Morphea in Pediatrics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Understanding and Managing Scleroderma
Understanding and Managing Scleroderma A publication of Scleroderma Foundation 300 Rosewood Drive, Suite 105 Danvers, MA 01923 Maureen D. Mayes, M.D., M.P.H. Understanding and Understanding My notes and Managing Scleroderma Managing Scleroderma This booklet is intended to help people with scleroderma, their families and others interested ________________________ in learning more about the disease to better understand what scleroderma is, what effects ________________________ it may have, and what those with scleroderma can do to help themselves and their physicians ________________________ manage the disease. It answers some of the most frequently asked questions about ________________________ A publication of Maureen D. Mayes, M.D., M.P.H. Scleroderma Foundation 300 Rosewood Drive, Suite 105 scleroderma. Danvers, MA 01923 800-722-HOPE (4673) www.scleroderma.org www.facebook.com/sclerodermaUS www.twitter.com/scleroderma ________________________ Disclaimer The Scleroderma Foundation does not provide medical advice nor does it ________________________ endorse any drug or treatment mentioned herein. ________________________ The material contained in this booklet is presented for general information only. It is not intended to provide medical advice, to answer questions specific to the condition or problems of particular individuals, nor in ________________________ any way to substitute for the professional advice and care of qualified physicians. Mention of particular drugs and/or treatments is for ________________________ information purposes only and does not constitute an endorsement of said drugs and/or treatments. ________________________ Thanks! ________________________ The Scleroderma Foundation expresses its deep appreciation to the many ________________________ physicians whose efforts have led to this booklet. Special thanks are owed to Maureen D. Mayes, M.D., M.P.H., of the ________________________ University of Texas McGovern Medical School, Houston. -

Dermatological Findings in Common Rheumatologic Diseases in Children
Available online at www.medicinescience.org Medicine Science ORIGINAL RESEARCH International Medical Journal Medicine Science 2019; ( ): Dermatological findings in common rheumatologic diseases in children 1Melike Kibar Ozturk ORCID:0000-0002-5757-8247 1Ilkin Zindanci ORCID:0000-0003-4354-9899 2Betul Sozeri ORCID:0000-0003-0358-6409 1Umraniye Training and Research Hospital, Department of Dermatology, Istanbul, Turkey. 2Umraniye Training and Research Hospital, Department of Child Rheumatology, Istanbul, Turkey Received 01 November 2018; Accepted 19 November 2018 Available online 21.01.2019 with doi:10.5455/medscience.2018.07.8966 Copyright © 2019 by authors and Medicine Science Publishing Inc. Abstract The aim of this study is to outline the common dermatological findings in pediatric rheumatologic diseases. A total of 45 patients, nineteen with juvenile idiopathic arthritis (JIA), eight with Familial Mediterranean Fever (FMF), six with scleroderma (SSc), seven with systemic lupus erythematosus (SLE), and five with dermatomyositis (DM) were included. Control group for JIA consisted of randomly chosen 19 healthy subjects of the same age and gender. The age, sex, duration of disease, site and type of lesions on skin, nails and scalp and systemic drug use were recorded. χ2 test was used. The most common skin findings in patients with psoriatic JIA were flexural psoriatic lesions, the most common nail findings were periungual desquamation and distal onycholysis, while the most common scalp findings were erythema and scaling. The most common skin finding in patients with oligoarthritis was photosensitivity, while the most common nail finding was periungual erythema, and the most common scalp findings were erythema and scaling. We saw urticarial rash, dermatographism, nail pitting and telogen effluvium in one patient with systemic arthritis; and photosensitivity, livedo reticularis and periungual erythema in another patient with RF-negative polyarthritis. -
Visual Recognition of Autoimmune Connective Tissue Diseases
Seeing the Signs: Visual Recognition of Autoimmune Connective Tissue Diseases Utah Association of Family Practitioners CME Meeting at Snowbird, UT 1:00-1:30 pm, Saturday, February 13, 2016 Snowbird/Alta Rick Sontheimer, M.D. Professor of Dermatology Univ. of Utah School of Medicine Potential Conflicts of Interest 2016 • Consultant • Paid speaker – Centocor (Remicade- – Winthrop (Sanofi) infliximab) • Plaquenil – Genentech (Raptiva- (hydroxychloroquine) efalizumab) – Amgen (etanercept-Enbrel) – Alexion (eculizumab) – Connetics/Stiefel – MediQuest • Royalties Therapeutics – Lippincott, – P&G (ChelaDerm) Williams – Celgene* & Wilkins* – Sanofi/Biogen* – Clearview Health* Partners • 3Gen – Research partner *Active within past 5 years Learning Objectives • Compare and contrast the presenting and Hallmark cutaneous manifestations of lupus erythematosus and dermatomyositis • Compare and contrast the presenting and Hallmark cutaneous manifestations of morphea and systemic sclerosis Distinguishing the Cutaneous Manifestations of LE and DM Skin involvement is 2nd most prevalent clinical manifestation of SLE and 2nd most common presenting clinical manifestation Comprehensive List of Skin Lesions Associated with LE LE-SPECIFIC LE-NONSPECIFIC Cutaneous vascular disease Acute Cutaneous LE Vasculitis Leukocytoclastic Localized ACLE Palpable purpura Urticarial vasculitis Generalized ACLE Periarteritis nodosa-like Ten-like ACLE Vasculopathy Dego's disease-like Subacute Cutaneous LE Atrophy blanche-like Periungual telangiectasia Annular Livedo reticularis -

Interstitial Granuloma Annulare Triggered by Lyme Disease
Volume 27 Number 5| May 2021 Dermatology Online Journal || Case Presentation 27(5):11 Interstitial granuloma annulare triggered by Lyme disease Jordan Hyde1 MD, Jose A Plaza1,2 MD, Jessica Kaffenberger1 MD Affiliations: 1Division of Dermatology, The Ohio State University Wexner Medical Center, Columbus, Ohio, USA, 2Department of Pathology, The Ohio State University Wexner Medical Center, Columbus, Ohio, USA Corresponding Author: Jessica Kaffenberger MD, Division of Dermatology, The Ohio State University Medical Wexner Medical Center, Suite 240, 540 Officenter Place, Columbus, OH 43230, Tel: 614-293-1707, Email: [email protected] been associated with a variety of systemic diseases Abstract including diabetes mellitus, malignancy, thyroid Granuloma annulare is a non-infectious disease, dyslipidemia, and infection [3,4]. granulomatous skin condition with multiple different associations. We present a case of a man in his 60s There are multiple histological variants of GA, with a three-week history of progressive targetoid including interstitial GA. The histopathology of plaques on his arms, legs, and trunk. Skin biopsy classic GA demonstrates a focal degeneration of demonstrated interstitial granuloma annulare. collagen surrounded by an inflammatory infiltrate Additional testing revealed IgM antibodies to Borrelia composed of lymphocytes and histiocytes. In a less burgdorferi on western blot suggesting interstitial common variant, interstitial GA, scattered histiocytes granuloma annulare was precipitated by the recent are seen -

A Review of the Evidence for and Against a Role for Mast Cells in Cutaneous Scarring and Fibrosis
International Journal of Molecular Sciences Review A Review of the Evidence for and against a Role for Mast Cells in Cutaneous Scarring and Fibrosis Traci A. Wilgus 1,*, Sara Ud-Din 2 and Ardeshir Bayat 2,3 1 Department of Pathology, Ohio State University, Columbus, OH 43210, USA 2 Centre for Dermatology Research, NIHR Manchester Biomedical Research Centre, Plastic and Reconstructive Surgery Research, University of Manchester, Manchester M13 9PT, UK; [email protected] (S.U.-D.); [email protected] (A.B.) 3 MRC-SA Wound Healing Unit, Division of Dermatology, University of Cape Town, Observatory, Cape Town 7945, South Africa * Correspondence: [email protected]; Tel.: +1-614-366-8526 Received: 1 October 2020; Accepted: 12 December 2020; Published: 18 December 2020 Abstract: Scars are generated in mature skin as a result of the normal repair process, but the replacement of normal tissue with scar tissue can lead to biomechanical and functional deficiencies in the skin as well as psychological and social issues for patients that negatively affect quality of life. Abnormal scars, such as hypertrophic scars and keloids, and cutaneous fibrosis that develops in diseases such as systemic sclerosis and graft-versus-host disease can be even more challenging for patients. There is a large body of literature suggesting that inflammation promotes the deposition of scar tissue by fibroblasts. Mast cells represent one inflammatory cell type in particular that has been implicated in skin scarring and fibrosis. Most published studies in this area support a pro-fibrotic role for mast cells in the skin, as many mast cell-derived mediators stimulate fibroblast activity and studies generally indicate higher numbers of mast cells and/or mast cell activation in scars and fibrotic skin. -

2017 Oregon Dental Conference® Course Handout
2017 Oregon Dental Conference® Course Handout Nasser Said-Al-Naief, DDS, MS Course 8125: “The Mouth as The Body’s Mirror: Oral, Maxillofacial, and Head and Neck Manifestations of Systemic Disease” Thursday, April 6 2 pm - 3:30 pm 2/28/2017 The Mouth as The Body’s Mirror Oral Maxillofacial and Head and Neck Manifestation of Ulcerative Conditions of Allergic & Immunological Systemic Disease the Oro-Maxillofacial Diseases Region Nasser Said-Al-Naief, DDS, MS Professor & Chair, Oral Pathology and Radiology Director, OMFP Laboratory Oral manifestations of Office 503-494-8904// Direct: 503-494-0041 systemic diseases Oral Manifestations of Fax: 503-494-8905 Dermatological Diseases Cell: 1-205-215-5699 Common Oral [email protected] Conditions [email protected] OHSU School of Dentistry OHSU School of Medicine 2730 SW Moody Ave, CLSB 5N008 Portland, Oregon 97201 Recurrent aphthous stomatitis (RAS) Recurrent aphthous stomatitis (RAS) • Aphthous" comes from the Greek word "aphtha”- • Recurrence of one or more painful oral ulcers, in periods of days months. = ulcer • Usually begins in childhood or adolescence, • The most common oral mucosal disease in North • May decrease in frequency and severity by age America. (30+). • Affect 5% to 66% of the North American • Ulcers are confined to the lining (non-keratinized) population. mucosa: • * 60% of those affected are members of the • Buccal/labial mucosa, lateral/ventral tongue/floor of professional class. the mouth, soft palate/oropharyngeal mucosa • Etiopathogenesis: 1 2/28/2017 Etiology of RAU Recurrent Aphthous Stomatitis (RAS): Types: Minor; small size, shallow, regular, preceeded by prodrome, heal in 7-10 days Bacteria ( S. -

Foot Pain in Scleroderma
Foot Pain in Scleroderma Dr Begonya Alcacer-Pitarch LMBRU Postdoctoral Research Fellow 20th Anniversary Scleroderma Family Day 16th May 2015 Leeds Institute of Rheumatic and Musculoskeletal Medicine Presentation Content n Introduction n Different types of foot pain n Factors contributing to foot pain n Impact of foot pain on Quality of Life (QoL) Leeds Institute of Rheumatic and Musculoskeletal Medicine Scleroderma n Clinical features of scleroderma – Microvascular (small vessel) and macrovascular (large vessel) damage – Fibrosis of the skin and internal organs – Dysfunction of the immune system n Unknown aetiology n Female to male ratio 4.6 : 1 n The prevalence of SSc in the UK is 8.21 per 100 000 Leeds Institute of Rheumatic and Musculoskeletal Medicine Foot Involvement in SSc n Clinically 90% of SSc patients have foot involvement n It typically has a later involvement than hands n Foot involvement is less frequent than hand involvement, but is potentially disabling Leeds Institute of Rheumatic and Musculoskeletal Medicine Different Types of Foot Pain Leeds Institute of Rheumatic and Musculoskeletal Medicine Ischaemic Pain (vascular) Microvascular disease (small vessel) n Intermittent pain – Raynaud’s (spasm) • Cold • Throb • Numb • Tingle • Pain n Constant pain – Vessel center narrows • Distal pain (toes) • Gradually increasing pain • Intolerable pain when necrosis is present Leeds Institute of Rheumatic and Musculoskeletal Medicine Ischaemic Pain (vascular) Macrovascular disease (large vessels) n Intermittent and constant pain – Peripheral Arterial Disease • Intermittent claudication – Muscle pain (ache, cramp) during walking • Aching or burning pain • Night and rest pain • Cramps Leeds Institute of Rheumatic and Musculoskeletal Medicine Ulcer Pain n Ulcer development – Constant pain n Infected ulcer – Unexpected/ excess pain or tenderness Leeds Institute of Rheumatic and Musculoskeletal Medicine Neuropathic Pain n Nerve damage is not always obvious. -

A Patient with Plaque Type Morphea Mimicking Systemic Lupus Erythematosus
CASE REPORT A Patient With Plaque Type Morphea Mimicking Systemic Lupus Erythematosus Wardhana1, EA Datau2 1 Department of Internal Medicine, Siloam International Hospitals. Karawaci, Indonesia. 2 Department of Internal Medicine, Prof. Dr. RD Kandou General Hospital & Sitti Maryam Islamic Hospital, Manado, North Sulawesi, Indonesia. Correspondence mail: Siloam Hospitals Group’s CEO Office, Siloam Hospital Lippo Village. 5th floor. Jl. Siloam No.6, Karawaci, Indonesia. email: [email protected] ABSTRAK Morfea merupakan penyakit jaringan penyambung yang jarang dengan gambaran utama berupa penebalan dermis tanpa disertai keterlibatan organ dalam. Penyakit ini juga dikenal sebagai bagian dari skleroderma terlokalisir. Berdasarkan gambaran klinis dan kedalaman jaringan yang terlibat, morfea dikelompokkan ke dalam beberapa bentuk dan sekitar dua pertiga orang dewasa dengan morfea mempunyai tipe plak. Produksi kolagen yang berlebihan oleh fibroblast merupakan penyebab kelainan pada morfea dan mekanisme terjadinya aktivitas fibroblast yang berlebihan ini masih belum diketahui, meskipun beberapa mekanisme pernah diajukan. Morfe tipe plak biasanya bersifat ringan dan dapat sembuh dengan sendirinya. Morfea tipe plak yang penampilan klinisnya menyerupai lupus eritematosus sistemik, misalnya meliputi alopesia dan ulkus mukosa di mulut, jarang dijumpai. Sebuah kasus morfea tipe plak pada wanita berusia 20 tahun dibahas. Pasien ini diobati dengan imunosupresan dan antioksidan local maupun sistemik. Kondisi paisen membaik tanpa disertai efek samping yang berarti. Kata kunci: morfea, tipe plak. ABSTRACT Morphea is an uncommon connective tissue disease with the most prominent feature being thickening or fibrosis of the dermal without internal organ involvement. It is also known as a part of localized scleroderma. Based on clinical presentation and depth of tissue involvement, morphea is classified into several forms, and about two thirds of adults with morphea have plaque type. -

A Acanthosis Nigricans, 139 Acquired Ichthyosis, 53, 126, 127, 159 Acute
Index A Anti-EJ, 213, 214, 216 Acanthosis nigricans, 139 Anti-Ferc, 217 Acquired ichthyosis, 53, 126, 127, 159 Antigliadin antibodies, 336 Acute interstitial pneumonia (AIP), 79, 81 Antihistamines, 324 Adenocarcinoma, 115, 116, 151, 173 Anti-histidyl-tRNA-synthetase antibody Adenosine triphosphate (ATP), 229 (Anti-Jo-1), 6, 14, 140, 166, 183, Adhesion molecules, 225–226 213–216 Adrenal gland carcinoma, 115 Anti-histone antibodies (AHA), 174, 217 Age, 30–32, 157–159 Anti-Jo-1 antibody syndrome, 34, 129 Alanine aminotransferase (ALT, ALAT), 16, Anti-Ki-67 antibody, 247 128, 205, 207, 255 Anti-KJ antibodies, 216–217 Alanyl-tRNA synthetase, 216 Anti-KS, 82 Aldolase, 14, 16, 128, 129, 205, 207, 255, 257 Anti-Ku antibodies, 163, 165, 217 Aledronate, 325 Anti-Mas, 217 Algorithm, 256, 259 Anti-Mi-2 Allergic contact dermatitis, 261 antibody syndrome, 11, 129, 215 Alopecia, 62, 199, 290 antibodies, 6, 15, 129, 142, 212 Aluminum hydroxide, 325, 326 Anti-Myo 22/25 antibodies, 217 Alzheimer’s disease-related proteins, 190 Anti-Myosin scintigraphy, 230 Aminoacyl-tRNA synthetases, 151, 166, 182, Antineoplastic agents, 172 212, 215 Antineoplastic medicines, 169 Aminoquinolone antimalarials, 309–310, 323 Antinuclear antibody (ANA), 1, 141, 152, 171, Amyloid, 188–190 172, 174, 213, 217 Amyopathic DM, 6, 9, 29–30, 32–33, 36, 104, Anti-OJ, 213–214, 216 116, 117, 147–153 Anti-p155, 214–215 Amyotrophic lateral sclerosis, 263 Antiphospholipid syndrome (APS), 127, Antisynthetase syndrome, 11, 33–34, 81 130, 219 Anaphylaxi, 316 Anti-PL-7 antibody, 82, 214 Anasarca, -
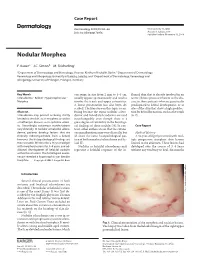
Nodular Morphea
Case Report Dermatology 2009;218:63–66 Received: July 13, 2008 DOI: 10.1159/000173976 Accepted: July 23, 2008 Published online: November 13, 2008 Nodular Morphea a b c F. Kauer J.C. Simon M. Sticherling a b Department of Dermatology and Venerology, Vivantes Klinikum Neukölln, Berlin , Department of Dermatology, c Venerology and Allergology, University of Leipzig, Leipzig , and Department of Dermatology, Venerology and Allergology, University of Erlangen, Erlangen , Germany Key Words can range in size from 2 mm to 4–5 cm, flamed skin that is already involved in an -Scleroderma ؒ Keloid ؒ Hypertrophic scar ؒ usually appear spontaneously and tend to active fibrotic process inherent to the dis Morphea involve the trunk and upper extremities. ease in those patients who are genetically A linear presentation has also been de- predisposed to keloid development, or at scribed. The literature on this topic is con- sites of the skin that show a high predilec- Abstract fusing because the terms ‘nodular sclero- tion for keloid formation, such as the trunk Scleroderma may present as being strictly derma’ and ‘keloidal scleroderma’ are used [6, 7] . limited to the skin, as in morphea, or within interchangeably even though there is a a multiorgan disease, as in systemic sclero- great degree of variability in the histologi- sis. Accordingly, cutaneous manifestations cal findings of these nodules [4] . In con- C a s e R e p o r t vary clinically. In nodular or keloidal sclero- trast, other authors stress that the cutane- derma, patients develop lesions that are ous manifestations may vary clinically, but Medical History clinically indistinguishable from a keloid; all share the same histopathological pat- A 16-year-old girl presented with mul- however, the histopathological findings are tern of both morphea/scleroderma and ke- tiple progressive morpheic skin lesions more variable. -

Topical Photodynamic Therapy for Localized Scleroderma
Acta Derm Venereol 2000; 80: 26±27 Topical Photodynamic Therapy for Localized Scleroderma SIGRID KARRER, CHRISTOPH ABELS, MICHAEL LANDTHALER and ROLF-MARKUS SZEIMIES Department of Dermatology, University of Regensburg, Regensburg, Germany Therapy of localized scleroderma is unsatisfactory, with MATERIAL AND METHODS numerous treatments being used that have only limited success Patients or considerable side-effects. The aim of this trial was to determine whether topical photodynamic therapy would be Five patients aged between 21 and 63 years with biopsy-proven effective in patients with localized scleroderma. Five patients localized scleroderma (morphoea) were studied. All patients had evidence of progressive disease, i.e. lesions showed an in¯ammatory with progressive disease, in whom conventional therapies had reaction and increase in size. In each patient the condition had failed, were treated by application of a gel containing 3% previously failed to respond to potent topical corticosteroids, systemic 5-aminolevulinic acid followed by irradiation with an incoherent therapy with penicillin and/or PUVA bath photochemotherapy. lamp (40 mW/cm2, 10 J/cm2). The treatment was performed Patients were required to discontinue all therapy at least 4 weeks once or twice weekly for 3 ± 6 months. In all patients the before study initiation. The most affected sclerotic plaque of each therapy was highly effective for sclerotic plaques, as measured patient was judged at baseline and then every 2 weeks during by a quantitative durometer score and a clinical skin score. The treatment. Sclerotic plaques were assessed by a clinical skin score (10) only side-effect was a transient hyperpigmentation of the and the durometer score (11). -

Beneath the Surface: Derm Clues to Underlying Disorders
Christian R. Halvorson, MD; Richard Colgan, MD Department of Family and Beneath the surface: Derm clues Community Medicine, University of Maryland School of Medicine, Baltimore to underlying disorders [email protected] Dermatologic fi ndings are frequent indicators of The authors reported no potential confl ict of interest connective tissue disorders. Here’s what to look for. relevant to this article. any systemic conditions are accompanied by skin PRACTICE manifestations. Th is is especially true for connec- RECOMMENDATIONS Mtive tissue disorders, for which dermatologic fi nd- › When evaluating patients ings are often the key to diagnosis. with suspected cutaneous In this review, we describe the dermatologic fi ndings of lupus erythematosus, use some well-known connective tissue disorders. Th e text and multiple criteria—including photographs in the pages that follow will help you hone your histologic and immuno- diagnostic skills, leading to earlier treatment and, possibly, fl uorescent biopsy fi ndings better outcomes. and American College of Rheumatology criteria—to rule out systemic disease. C Lupus erythematosus: Cutaneous › Cancer screening with a and systemic disease often overlap careful history and physi- Lupus erythematosus (LE), a chronic, infl ammatory autoim- cal examination is recom- mended for all adult patients mune condition that primarily aff ects women in their 20s and whom you suspect of having 30s, may initially present as a systemic disease or in a purely dermatomyositis. C cutaneous form. However, most patients with systemic LE have some skin manifestations, and those with cutaneous › Suspect mixed connective LE often have—or subsequently develop—systemic involve- tissue disease in patients 1 with skin fi ndings charac- ment.