200779372.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Monograph on Dematiaceous Fungi
Monograph On Dematiaceous fungi A guide for description of dematiaceous fungi fungi of medical importance, diseases caused by them, diagnosis and treatment By Mohamed Refai and Heidy Abo El-Yazid Department of Microbiology, Faculty of Veterinary Medicine, Cairo University 2014 1 Preface The first time I saw cultures of dematiaceous fungi was in the laboratory of Prof. Seeliger in Bonn, 1962, when I attended a practical course on moulds for one week. Then I handled myself several cultures of black fungi, as contaminants in Mycology Laboratory of Prof. Rieth, 1963-1964, in Hamburg. When I visited Prof. DE Varies in Baarn, 1963. I was fascinated by the tremendous number of moulds in the Centraalbureau voor Schimmelcultures, Baarn, Netherlands. On the other hand, I was proud, that El-Sheikh Mahgoub, a Colleague from Sundan, wrote an internationally well-known book on mycetoma. I have never seen cases of dematiaceous fungal infections in Egypt, therefore, I was very happy, when I saw the collection of mycetoma cases reported in Egypt by the eminent Egyptian Mycologist, Prof. Dr Mohamed Taha, Zagazig University. To all these prominent mycologists I dedicate this monograph. Prof. Dr. Mohamed Refai, 1.5.2014 Heinz Seeliger Heinz Rieth Gerard de Vries, El-Sheikh Mahgoub Mohamed Taha 2 Contents 1. Introduction 4 2. 30. The genus Rhinocladiella 83 2. Description of dematiaceous 6 2. 31. The genus Scedosporium 86 fungi 2. 1. The genus Alternaria 6 2. 32. The genus Scytalidium 89 2.2. The genus Aurobasidium 11 2.33. The genus Stachybotrys 91 2.3. The genus Bipolaris 16 2. -
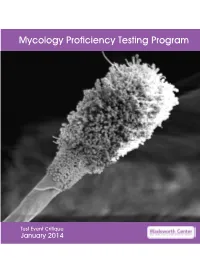
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

N 13. 2. Zigomicetes Identificaci!N De Otros Hongos Miceliares
ïí ×¼»²¬·º·½¿½·‰² ¼» ±¬®±• ¸±²¹±• ³·½»´·¿®»• ïíóï Ö±•»°¿ Ù»²’ Ö±•»° Ù«¿®®± ïíòïò ײ¬®±¼«½½·‰² ïíò îò Æ·¹±³·½»¬»• El aumento de pacientes con alteraciones en Los zigomicetes se diferencian del resto de su sistema inmunitario o la utilización de técnicas hongos miceliares por presentar hifas anchas, rami- agresivas en la medicina moderna, entre otros facto- ficadas, generalmente no septadas, y esporas sexua- res, han propiciado en las últimas décadas un consi- les denominadas zigosporas (Figura 13.1). L a s derable incremento de las infecciones producidas infecciones ocasionadas por estos hongos son referi- por microorganismos saprotrofos. Entre ellos cabe das como zigomicosis. Sin embargo, este término es citar numerosos hongos miceliares habitualmente muy amplio ya que incluye a zigomicetes que perte- colonizadores de diferentes tipos de sustratos vege- necen a dos grupos (órdenes) muy diferentes, los tales y frecuentes en el ambiente que rodea al hom- entomoftorales y los mucorales. Los primeros son bre(suelo,paredeshúmedas,aire...).Hace hongos endémicos de países tropicales y subtropica- relativamente poco tiempo, cuando dichos hongos les que suelen ocasionar micosis subcutáneas [1-3] eran aislados de muestras clínicas solían ser consi- y que no vamos a tratar en este capítulo ya que es derados como meros contaminantes. Sin embargo, difícil encontrarlos en nuestro país. Los mucorales, se ha demostrado reiteradamente que muchos de en cambio, están ampliamente distribuidos por las estos hongos son capaces de infectar al hombre. diferentes áreas geográficas del globo, y algunos de Estos hechos deben ser considerados por los micro- ellos son capaces de ocasionar un amplio rango de biólogos clínicos, los cuales según las evidencias infecciones en el hombre [1-3]. -

Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2013 Mycology Laboratory Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 15 Mold Descriptions 16 M-1 Exserohilum species 16 M-2 Phialophora species 20 M-3 Chrysosporium species 25 M-4 Fusarium species 30 M-5 Rhizopus species 34 Yeast Descriptions 38 Y-1 Rhodotorula mucilaginosa 38 Y-2 Trichosporon asahii 41 Y-3 Candida glabrata 44 Y-4 Candida albicans 47 Y-5 Geotrichum candidum 50 Direct Detection - Cryptococcal Antigen 53 Antifungal Susceptibility Testing - Yeast 55 Antifungal Susceptibility Testing - Mold (Educational) 60 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Aspartic Peptidase of Phialophora Verrucosa As Target of HIV
Journal of Enzyme Inhibition and Medicinal Chemistry ISSN: 1475-6366 (Print) 1475-6374 (Online) Journal homepage: https://www.tandfonline.com/loi/ienz20 Aspartic peptidase of Phialophora verrucosa as target of HIV peptidase inhibitors: blockage of its enzymatic activity and interference with fungal growth and macrophage interaction Marcela Q. Granato, Ingrid S. Sousa, Thabatta L. S. A. Rosa, Diego S. Gonçalves, Sergio H. Seabra, Daniela S. Alviano, Maria C. V. Pessolani, André L. S. Santos & Lucimar F. Kneipp To cite this article: Marcela Q. Granato, Ingrid S. Sousa, Thabatta L. S. A. Rosa, Diego S. Gonçalves, Sergio H. Seabra, Daniela S. Alviano, Maria C. V. Pessolani, André L. S. Santos & Lucimar F. Kneipp (2020) Aspartic peptidase of Phialophoraverrucosa as target of HIV peptidase inhibitors: blockage of its enzymatic activity and interference with fungal growth and macrophage interaction, Journal of Enzyme Inhibition and Medicinal Chemistry, 35:1, 629-638, DOI: 10.1080/14756366.2020.1724994 To link to this article: https://doi.org/10.1080/14756366.2020.1724994 © 2020 The Author(s). Published by Informa Published online: 10 Feb 2020. UK Limited, trading as Taylor & Francis Group. Submit your article to this journal Article views: 318 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=ienz20 JOURNAL OF ENZYME INHIBITION AND MEDICINAL CHEMISTRY 2020, VOL. 35, NO. 1, 629–638 https://doi.org/10.1080/14756366.2020.1724994 RESEARCH PAPER Aspartic peptidase of Phialophora verrucosa as target of HIV peptidase inhibitors: blockage of its enzymatic activity and interference with fungal growth and macrophage interaction aà aà b c,d e Marcela Q. -

Characterization of Phialophora Spp. Isolates from a Montana Take-All Suppressive Soil and Their Use in Suppression of Wheat
Characterization of Phialophora spp. isolates from a Montana take-all suppressive soil and their use in suppression of wheat take-all caused by Gaeumannomyces graminis var. tritici (Ggt) by Narjess Zriba A thesis submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Plant Pathology Montana State University © Copyright by Narjess Zriba (1997) Abstract: Sterile fungi isolated from a Montana take-all suppressive soil were identified as Phialophora spp. and were characterized morphologically. These Phialophora spp. isolates were nonpathogenic on wheat or barley in glasshouse experiments. They, however, did not confer a substantial protection of wheat and barley seedlings against Gaeumannomvces graminis var. tritici (Ggt) in glasshouse tests. Ribosomal DNA (rDNA) fragments from four Phialonhora and two Gaeumannomvces isolates were amplified with Polymerase Chain Reaction (PCR) using universal primers, cloned, and sequenced. Sequence comparison to known sequences of Phialonhora spp. and Gaeumannomvces spp. revealed that the Phialonhora isolates included in this study were very closely related to Gaeumannomvces and less so to other Phialonhora spp. Sequence alignment allowed the design of primers to be used in detecting Phialonhora sp. I-52 in the soil and on cereal roots. Phialonhora sp. I-52 was tentatively identified as P. graminicola based on morphological and molecular analyses. In vitro tests of antagonism involving Phialonhora spp. I-52, I-58, as well as a Bacillus sp. strain L that originated from the same soil as I-52 and I-58, resulted in significant inhibition of Ggt growth. Phialonhora sp. I-52 was combined with Phialonhora sp. I-58 and tested for Ggt suppression in the field and with Bacillus sp. -

A First Comprehensive Census of Fungi in Soil Reveals Both Hyperdiversity
Ecological Monographs, 84(1), 2014, pp. 3–20 Ó 2014 by the Ecological Society of America A first comprehensive census of fungi in soil reveals both hyperdiversity and fine-scale niche partitioning 1,4 2 1,5 3 3 D. LEE TAYLOR, TERESA N. HOLLINGSWORTH, JACK W. MCFARLAND, NIALL J. LENNON, CHAD NUSBAUM, 1 AND ROGER W. RUESS 1Institute of Arctic Biology, 311 Irving I Building, University of Alaska, Fairbanks, Alaska 99775 USA 2USDA Forest Service, PNW Research Station, Boreal Ecology Cooperative Research Unit, Fairbanks, Alaska 99775 USA 3Broad Institute of MIT and Harvard, 320 Charles Street, Cambridge, Massachusetts 02141 USA Abstract. Fungi play key roles in ecosystems as mutualists, pathogens, and decomposers. Current estimates of global species richness are highly uncertain, and the importance of stochastic vs. deterministic forces in the assembly of fungal communities is unknown. Molecular studies have so far failed to reach saturated, comprehensive estimates of fungal diversity. To obtain a more accurate estimate of global fungal diversity, we used a direct molecular approach to census diversity in a boreal ecosystem with precisely known plant diversity, and we carefully evaluated adequacy of sampling and accuracy of species delineation. We achieved the first exhaustive enumeration of fungi in soil, recording 1002 taxa in this system. We show that the fungus : plant ratio in Picea mariana forest soils from interior Alaska is at least 17:1 and is regionally stable. A global extrapolation of this ratio would suggest 6 million species of fungi, as opposed to leading estimates ranging from 616 000 to 1.5 million. We also find that closely related fungi often occupy divergent niches. -

Case Report Phialophora Verrucosa Infection in a BMT Patient
Bone Marrow Transplantation, (1997) 20, 789–791 1997 Stockton Press All rights reserved 0268–3369/97 $12.00 Case report Phialophora verrucosa infection in a BMT patient TS Lundstrom, MR Fairfax, MC Dugan, JA Vazquez, PH Chandrasekar, E Abella and C Kasten-Sportes Detroit Medical Center, Wayne State University, Detroit, MI, USA Summary: Case report Phialophora is a dematiaceous fungus isolated from soil The patient was a 42-year-old Caucasian female diagnosed and wood. Human infections including chromoblasto- with AML (type M4) in February 1994 with 58% blasts on mycosis, mycotic keratitis, cutaneous infections, and bone marrow biopsy. In March 1994 she received induction prosthetic valve endocarditis have been reported. We therapy with idarubicin and cytarabine (Ara-C). Her course report a case of fatal hemorrhage due to Phialophora was complicated by Pseudomonas aeruginosa bacteremia verrucosa in a patient with prolonged neutropenia and Ludwig’s angina. Consolidation therapy in June 1994 undergoing autologous bone marrow transplant (BMT) with idarubicin and Ara-C was complicated by Stenotro- for acute myelogenous leukemia (AML). Bacterial infec- phomonas maltophilia sternal osteomyelitis which was tions complicated induction and consolidation chemo- treated for 6 weeks with intravenous broad-spectrum anti- therapies. Liposomal amphotericin B (LAMB) was biotics. In September 1994 the patient was in complete given from day +33 to day +72 for febrile neutropenia. remission and hospitalized for autologous BMT. Prepara- Death occurred on day +74 due to tracheal hemorrhage. tive therapy consisted of busulfan and cyclosphosphamide. Autopsy revealed granulation tissue on the posterior She received prophylactic norfloxacin and fluconazole. wall of the trachea with fungal hyphae on histopathol- The BMT course was as follows: on day +2, the patient ogy; the tissue grew Phialophora verrucosa. -

Descriptions of Medical Fungi
DESCRIPTIONS OF MEDICAL FUNGI THIRD EDITION (revised November 2016) SARAH KIDD1,3, CATRIONA HALLIDAY2, HELEN ALEXIOU1 and DAVID ELLIS1,3 1NaTIONal MycOlOgy REfERENcE cENTRE Sa PaTHOlOgy, aDElaIDE, SOUTH aUSTRalIa 2clINIcal MycOlOgy REfERENcE labORatory cENTRE fOR INfEcTIOUS DISEaSES aND MIcRObIOlOgy labORatory SERvIcES, PaTHOlOgy WEST, IcPMR, WESTMEaD HOSPITal, WESTMEaD, NEW SOUTH WalES 3 DEPaRTMENT Of MOlEcUlaR & cEllUlaR bIOlOgy ScHOOl Of bIOlOgIcal ScIENcES UNIvERSITy Of aDElaIDE, aDElaIDE aUSTRalIa 2016 We thank Pfizera ustralia for an unrestricted educational grant to the australian and New Zealand Mycology Interest group to cover the cost of the printing. Published by the authors contact: Dr. Sarah E. Kidd Head, National Mycology Reference centre Microbiology & Infectious Diseases Sa Pathology frome Rd, adelaide, Sa 5000 Email: [email protected] Phone: (08) 8222 3571 fax: (08) 8222 3543 www.mycology.adelaide.edu.au © copyright 2016 The National Library of Australia Cataloguing-in-Publication entry: creator: Kidd, Sarah, author. Title: Descriptions of medical fungi / Sarah Kidd, catriona Halliday, Helen alexiou, David Ellis. Edition: Third edition. ISbN: 9780646951294 (paperback). Notes: Includes bibliographical references and index. Subjects: fungi--Indexes. Mycology--Indexes. Other creators/contributors: Halliday, catriona l., author. Alexiou, Helen, author. Ellis, David (David H.), author. Dewey Number: 579.5 Printed in adelaide by Newstyle Printing 41 Manchester Street Mile End, South australia 5031 front cover: Cryptococcus neoformans, and montages including Syncephalastrum, Scedosporium, Aspergillus, Rhizopus, Microsporum, Purpureocillium, Paecilomyces and Trichophyton. back cover: the colours of Trichophyton spp. Descriptions of Medical Fungi iii PREFACE The first edition of this book entitled Descriptions of Medical QaP fungi was published in 1992 by David Ellis, Steve Davis, Helen alexiou, Tania Pfeiffer and Zabeta Manatakis. -

Table S1. Characteristics of Repurposed Drugs/Compounds for Control of Fungal Pathogens. 1 Compounds Original Functions Target F
Table S1. Characteristics of repurposed drugs/compounds for control of fungal pathogens. 1 Repurposing methods; Compounds Original functions Target fungi References cellular processes affected A. IN SILICO, COMPUTATIONAL Computational chemogenomics; Vistusertib, Anti-neoplastic drug Paracoccidioides species fungal phosphatidylinositol 3-kinase [15] BGT-226 candidates (TOR2) Candida albicans, Candida glabrata, Candida tropicalis, Candida dubliniensis, Candida parapsilosis, Aspergillus fumigatus, Aspergillus flavus, Rhizopus oryzae, Rhizopus microspores, Rhizomucor pusillus, Computational, Docking fluvastatin Rhizomucor miehei, Mucor racemosus, with cytochrome P450 (CYP51) Fluvastatin Anti-high cholesterol & [18,19] Mucor mucedo, Mucor circinelloides, model; triglycerides (blood) Absidia corymbifera, Absidia glauca, inhibition of growth and biofilm Trichophyton mentagrophytes, formation Trichophyton rubrum, Microsporum canis, Microsporum gypseum, Paecilomyces variotii, Syncephalastrum racemosum, Pythium insidiosum Ligand-based virtual screening, C. albicans, C. parapsilosis, Plant chorismate mutase homology modelling, molecular [16] Abscisic acid Aspergillus niger, inhibitor docking; T. rubrum, Trichophyton mentagrophytes chorismate mutase Homology modeling and molecular docking; P. insidiosum, Candida species, putative aldehyde dehydrogenase Disulfiram Treatment of alcoholism Cryptococcus species, A. fumigatus, [17,22] and urease activities, Histoplasma capsulatum bind/inactivate multiple proteins of P. insidiosum Raltegravir (MDDR, In -

Chromoblastomycosis Caused by Phialophora—Proven Cases from Mexico
Journal of Fungi Article Chromoblastomycosis Caused by Phialophora—Proven Cases from Mexico Sarah A. Ahmed 1,2,3 , Alexandro Bonifaz 4,* , Gloria M. González 5, Leandro F. Moreno 6, Nickolas Menezes da Silva 1,7,8, Vania A. Vicente 7, Ruoyu Li 9 and Sybren de Hoog 1,3,7,* 1 Center of Expertise in Mycology, Radboud University Medical Center/Canisius Wilhelmina Hospital, 6525GA Nijmegen, The Netherlands; [email protected] (S.A.A.); [email protected] (N.M.d.S.) 2 Faculty of Medical Laboratory Sciences, University of Khartoum, Khartoum 11115, Sudan 3 Foundation Atlas of Clinical Fungi, 1214GP Hilversum, The Netherlands 4 Hospital General de México, “Dr. Eduardo Liceaga”, Dr. Balmis 148, Doctores, 06720 Ciudad de México, Mexico 5 School of Medicine, Microbiology Department, Universidad Autónoma de Nuevo León, 64460 Monterrey, Mexico; [email protected] 6 Amsterdam Medical Center, 1105AZ Amsterdam, The Netherlands; [email protected] 7 Department of Basic Pathology, Federal University of Paraná State, Curitiba 81530-000, Brazil; [email protected] 8 Graduate Program in Bioprocess Engineering and Biotechnology, Federal University of Paraná, Curitiba 81530-000, Brazil 9 Department of Dermatology, Peking University First Hospital, Research Center for Medical Mycology, Peking University, Beijing 100034, China; [email protected] or [email protected] * Correspondence: [email protected] (A.B.); [email protected] (S.d.H.) Abstract: Chromoblastomycosis is a chronic severely mutilating disease caused by fungi of the order Chaetothyriales. Classically, Phialophora verrucosa has been listed among these etiologic agents. Citation: Ahmed, S.A.; Bonifaz, A.; This species is known to occur in the environment and has been found to cause other infections González, G.M.; Moreno, L.F.; like phaeohyphomycosis, while reported cases of chromoblastomycosis are scant. -

A New Species, Phialophora Europaea, Causing Superficial Infections In
MYCOSES 43, 409±416 (2000) ACCEPTED:MARCH 2, 2000 A new species, Phialophora europaea, causing super®cial infections in humans Eine neue Art, Phialophora europaea, als Erreger ober¯aÈchlicher Infektionen beim Menschen G. S. de Hoog1, P. Mayser2, G. Haase3, R. HorreÂ4 and A. M. Horrevorts5 Key words. Phialophora europaea, nova species, cutaneous infections, onychomycosis, ITS rDNA sequencing, physiology, diagnostics. SchluÈ sselwoÈrter. Phialophora europaea, nova species, Hautinfektion, Onychomykose, ITS rDNA-Sequenzierung, Physiologie, Diagnostik. Summary. A new species, Phialophora europaea, Menschen aus Nordwest Europa isoliert. Ein member of the P. verrucosa complex, is intro- BestimmungsschluÈssel fuÈr diese und morpholo- duced. It is distinguished from existing species gisch aÈhnliche Pilze wird zur VerfuÈgung gestellt. by reduced, ¯aring phialidic collarettes and inability to assimilate melibiose as sole source of carbon.AnalysisofITS1and2rDNAofsix strains attributed to the species show it to be Introduction clearly individualized. All strains originated from cutaneous and nail infections of humans in The genus Phialophora is characterized by mela- North-western Europe. A key to morphologically nized hyphae and by the production of slimy, similar taxa is provided. one-celled conidia in heads from phialides with distinct collarattes. The genus is polyphyletic, as it comprises species which belong to different Zusammenfassung. Wir beschreiben eine orders of the fungal kingdom [1]. neue Art, Phialophora europaea,innerhalbderP. Phialophora-like species causing infections of verrucosa-Gruppe. Diese Spezies ist durch redu- human skin are frequently referred to as Phialo- zierte, etwas fransige Collaretten der Phialiden phora verrucosa Medlar, which is one of the classi- gekennzeichnet und unfaÈhig, Melibiose als ein- cal agents of chromoblastomycosis.