Patterns are Altered in Healthy Young Individuals During the Acute Reperfusion Phase of Ischemia-Reperfusion" (2010). Journal Articles. 56. https://digitalcommons.unomaha.edu/biomechanicsarticles/56 This Article is brought to you for free and open access by the Department of Biomechanics at DigitalCommons@UNO. It has been accepted for inclusion in Journal Articles by an authorized administrator of DigitalCommons@UNO. For more information, please contact [email protected]. 1 1 Gait variability pattern are altered in healthy young individuals during the acute 2 reperfusion phase of ischemia-reperfusion. 3 Sara A. Myers MS1, Nick Stergiou PhD1,4, Iraklis I. Pipinos MD2,3, Jason M. Johanning MD2,3 4 1 Nebraska Biomechanics Core Facility, University of Nebraska at Omaha, Omaha, NE 5 2Dept of Surgery, University of Nebraska Medical Center, Omaha, NE 6 3Dept of Surgery, Veterans Affairs Medical Center of Nebraska and Western Iowa, Omaha, NE 7 4College of Public Health, University of Nebraska Medical Center, Omaha, NE 8 9 Corresponding Author: Jason M. -

Study Protocol, Status of Data Collection, an Assessment Of
ISCHEMIA Trial Protocol International Study of Comparative Health Effectiveness with Medical and Invasive Approaches Sponsor: National Heart, Lung, and Blood Institute (NHLBI) Study Chair Judith S. Hochman, MD Study Co-Chair David J. Maron, MD Clinical Coordinating Center Cardiovascular Clinical Research Center New York University School of Medicine Statistical and Data Coordinating Duke Clinical Research Institute Center Protocol Version Date: January 18, 2012 Protocol Date: Jan.18.2012 Version 1.0 1 PROTOCOL VERSION AND AMENDMENT TRACKING Version Number/Amendment Approval Date Protocol Date: Jan.18.2012 Version 1.0 2 Protocol Signature Page The signature below constitutes the approval of this protocol and the attachments, and provides the necessary assurances that this trial will be conducted according to all stipulations of the protocol, including all statements regarding confidentiality, and according to local legal and regulatory requirements and applicable regulations and ICH guidelines. Version Date: January 18, 2012 _________________________________ _________________________ Signature of Principal Investigator Date _________________________________ Printed Name of Principal Investigator _________________________________ Name of Facility _________________________________ Location of Facility (City, Country) Protocol Date: Jan.18.2012 Version 1.0 3 CLINICAL TRIAL SUMMARY Title International Study of Comparative Health Effectiveness with Medical and Invasive Approaches Study Objectives Primary objective is to determine whether an -

Effects on Cardiac Function
www.nature.com/scientificreports OPEN Efects on cardiac function, remodeling and infammation following myocardial ischemia–reperfusion injury or unreperfused myocardial infarction in hypercholesterolemic APOE*3‑Leiden mice Niek J. Pluijmert1*, Cindy I. Bart1, Wilhelmina H. Bax1, Paul H. A. Quax2,3 & Douwe E. Atsma1 Many novel therapies to treat myocardial infarction (MI), yielding promising results in animal models, nowadays failed in clinical trials for several reasons. The most used animal MI model is based on permanent ligation of the left anterior descending (LAD) coronary artery in healthy mice resulting in transmural MI, while in clinical practice reperfusion is usually accomplished by primary percutaneous coronary interventions (PCI) limiting myocardial damage and inducing myocardial ischemia–reperfusion (MI‑R) injury. To evaluate a more similar murine MI model we compared MI‑R injury to unreperfused MI in hypercholesterolemic apolipoprotein (APO)E*3‑Leiden mice regarding efects on cardiac function, left ventricular (LV) remodeling and infammation. Both MI‑R and MI resulted in signifcant LV dilation and impaired cardiac function after 3 weeks. Although LV dilation, displayed by end‑diastolic (EDV) and end‑systolic volumes (ESV), and infarct size (IS) were restricted following MI‑R compared to MI (respectively by 27.6% for EDV, 39.5% ESV, 36.0% IS), cardiac function was not preserved. LV‑wall thinning was limited with non‑transmural LV fbrosis in the MI‑R group (66.7%). Two days after inducing myocardial ischemia, local leucocyte infltration in the infarct area was decreased following MI‑R compared to MI (36.6%), whereas systemic circulating monocytes were increased in both groups compared to sham (130.0% following MI‑R and 120.0% after MI). -

A Review on the Pathophysiology and Management of Anterior Spinal Artery Syndrome
J Spine Res Surg 2020; 2 (4): 085-096 DOI: 10. 26502/fjsrs0019 Review Article A Review on the Pathophysiology and Management of Anterior Spinal Artery Syndrome Masum Rahman1*, Sajedur Rahman2, Abu Bakar Siddik3, Mohammad D Hossain2, Juna Musa4, Radzi Hamjah5, Salman Salehin6, Mohmmad Alvi1, Lucas P Carlstrom1, Desmond A Brown1 1Department of Neurosurgery, Mayo Clinic, Rochester, MN, USA 2Jalalabad Ragib Rabeya Medical College and hospital, Sylhet, Bangladesh 3Northern International Medical College and Hospital, Dhaka, Bangladesh 4Department of Surgery, Critical Care Trauma, Mayo Clinic, Rochester, MN, USA 5Harvard TH Chan School of Public Health, Massachusetts, USA 6Department of Internal Medicine, University of Texas Medical Branch (UTMB), Texas, USA *Corresponding Author: Masum Rahman, Department of Neurosurgery, Mayo Clinic, Rochester, MN, USA, Tel: +1 (507) 319-9044; E- mail: [email protected] Received: 01 October 2020; Accepted: 09 October 2020; Published: 20 October 2020 Citation: Masum Rahman, Sajedur Rahman, Abu Bakar Siddik, Mohammad D Hossain, Juna Musa, Radzi Hamjah, Salman Salehin, Mohmmad Alvi, Lucas P Carlstrom, Desmond A Brown. A Review on the Pathophysiology and Management of Anterior Spinal Artery Syndrome. Journal of Spine Research and Surgery 2 (2020): 085-096. Abstract blood flow disruption is essential for patient As an uncommon cause of spinal cord infarction, management. This review article highlights the critical anterior spinal cord syndrome can manifest with motor clinical manifestation of Anterior spinal artery paralysis, loss of pain, and temperature sensation distal syndrome. It also describes etiology, pathogenesis, to the lesion site. The primary pathogenesis of this diagnosis, prognosis, possible management, and syndrome is the disruption of blood flow in the anterior complications. -

Long-Term Outcome After Neonatal Meconium Obstruction
Long-term Outcome After Neonatal Meconium Obstruction Julie R. Fuchs, MD, and Jacob C. Langer, MD ABSTRACT. Objective. It is unclear whether children meconium ileus and those undergoing resection or enter- with cystic fibrosis (CF) who present with neonatal ostomy. Patients with meconium obstruction who do not meconium ileus have a different long-term outcome from have CF have an excellent long-term prognosis. This those presenting later in childhood with pulmonary com- information will be useful in counseling the families of plications or failure to thrive. We examined a cohort of infants presenting with neonatal meconium obstruction. patients with meconium ileus, and compared their long- Pediatrics 1998;101(4). URL: http://www.pediatrics.org/ term outcome with children who had CF without meco- cgi/content/full/101/4/e7; cystic fibrosis, meconium ileus, nium ileus and neonates who had meconium obstruction meconium plug syndrome. without CF (meconium plug syndrome). Study Design. Comparative study using retrospective and follow-up interview data. ABBREVIATION. CF, cystic fibrosis. Patients. Group 1 consisted of 35 surviving CF pa- tients who presented with meconium ileus between 1966 econium obstruction in the neonate is a and 1992. Two control groups were also studied: 35 age- spectrum of disease that includes meco- and sex-matched CF patients without meconium ileus 1 (group 2), and 12 infants presenting with meconium plug Mnium ileus and meconium plug syndrome. syndrome during the same time period (group 3). Meconium ileus is characterized by extremely viscid, Outcome Measures. Pulmonary, gastrointestinal, nu- protein-rich inspissated meconium causing terminal tritional, and functional status were reviewed, and sur- ileal obstruction, and accounts for approximately gical complications were recorded. -
Diagnostic Codes
DISEASES OF THE DIGESTIVE SYSTEM DISEASES OF ORAL CAVITY, SALIVARY GLANDS AND JAWS (520 - 529.9) 520 DISORDERS OF TOOTH DEVELOPMENT AND ERUPTION 520.0 ANODONTIA 520.1 SUPERNUMERARY TEETH 520.2 ABNORMALITIES OF SIZE AND FORM 520.3 MOTTLED TEETH 520.4 DISTURBANCES OF TOOTH FORMATION 520.5 HEREDITARY DISTURBANCES IN TOOTH STRUCTURE, NOT ELSEWHERE CLASSIFIED 520.6 DISTURBANCES IN TOOTH ERUPTION 520.7 TEETHING SYNDROME 520.8 OTHER DISORDERS OF TOOTH DEVELOPMENT 520.9 UNSPECIFIED 521 DISEASES OF HARD TISSUES OF TEETH 521.0 DENTAL CARIES 521.1 EXCESSIVE ATTRITION 521.2 ABRASION 521.3 EROSION 521.4 PATHOLOGICAL RESORPTION 521.5 HYPERCEMENTOSIS 521.6 ANKYLOSIS OF TEETH 521.7 POSTERUPTIVE COLOUR CHANGES 521.8 OTHER DISEASES OF HARD TISSUES OF TEETH 521.9 UNSPECIFIED 522 DISEASES OF PULP AND PERIAPICAL TISSUES 522.0 PULPITIS 522.1 NECROSIS OF THE PULP 522.2 PULP DEGENERATION 522.3 ABNORMAL HARD TISSUE FORMATION IN PULP 522.4 ACUTE APICAL PERIODONTITIS OF PULPAL ORIGIN 522.5 PERIAPICAL ABSCESS WITHOUT SINUS 522.6 CHRONIC APICAL PERIODONTITIS 522.7 PERIAPICAL ABSCESS WITH SINUS 522.8 RADICULAR CYST 522.9 OTHER AND UNSPECIFIED 523 GINGIVAL AND PERIODONTAL DISEASES 523.0 ACUTE GINGIVITIS 523.1 CHRONIC GINGIVITIS 523.2 GINGIVAL RECESSION 523.3 ACUTE PERIODONTITIS 523.4 CHRONIC PERIODONTITIS 523.5 PERIODONTOSIS 523.6 ACCRETIONS ON TEETH 523.8 OTHER PERIODONTAL DISEASES 523.9 UNSPECIFIED 524 DENTOFACIAL ANOMALIES, INCLUDING MALOCCLUSION 524.0 MAJOR ANOMALIES OF JAW SIZE 524.1 ANOMALIES OF RELATIONSHIP OF JAW TO CRANIAL BASE 524.2 ANOMALIES OF DENTAL ARCH -
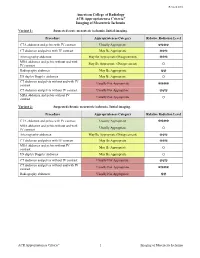
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

Dysfunction of the Continent Ileostomy: Clinical Features and Bacteriology*
Gut: first published as 10.1136/gut.24.3.193 on 1 March 1983. Downloaded from Gut, 1983, 24, 193-201 Dysfunction of the continent ileostomy: clinical features and bacteriology* DARLENE G KELLY, S F PHILLIPS. K A KELLY, W M WEINSTEIN, AND MARY J R GILCHRIST From the Gastroenterology Unit and Department of Laboratorv Medicine, Mayo Clinic and Mayo Foundation, Rochester, Minnesota, and the Departmlent of Medicine, University of California, Los Angeles, California, USA SUMMARY The pathogenesis and treatment of dysfunction of the continent ileostomy was investigated in 12 patients, five of whom had asymptomatic malabsorption and seven of whom had acute complaints. The number of anaerobic bacteria in jejunal aspirates was increased in patients with pouch malfunction (range 103 to 108/g aspirate), but the microbiology of ileal effluent and the morphology of the ileal mucosa could not be correlated with dysfunction. Bile acid breath tests and lactose tolerance tests were not, however, reliable indicators of jejunal bacterial overgrowth. The symptoms, the malabsorption, and the number of jejunal and ileal anaerobic bacteria decreased in patients during treatment with metronidazole, implicating overgrowth of anaerobic bacterial flora in the pathogenesis of the syndrome. The continent ileostomy (ileal pouch), devised by vitamin B12,9 12 proliferation of anaerobic bacteria http://gut.bmj.com/ Kock,' has been used as an alternative to con- in the pouch,9 inflammation in the pouch,7 ventional ileostomy for selected patients with incontinence,"' difficulty with intubation,1' and ulcerative colitis and familial polyposis.2-5 The bloody discharge.5 We previously reported reservoir functions satisfactorily in most patients, diarrhoea with some features of malabsorption in but malfunction of the 'nipple valve' may occur in up approximately one-third of asymptomatic patients to a third of patients and lead to incontinence.