Client Services Manual Public Health Laboratory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -
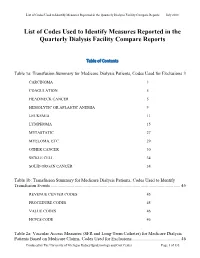
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -

Specimen Type, Collection Methods, and Diagnostic Assays Available For
Specimen type, collection methods, and diagnostic assays available for the detection of poxviruses from human specimens by the Poxvirus and Rabies Branch, Centers for Disease Control and Prevention1. Specimen Orthopoxvirus Parapoxvirus Yatapoxvirus Molluscipoxvirus Specimen type collection method PCR6 Culture EM8 IHC9,10 Serology11 PCR12 EM8 IHC9,10 PCR13 EM8 PCR EM8 Lesion material Fresh or frozen Swab 5 Lesion material [dry or in media ] [vesicle / pustule Formalin fixed skin, scab / crust, etc.] Paraffin block Fixed slide(s) Container Lesion fluid Swab [vesicle / pustule [dry or in media5] fluid, etc.] Touch prep slide Blood EDTA2 EDTA tube 7 Spun or aliquoted Serum before shipment Spun or aliquoted Plasma before shipment CSF3,4 Sterile 1. The detection of poxviruses by electron microscopy (EM) and immunohistochemical staining (IHC) is performed by the Infectious Disease Pathology Branch of the CDC. 2. EDTA — Ethylenediaminetetraacetic acid. 3. CSF — Cerebrospinal fluid. 4. In order to accurately interpret test results generated from CSF specimens, paired serum must also be submitted. 5. If media is used to store and transport specimens a minimal amount should be used to ensure as little dilution of DNA as possible. 6. Orthopoxvirus generic real-time polymerase chain reaction (PCR) assays will amplify DNA from numerous species of virus within the Orthopoxvirus genus. Species-specific real-time PCR assays are available for selective detection of DNA from variola virus, vaccinia virus, monkeypox virus, and cowpox virus. 7. Blood is not ideal for the detection of orthopoxviruses by PCR as the period of viremia has often passed before sampling occurs. 8. EM can reveal the presence of a poxvirus in clinical specimens or from virus culture, but this technique cannot differentiate between virus species within the same genus. -

Supporting Information
Supporting Information Rosenberg et al. 10.1073/pnas.1307243110 SI Results and Discussion domestic ungulates (horses, cows, sheep, goats, camels, and pigs) Of the 83 arboviruses, nonhuman vertebrate hosts have been and rodents in both groups might be a consequence of spatial identified for 70 (84%); the remaining 13 are presumed to be proximity to humans. Sentinel monkeys were often used in pro- zoonoses because there is no indication they can be transmitted cedures to isolate arboviruses, which might account for their directly between humans by vectors (Table S1). Animal hosts have higher representation among arboviruses. In contrast, there are been identified for at least 57 (44%) of the 130 nonarboviruses; an few published records of bats being routinely sampled during additional 5 (8%) are presumed on epidemiological evidence to arbovirus studies, and only two arboviruses (3%) have been iso- have nonhuman reservoirs (Table S1). A number of viruses infect lated from bats. The reason a much larger number of arbovirus more than one nonhuman vertebrate host species and it is likely species (n = 16) have been isolated from birds than have that the variety of hosts is wider than has been recorded. The nonarbovirus species (n = 1) might, however, be characteristic of predominant host groups for arboviruses (n = 70) are nonhuman the pathogenicity of the togaviruses and flaviviruses, which are primates (31%), rodents (29%), ungulates (26%), and birds (23%); much more common among the arboviruses. The most prominent for the nonarboviruses (n = 57), they are rodents (30%), ungu- vectors of arboviruses were mosquitoes (67%), ticks (19%), and lates (26%), bats (23%), and primates (16%). -

Document-1.Pdf (100.7Kb)
JOURNAL OF VIROLOGY, Jan. 2004, p. 168–177 Vol. 78, No. 1 0022-538X/04/$08.00ϩ0 DOI: 10.1128/JVI.78.1.168–177.2004 Copyright © 2004, American Society for Microbiology. All Rights Reserved. Genomes of the Parapoxviruses Orf Virus and Bovine Papular Stomatitis Virus G. Delhon,1,2 E. R. Tulman,1 C. L. Afonso,1 Z. Lu,1 A. de la Concha-Bermejillo,3 H. D. Lehmkuhl,4 M. E. Piccone,1 G. F. Kutish,1 and D. L. Rock1* Plum Island Animal Disease Center, Agricultural Research Service, United States Department of Agriculture, Greenport, New York 119441; Area of Virology, School of Veterinary Sciences, University of Buenos Aires, 1427 Buenos Aires, Argentina2; Department of Veterinary Pathobiology, College of Veterinary Medicine, Texas A&M University, College Station, Texas 77843-44673; and National Animal Disease Center, Agricultural Research Service, United States Department of Agriculture, Downloaded from Ames, Iowa 500104 Received 19 August 2003/Accepted 22 September 2003 Bovine papular stomatitis virus (BPSV) and orf virus (ORFV), members of the genus Parapoxvirus of the Poxviridae, are etiologic agents of worldwide diseases affecting cattle and small ruminants, respectively. Here we report the genomic sequences and comparative analysis of BPSV strain BV-AR02 and ORFV strains OV-SA00, isolated from a goat, and OV-IA82, isolated from a sheep. Parapoxvirus (PPV) BV-AR02, OV-SA00, .and OV-IA82 genomes range in size from 134 to 139 kbp, with an average nucleotide composition of 64% G؉C BPSV and ORFV genomes contain 131 and 130 putative genes, respectively, and share colinearity over 127 http://jvi.asm.org/ genes, 88 of which are conserved in all characterized chordopoxviruses. -

INFECTIOUS DISEASES of HAITI Free
INFECTIOUS DISEASES OF HAITI Free. Promotional use only - not for resale. Infectious Diseases of Haiti - 2010 edition Infectious Diseases of Haiti - 2010 edition Copyright © 2010 by GIDEON Informatics, Inc. All rights reserved. Published by GIDEON Informatics, Inc, Los Angeles, California, USA. www.gideononline.com Cover design by GIDEON Informatics, Inc No part of this book may be reproduced or transmitted in any form or by any means without written permission from the publisher. Contact GIDEON Informatics at [email protected]. ISBN-13: 978-1-61755-090-4 ISBN-10: 1-61755-090-6 Visit http://www.gideononline.com/ebooks/ for the up to date list of GIDEON ebooks. DISCLAIMER: Publisher assumes no liability to patients with respect to the actions of physicians, health care facilities and other users, and is not responsible for any injury, death or damage resulting from the use, misuse or interpretation of information obtained through this book. Therapeutic options listed are limited to published studies and reviews. Therapy should not be undertaken without a thorough assessment of the indications, contraindications and side effects of any prospective drug or intervention. Furthermore, the data for the book are largely derived from incidence and prevalence statistics whose accuracy will vary widely for individual diseases and countries. Changes in endemicity, incidence, and drugs of choice may occur. The list of drugs, infectious diseases and even country names will vary with time. © 2010 GIDEON Informatics, Inc. www.gideononline.com All Rights Reserved. Page 2 of 314 Free. Promotional use only - not for resale. Infectious Diseases of Haiti - 2010 edition Introduction: The GIDEON e-book series Infectious Diseases of Haiti is one in a series of GIDEON ebooks which summarize the status of individual infectious diseases, in every country of the world. -

Discovery of Antivirals Against Smallpox
Discovery of antivirals against smallpox Stephen C. Harrisona,b, Bruce Albertsc, Ellie Ehrenfeldd, Lynn Enquiste, Harvey Finebergf, Steven L. McKnightg, Bernard Mossh, Michael O’Donnelli, Hidde Ploeghj, Sandra L. Schmidk, K. Peter Walterl, and Julie Theriotm aHarvard Medical School, Howard Hughes Medical Institute, Seeley Mudd Building, Room 130, 250 Longwood Avenue, Boston, MA 02115; cNational Academy of Sciences, 2101 Constitution Avenue, NW, Washington, DC 20418; dLaboratory of Infectious Disease, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Building 50, Room 6120, 50 South Drive, Bethesda, MD 20892; ePrinceton University, 314 Schultz Laboratory, Washington Road, Princeton, NJ 08544; fInstitute of Medicine, 2101 Constitution Avenue, NW, Washington, DC 20418; gDepartment of Biochemistry, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390; hLaboratory of Viral Diseases, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Building 4, Room 229, 4 Center Drive, Bethesda, MD 20892; iLaboratory of DNA Replication, The Rockefeller University, Howard Hughes Medical Institute, 1230 York Avenue, New York, NY 10021; jDepartment of Pathology, Harvard Medical School, NRB, 77 Avenue Louis Pasteur, Boston, MA 02115; kDepartment of Cell Biology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, CA 92037; lDepartment of Biochemistry and Biophysics, University of California School of Medicine, Howard Hughes Medical Institute, Box 0448, HSE 1001, San Francisco, CA 94143; and mDepartment of Biochemistry, Stanford University School of Medicine, Stanford, CA 94305 Contributed by Stephen C. Harrison, May 21, 2004 mallpox, a devastating infectious Whatever the likelihood of covertly dopoxviruses has a restricted and spe- disease dreaded throughout much held variola virus stocks, an intentional cific host array (Table 2). -

Zoonotic Poxviruses Associated with Companion Animals
Animals 2011, 1, 377-395; doi:10.3390/ani1040377 OPEN ACCESS animals ISSN 2076-2615 www.mdpi.com/journal/animals Review Zoonotic Poxviruses Associated with Companion Animals Danielle M. Tack 1,2,* and Mary G. Reynolds 2 1 Epidemic Intelligence Service, Centers for Disease Control and Prevention, Atlanta, GA 30333, USA 2 Poxvirus and Rabies Branch, Centers for Disease Control and Prevention, Atlanta, GA 30333, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-404-639-5278. Received: 13 October 2011; in revised form: 2 November 2011 / Accepted: 15 November 2011 / Published: 17 November 2011 Simple Summary: Contemporary enthusiasm for the ownership of exotic animals and hobby livestock has created an opportunity for the movement of poxviruses—such as monkeypox, cowpox, and orf—outside their traditional geographic range bringing them into contact with atypical animal hosts and groups of people not normally considered at risk. It is important that pet owners and practitioners of human and animal medicine develop a heightened awareness for poxvirus infections and understand the risks that can be associated with companion animals and livestock. This article reviews the epidemiology and clinical features of zoonotic poxviruses that are most likely to affect companion animals. Abstract: Understanding the zoonotic risk posed by poxviruses in companion animals is important for protecting both human and animal health. The outbreak of monkeypox in the United States, as well as current reports of cowpox in Europe, point to the fact that companion animals are increasingly serving as sources of poxvirus transmission to people. -

Infectious Diseases of the Dominican Republic
INFECTIOUS DISEASES OF THE DOMINICAN REPUBLIC Stephen Berger, MD 2018 Edition Infectious Diseases of the Dominican Republic Copyright Infectious Diseases of the Dominican Republic - 2018 edition Stephen Berger, MD Copyright © 2018 by GIDEON Informatics, Inc. All rights reserved. Published by GIDEON Informatics, Inc, Los Angeles, California, USA. www.gideononline.com Cover design by GIDEON Informatics, Inc No part of this book may be reproduced or transmitted in any form or by any means without written permission from the publisher. Contact GIDEON Informatics at [email protected]. ISBN: 978-1-4988-1759-2 Visit www.gideononline.com/ebooks/ for the up to date list of GIDEON ebooks. DISCLAIMER Publisher assumes no liability to patients with respect to the actions of physicians, health care facilities and other users, and is not responsible for any injury, death or damage resulting from the use, misuse or interpretation of information obtained through this book. Therapeutic options listed are limited to published studies and reviews. Therapy should not be undertaken without a thorough assessment of the indications, contraindications and side effects of any prospective drug or intervention. Furthermore, the data for the book are largely derived from incidence and prevalence statistics whose accuracy will vary widely for individual diseases and countries. Changes in endemicity, incidence, and drugs of choice may occur. The list of drugs, infectious diseases and even country names will vary with time. Scope of Content Disease designations may reflect a specific pathogen (ie, Adenovirus infection), generic pathology (Pneumonia - bacterial) or etiologic grouping (Coltiviruses - Old world). Such classification reflects the clinical approach to disease allocation in the Infectious Diseases Module of the GIDEON web application. -

Report for the Hemodialysis Vascular Access: Standardized Fistula Rate
ESRD Quality Measure Development, Maintenance, and Support Contract Number HHSM-500-2013-13017I Report for the Hemodialysis Vascular Access: Standardized Fistula Rate (SFR) NQF #2977 Submitted to CMS by the University of Michigan Kidney Epidemiology and Cost Center June 21, 2017 Produced by UM-KECC Submitted: 6.21.2017 1 ESRD Quality Measure Development, Maintenance, and Support Contract Number HHSM-500-2013-13017I Table of Contents Introduction .................................................................................................................................................. 3 Methods ........................................................................................................................................................ 3 Overview ................................................................................................................................................... 3 Data Sources ............................................................................................................................................. 4 Outcome Definition .................................................................................................................................. 4 Denominator Definition ............................................................................................................................ 5 Risk Adjustment ........................................................................................................................................ 5 Choosing Adjustment Factors -

POXVIRUS INFECTIONS in NORTH AMERICAN PINNIPEDS By
POXVIRUS INFECTIONS IN NORTH AMERICAN PINNIPEDS By HENDRIK HANS NOLLENS A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2005 Copyright 2005 by Hendrik Hans Nollens ACKNOWLEDGMENTS Funding for this work was provided in part by the UF College of Veterinary Medicine Batchelor Foundation, by a grant from the Florida Fish and Wildlife Conservation Commission, and by John H. Prescott Marine Mammal Rescue Assistance grant number NA03NMF4390410 to E.J. All samples were collected under NMFS Scientific Research Permit nos. 932-1489-00 and 1054-1731-00. Sample collection protocols were approved by the University of Florida Institutional Animal Care and Use Committee (IACUC C403). I would like to thank the staff at The Marine Mammal Center (CA), the Marine Mammal Stranding Center (NJ), Animal Health Center (British Columbia), Mystic Aquarium (CT), Sea World of Orlando (FL), SeaWorld of San Diego (CA) and the Virginia Marine Science Museum (VA) for their participation in this study. I thank Dr. John Wise and Dr. Carie Goertz at the Wise Laboratory of Environmental and Genetic Toxicology, University of Southern Maine, for supplying the seal and sea lion cell cultures. Dr. Andy Mercer of the University of Otago, New Zealand, was very generous with his advice on virus isolation and interpretation of electron microscopy images. Dr. Robert DeLong of the National Marine Mammal Lab, Seattle WA, kindly provided me with sera from free-ranging sea lions. The cidofovir was provided by Chimerix, La Jolla CA. -

GOVE1RNMENT of the DISTRICT of COLUMBIA Department of Health Care Finance * * *
GOVE1RNMENT OF THE DISTRICT OF COLUMBIA Department of Health Care Finance * * * Office of the Deputy Director DHCF Transmittal #11-36 TO: Hospital Providers FR: Linda Elam, Ph.D., MP Deputy Director - Medi id Director DT: December 19, 2011 RE: Hospital Room (ER) Diagnosis Indicators The purpose of this Transmittal is to provide notice of updated emergency room (ER) code indicators, effective January 1, 2012. DHCF's analysis of ER indicator codes encompasses codes from 10/1/2006 forward. ICD-9-CM diagnosis codes that will be eligible for payment at the increased payment rate for emergency services are listed in the attached table. For more information, please contact Benjamin Finder, Director of the Division of Research, Analysis and Rate Setting at 202-724-4029 or email: [email protected]. Attaclunent 825 North Capitol Street, N.E., Washington, D.C. 20002 (202) 442-5988 Fax (202) 442-4790 Diagnosis Diagnosis Code Short Description Code Short Description 038.12 MRSA septicemia 200.37 Margin zone lymph spleen 040.41 Infant botulism 200.38 Margin zone lymph muttip 040.42 Wound botulism 200.40 Mantle cell lyrn xtrrndl 041.12 MRSA elsewhere/NOS 200A1 Mantle cell hrmph head 046.11 Varnt Creutzfeldt-Jakob 200.42 Mantle cell lymph thorax 046.19 Creutztidt-Jalcob NEC/NOS 200A3 Mantle cell lymph abdom 046.71 Gerstmn-Straus-Schnk syn 200.44 Mantle cell lymph axilla 046.72 Fatal Jambi insomnia 200A5 Mantle cell lymph inguin 046.79 Non dis of CNS NEC/NOS 200.46 Mantle cell lymph petec 051.01 Cowpox 200.47 Mantle cell lymph spleen 051.02 Vaccinia