ACMR16 21.Pdf (470.0Kb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Case Report of Tinea Nigra from North India
Letters to the Editor transepidermal elimination. Topical (retinoic acid, 12% lactic acid, 10% urea), mechanical (cauterization, curettage, dermabrasion, CO2 laser) and systemic (oral isotretinoin) treatment modalities are available.[1,5] AAyseyse SSeraperap KKaradag,aradag, EbruEbru CakCakõr1, AAylinylin PPelitlielitli Department of Dermatology, Ankara Kecioren Research and Training Hospital, 1Department of Pathology, Atatürk Chest Diseases and Thoracic Surgery Centre, Ankara, Turkey AAddressddress fforor correspondence:correspondence: Dr. Ayse Serap Karadag, Department of Dermatology, Ankara Kecioren Research and Training Hospital, Ankara, Turkey. E-mail: [email protected] DDOI:OI: 10.4103/0378-6323.55421 - PPMID:MID: ** Figure 1: Multiple, blue coloured, 1−3 mm sized vellus hair cysts localized on the anterolateral chest wall RREFERENCESEFERENCES 1. Reep MD, Robson KJ. Eruptive vellus hair cysts presenting as multiple periorbital papules in a 13-year-old boy. Pediatr Dermatol 2002;19:26-7. 2. Hong SD, Frieden IJ. Diagnosing eruptive vellus hair cysts. Pediatr Dermatol 2001;18:258-9. 3. Sárdy M, Kárpáti S. Needle evacuation of eruptive vellus hair cysts. Br J Dermatol 1999;141:594-5. 4. Strobos MA, Jonkman MF. Trichostasis spinulosa: itchy follicular papules in young adults. Int J Dermatol 2002;41: 643-6. 5. Kaya TI, Tataroglu C, Tursen U, Ikizoglu G. Eruptive vellus hair cysts: An effective extraction technique for treatment and diagnosis. J Eur Acad Dermatol Venereol 2006;20:264-8. Figure 2: Potassium hydroxide preparation showing numerous A ccasease rreporteport ooff ttineainea nnigraigra ffromrom vellus hairs in a serpentine array (magniÞ cation, X100) NNorthorth IIndiandia Sir, Tinea nigra is a rare superficial fungal infection of the skin. It is caused by Hortaea werneckii (formerly known as Phaeoannellomyces werneckii, Exophiala werneckii, and Cladosporium werneckii).[1] It occurs most frequently in tropical climates and presents as asymptomatic brown to black nonscaly macules with well-defined borders resembling silver nitrate stains. -

Mucormycosis of the Central Nervous System
Journal of Fungi Review Mucormycosis of the Central Nervous System 1 1,2, , 3, , Amanda Chikley , Ronen Ben-Ami * y and Dimitrios P Kontoyiannis * y 1 Infectious Diseases Unit, Tel Aviv Sourasky Medical Center, Tel Aviv 64239, Israel 2 Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 64239, Israel 3 Department of Infectious Diseases, The University of Texas, M.D. Anderson Cancer Center, Houston, TX 77030, USA * Correspondence: [email protected] (R.B.-A.); [email protected] (D.P.K.) These authors contribute equally to this paper. y Received: 6 June 2019; Accepted: 7 July 2019; Published: 8 July 2019 Abstract: Mucormycosis involves the central nervous system by direct extension from infected paranasal sinuses or hematogenous dissemination from the lungs. Incidence rates of this rare disease seem to be rising, with a shift from the rhino-orbital-cerebral syndrome typical of patients with diabetes mellitus and ketoacidosis, to disseminated disease in patients with hematological malignancies. We present our current understanding of the pathobiology, clinical features, and diagnostic and treatment strategies of cerebral mucormycosis. Despite advances in imaging and the availability of novel drugs, cerebral mucormycosis continues to be associated with high rates of death and disability. Emerging molecular diagnostics, advances in experimental systems and the establishment of large patient registries are key components of ongoing efforts to provide a timely diagnosis and effective treatment to patients with cerebral mucormycosis. Keywords: central nervous system; mucormycosis; Mucorales; zygomycosis 1. Introduction Mucormycosis is the second most frequent invasive mold disease after aspergillosis [1–3], with rising incidence reported in some countries [4–7]. -

Oral Antifungals Month/Year of Review: July 2015 Date of Last
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Class Update with New Drug Evaluation: Oral Antifungals Month/Year of Review: July 2015 Date of Last Review: March 2013 New Drug: isavuconazole (a.k.a. isavunconazonium sulfate) Brand Name (Manufacturer): Cresemba™ (Astellas Pharma US, Inc.) Current Status of PDL Class: See Appendix 1. Dossier Received: Yes1 Research Questions: Is there any new evidence of effectiveness or safety for oral antifungals since the last review that would change current PDL or prior authorization recommendations? Is there evidence of superior clinical cure rates or morbidity rates for invasive aspergillosis and invasive mucormycosis for isavuconazole over currently available oral antifungals? Is there evidence of superior safety or tolerability of isavuconazole over currently available oral antifungals? • Is there evidence of superior effectiveness or safety of isavuconazole for invasive aspergillosis and invasive mucormycosis in specific subpopulations? Conclusions: There is low level evidence that griseofulvin has lower mycological cure rates and higher relapse rates than terbinafine and itraconazole for adult 1 onychomycosis.2 There is high level evidence that terbinafine has more complete cure rates than itraconazole (55% vs. 26%) for adult onychomycosis caused by dermatophyte with similar discontinuation rates for both drugs.2 There is low -

Fungal Infections – an Overview
REVIEW Fungal infections – An overview Natalie Schellack, BCur, BPharm, PhD(Pharmacy); Jade du Toit, BPharm; Tumelo Mokoena, BPharm; Elmien Bronkhorst, BPharm, MSc(Med) School of Pharmacy, Faculty of Health Sciences, Sefako Makgatho Health Sciences University Correspondence to: Prof Natalie Schellack, [email protected] Abstract Fungi normally originate from the environment that surrounds us, and appear to be harmless until inhaled or ingestion of spores occurs. A pathogenic fungus may lead to infection. People who are at risk of acquiring fungal infection are those living with human immunodeficiency virus (HIV), cancer, receiving immunosuppressant therapy, neonates and those of advanced age. The management of superficial fungal infections is mainly topical, with agents including terbinafine, miconazole and ketoconazole. Oral treatment includes griseofulvin and fluconazole. Invasive fungal infections are difficult to treat, and are managed with agents including the azoles, echinocandins and amphotericin B. This paper provides a general overview of the management of fungus infections. © Medpharm S Afr Pharm J 2019;86(1):33-40 Introduction more advanced biochemical or molecular testing.4 Fungi normally originate from the environment that surrounds Superficial fungal infections us, and appear to be harmless until inhaled or ingestion of spores Either yeasts or fungi can cause dermatomycosis, or superficial occurs. Infection with fungi is also more likely when the body’s fungal infections.7 Fungi that infect the hair, skin, nails and mucosa immune system becomes weakened. A pathogenic fungus may lead to infection. The number of fungus species ranges in the can cause a superficial fungal infection. Dermatophytes are found millions and only a few species seem to be harmful to humans; the naturally in soil, human skin and keratin-containing structures, 3 ones found mostly on the mucous membrane and the skin have which provide them with a source of nutrition. -

Cryptococcosis in Cats
12 Cryptococcosis in cats FACT SHEET What is cryptococcosis? ! Atypical forms are characterized by one or more skin nodules that are not ! Cryptococcosis is the most common systemic fungal disease in cats worldwide. painful but may be firm or fluctuant. Solitary nodules are suggestive of direct inoculation. ! It is caused by the C. neoformans-C. gattii species complex which can also infect o Multiple nodules are suggestive of haematogenous spread from the primary humans, domestic and wild mammals and birds. o site of infection. ! C. neoformans is considered an opportunistic pathogen in human urban ! populations, whereas C. gattii is a true pathogen, more prevalent in rural areas. Haematogenous dissemination may lead to meningoencephalomyelitis, uveitis, chorioretinitis, osteomyelitis, polyarthritis, systemic lymphadenitis and multi- ! Cryptococcosis is a rare non-contagious fungal disease, acquired from a organ involvement. contaminated environment. ! CNS involvement may occur following local dissemination through the cribriform plate, causing sudden blindness, seizures and/or behavioural changes. ! Apathy and cachexia appear in chronic cases with systemic dissemination. Pathogenesis ! Cryptococcus is mainly an airborne pathogen, and basidiospores, which develop in the environment, penetrate the cat’s respiratory system and induce primary Diagnosis infection. ! Cutaneous inoculation or spread from the respiratory to the central nervous ! Cytology: samples stained with Romanowsky-type stains demonstrate pink to system (CNS) is also possible. violet, round or budding yeasts that vary in size (4-15 microns) and shape. They are typically surrounded by a clear, more or less thick halo corresponding to the ! The yeast cell survives inside phagocytic cells such as macrophages, dendritic unstained capsule. cells, and neutrophils, replicating both extracellularly and intracellularly. -

Clinical Diversity of Invasive Cryptococcosis in AIDS Patients
Zhang et al. BMC Infectious Diseases (2019) 19:1003 https://doi.org/10.1186/s12879-019-4634-7 CASE REPORT Open Access Clinical diversity of invasive cryptococcosis in AIDS patients from central China: report of two cases with review of literature Yongxi Zhang1, Brian Cooper2,Xi’en Gui1, Renslow Sherer2 and Qian Cao1* Abstract Background: Although antiretroviral therapy (ART) has greatly improved the prognosis of acquired immunodeficiency syndrome (AIDS) patients globally, opportunistic infections (OIs) are still common in Chinese AIDS patients, especially cryptococcosis. Case presentation: We described here two Chinese AIDS patients with cryptococcal infections. Case one was a fifty- year-old male. At admission, he was conscious and oriented, with papulonodular and umbilicated skin lesions, some with ulceration and central necrosis resembling molluscum contagiosum. The overall impression reminded us of talaromycosis: we therefore initiated empirical treatment with amphotericin B, even though the case history of this patient did not support such a diagnosis. On the second day of infusion, the patient complained of intermittent headache, but the brain CT revealed no abnormalities. On the third day, a lumbar puncture was performed. The cerebral spinal fluid (CSF) was turbid, with slightly increased pressure. India ink staining was positive, but the cryptococcus antigen latex agglutination test (CrAgLAT: IMMY, USA) was negative. Two days later, the blood culture showed a growth of Cryptococcus neoformans, and the same result came from the skin culture. We added fluconazole to the patient’s treatment, but unfortunately, he died three days later. Case two was a sixty-four-year-old female patient with mild fever, productive cough, dyspnea upon movement, and swelling in both lower limbs. -

Monograph on Dematiaceous Fungi
Monograph On Dematiaceous fungi A guide for description of dematiaceous fungi fungi of medical importance, diseases caused by them, diagnosis and treatment By Mohamed Refai and Heidy Abo El-Yazid Department of Microbiology, Faculty of Veterinary Medicine, Cairo University 2014 1 Preface The first time I saw cultures of dematiaceous fungi was in the laboratory of Prof. Seeliger in Bonn, 1962, when I attended a practical course on moulds for one week. Then I handled myself several cultures of black fungi, as contaminants in Mycology Laboratory of Prof. Rieth, 1963-1964, in Hamburg. When I visited Prof. DE Varies in Baarn, 1963. I was fascinated by the tremendous number of moulds in the Centraalbureau voor Schimmelcultures, Baarn, Netherlands. On the other hand, I was proud, that El-Sheikh Mahgoub, a Colleague from Sundan, wrote an internationally well-known book on mycetoma. I have never seen cases of dematiaceous fungal infections in Egypt, therefore, I was very happy, when I saw the collection of mycetoma cases reported in Egypt by the eminent Egyptian Mycologist, Prof. Dr Mohamed Taha, Zagazig University. To all these prominent mycologists I dedicate this monograph. Prof. Dr. Mohamed Refai, 1.5.2014 Heinz Seeliger Heinz Rieth Gerard de Vries, El-Sheikh Mahgoub Mohamed Taha 2 Contents 1. Introduction 4 2. 30. The genus Rhinocladiella 83 2. Description of dematiaceous 6 2. 31. The genus Scedosporium 86 fungi 2. 1. The genus Alternaria 6 2. 32. The genus Scytalidium 89 2.2. The genus Aurobasidium 11 2.33. The genus Stachybotrys 91 2.3. The genus Bipolaris 16 2. -

Valley Fever a K a Coccidioidomycosis Coccidioidosis Coccidiodal Granuloma San Joaquin Valley Fever Desert Rheumatism Valley Bumps Cocci Cox C
2019 Lung Infection Symposium - Libke 10/26/2019 58 YO ♂ • 1974 PRESENTED WITH HEADACHE – DX = COCCI MENINGITIS WITH HYDROCEPHALUS – Rx = IV AMPHOTERICIN X 6 WKS – VP SHUNT – INTRACISTERNAL AMPHO B X 2.5 YRS (>200 PUNCTURES) • 1978 – 2011 VP SHUNT REVISIONS X 5 • 1974 – 2019 GAINFULLY EMPLOYED, RAISED FAMILY, RETIRED AND CALLS OCCASIONALLY TO SEE HOW I’M DOING. VALLEY FEVER A K A COCCIDIOIDOMYCOSIS COCCIDIOIDOSIS COCCIDIODAL GRANULOMA SAN JOAQUIN VALLEY FEVER DESERT RHEUMATISM VALLEY BUMPS COCCI COX C 1 2019 Lung Infection Symposium - Libke 10/26/2019 COCCIDIOIDOMYCOSIS • DISEASE FIRST DESCRIBED IN 1892 – POSADAS –ARGENTINA – RIXFORD & GILCHRIST - CALIFORNIA – INITIALLY THOUGHT PARASITE – RESEMBLED COCCIDIA “COCCIDIOIDES” – “IMMITIS” = NOT MINOR COCCIDIOIDOMYCOSIS • 1900 ORGANISM IDENTIFIED AS FUNGUS – OPHULS AND MOFFITT – ORGANISM CULTURED FROM TISSUES OF PATIENT – LIFE CYCLE DEFINED – FULFULLED KOCH’S POSTULATES 2 2019 Lung Infection Symposium - Libke 10/26/2019 COCCIDIOIDOMYCOSIS • 1932 ORGANISM IN SOIL SAMPLE FROM DELANO – UNDER BUNKHOUSE OF 4 PATIENTS – DISEASE FATAL • 1937 DICKSON & GIFFORD CONNECTED “VALLEY FEVER” TO C. IMMITIS – USUALLY SELF LIMITED – FREQUENTLY SEEN IN SAN JOAQUIN VALLEY – RESPIRATORY TRACT THE PORTAL OF ENTRY The usual cause for coccidioidomycosis in Arizona is C. immitis A. True B. False 3 2019 Lung Infection Symposium - Libke 10/26/2019 COCCIDIOIDAL SPECIES • COCCIDIOIDES IMMITIS – CALIFORNIA • COCCIDIOIDES POSADASII – NON-CALIFORNIA • ARIZONA, MEXICO • OVERLAP IN SAN DIEGO AREA THE MICROBIAL WORLD • PRIONS -

Prostatic Cryptococcosis - a Case Report
Received: November 8, 2007 J. Venom. Anim. Toxins incl. Trop. Dis. Accepted: April 1, 2008 V.14, n.2, p.378-385, 2008. Abstract published online: April 2, 2008 Case report. Full paper published online: May 31, 2008 ISSN 1678-9199. PROSTATIC CRYPTOCOCCOSIS - A CASE REPORT CHANG M. R. (1), PANIAGO A. M. M. (2), SILVA M. M. (3), LAZÉRA M. S. (4), WANKE B. (4) (1) Department of Pharmacy-Biochemistry, Federal University of Mato Grosso do Sul (UFMS), Campo Grande, Mato Grosso do Sul State, Brazil; (2) Department of Internal Medicine, UFMS, Campo Grande, Mato Grosso do Sul State, Brazil; (3) Medicine Program, University for Development of the State and the Pantanal Region (UNIDERP), Campo Grande, Mato Grosso do Sul State, Brazil; (4) Mycology Service Evandro Chagas Institute of Clinical Research (IPEC), Oswaldo Cruz Foundation (FIOCRUZ), Rio de Janeiro, Rio de Janeiro State, Brazil. ABSTRACT: Cryptococcosis is a systemic mycosis usually affecting immunodeficient individuals. In contrast, immunologically competent patients are rarely affected. Dissemination of cryptococcosis usually involves the central nervous system, manifesting as meningitis or meningoencephalitis. Prostatic lesions are not commonly found. A case of prostate cryptococcal infection is presented and cases of prostatic cryptococcosis in normal and immunocompromised hosts are reviewed. A fifty-year-old HIV-negative man with urinary retention and renal insufficiency underwent prostatectomy due to massive enlargement of the organ. Prostate histopathologic examination revealed encapsulated yeast-like structures. After 30 days, the patient’s clinical manifestations worsened, with headache, neck stiffness, bradypsychia, vomiting and fever. Direct microscopy of the patient’s urine with China ink preparations showed capsulated yeasts, and positive culture yielded Cryptococcus neoformans. -

Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm)
Editorial | Journal of Gandaki Medical College-Nepal Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm) Reddy KR Professor & Head Microbiology Department Gandaki Medical College & Teaching Hospital, Pokhara, Nepal Medical Mycology, a study of fungal epidemiology, ecology, pathogenesis, diagnosis, prevention and treatment in human beings, is a newly recognized discipline of biomedical sciences, advancing rapidly. Earlier, the fungi were believed to be mere contaminants, commensals or nonpathogenic agents but now these are commonly recognized as medically relevant organisms causing potentially fatal diseases. The discipline of medical mycology attained recognition as an independent medical speciality in the world sciences in 1910 when French dermatologist Journal of Raymond Jacques Adrien Sabouraud (1864 - 1936) published his seminal treatise Les Teignes. This monumental work was a comprehensive account of most of then GANDAKI known dermatophytes, which is still being referred by the mycologists. Thus he MEDICAL referred as the “Father of Medical Mycology”. COLLEGE- has laid down the foundation of the field of Medical Mycology. He has been aptly There are significant developments in treatment modalities of fungal infections NEPAL antifungal agent available. Nystatin was discovered in 1951 and subsequently and we have achieved new prospects. However, till 1950s there was no specific (J-GMC-N) amphotericin B was introduced in 1957 and was sanctioned for treatment of human beings. In the 1970s, the field was dominated by the azole derivatives. J-GMC-N | Volume 10 | Issue 01 developed to treat fungal infections. By the end of the 20th century, the fungi have Now this is the most active field of interest, where potential drugs are being January-June 2017 been reported to be developing drug resistance, especially among yeasts. -
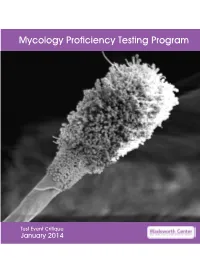
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Pulmonary Cryptococcosis Secondary To
& My gy co lo lo ro g i y V Ramana et al., Virol Mycol 2012, 1:3 Virology & Mycology DOI: 10.4172/2161-0517.1000107 ISSN: 2161-0517 Case Report Open Access Pulmonary Cryptococcosis Secondary to Bronchial Asthma Presenting as Type I Respiratory Failure- A Case Report with Review of Literature KV Ramana*, Moses Vinay Kumar, Sanjeev D Rao, Akhila R, Sandhya, Shruthi P, Pranuthi M, Krishnappa M, Anand K Department of Microbiology, Prathima Inst of Medical Sciences, Nagunur, Karimnagar, Andhrapradesh, India Introduction mellitus, pleuritis, systemic lupus erythematus, cushings syndrome, Continous Ambulatory Peritoneal Dialysis (CAPD), liver cirrhosis, Cryptococcus spp, was first isolated and described in 1894 by cancer, organ transplants, spleenectomy, malnutrition, leprosy, Sanfelice F in Italy from peach juice and named it as Saccharomyces pulmonary tuberculosis and those on cortico steroid therapy [13-20]. neoformans, is an yeast like fungus [1], first isolated from a clinical Pulmonary Cryptococcosis may be presenting as pleural effusions, specimen by Busse in the same year from Germany [2]. Cryptococci solitary or multiple masses, glass-ground interstitial opacities, dense are a saprophytic fungi present in soil contaminated with bird consolidations, patchy, segmented or lobar air space consolidation droppings mainly of pigeons, roosting sites and decaying vegetables (cryptococcal pneumonia) and nodular and reticulonodular cavities. [3]. Previous reports have also showed the presence of Cryptococcus Differential diagnosis of pulmonary cryptococcosis should be done spp colonized in the nasopharynx and on skin of healthy individuals with pneumonia [21,22]. Review of literature showed only two previous [4]. Belonging to Basidiomyctes group of fungi Cryptococcus spp reported cases of pulmonary cryptococcosis presenting as acute primarily infects central nervous system causing meningoencephalitis respiratory failure [7,23,24].