Supporting Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Illness Caused by E. Coli O157:H7 from Food and Non-Food Sources
FRI BRIEFINGS Human Illness Caused by E. coli O157:H7 from Food and Non-food Sources M. Ellin Doyle1*, John Archer2, Charles W. Kaspar1, and Ronald Weiss1 1Food Research Institute, University of Wisconsin–Madison, Madison, WI 53706 2Wisconsin Division of Public Health, Bureau of Communicable Diseases and Preparedness, Communicable Disease Epidemiology Section, Madison, WI 53702 Contents Introduction ...................................................................................................................................2 Epidemiology of E. coli O157:H7..................................................................................................2 Outbreak Data ........................................................................................................................2 Reservoirs of E. coli O157:H7 ..............................................................................................3 Cattle—the primary reservoir ........................................................................................3 Other ruminants .............................................................................................................4 Other animals .................................................................................................................4 Transport Hosts......................................................................................................................4 Routes of Human Infection ....................................................................................................5 -

Guide for Common Viral Diseases of Animals in Louisiana
Sampling and Testing Guide for Common Viral Diseases of Animals in Louisiana Please click on the species of interest: Cattle Deer and Small Ruminants The Louisiana Animal Swine Disease Diagnostic Horses Laboratory Dogs A service unit of the LSU School of Veterinary Medicine Adapted from Murphy, F.A., et al, Veterinary Virology, 3rd ed. Cats Academic Press, 1999. Compiled by Rob Poston Multi-species: Rabiesvirus DCN LADDL Guide for Common Viral Diseases v. B2 1 Cattle Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 2 Deer and Small Ruminants Please click on the principle system involvement Generalized viral disease Respiratory viral disease Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 3 Swine Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 4 Horses Please click on the principle system involvement Generalized viral diseases Neurological viral diseases Respiratory viral diseases Enteric viral diseases Abortifacient/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 5 Dogs Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. -

How Do Pathogenic Microorganisms Develop Cross-Kingdom Host Jumps? Peter Van Baarlen1, Alex Van Belkum2, Richard C
Molecular mechanisms of pathogenicity: how do pathogenic microorganisms develop cross-kingdom host jumps? Peter van Baarlen1, Alex van Belkum2, Richard C. Summerbell3, Pedro W. Crous3 & Bart P.H.J. Thomma1 1Laboratory of Phytopathology, Wageningen University, Wageningen, The Netherlands; 2Department of Medical Microbiology and Infectious Diseases, Erasmus MC, University Medical Centre Rotterdam, Rotterdam, The Netherlands; and 3CBS Fungal Biodiversity Centre, Utrecht, The Netherlands Correspondence: Bart P.H.J. Thomma, Abstract Downloaded from https://academic.oup.com/femsre/article/31/3/239/2367343 by guest on 27 September 2021 Laboratory of Phytopathology, Wageningen University, Binnenhaven 5, 6709 PD It is common knowledge that pathogenic viruses can change hosts, with avian Wageningen, The Netherlands. Tel.: 10031 influenza, the HIV, and the causal agent of variant Creutzfeldt–Jacob encephalitis 317 484536; fax: 10031 317 483412; as well-known examples. Less well known, however, is that host jumps also occur e-mail: [email protected] with more complex pathogenic microorganisms such as bacteria and fungi. In extreme cases, these host jumps even cross kingdom of life barriers. A number of Received 3 July 2006; revised 22 December requirements need to be met to enable a microorganism to cross such kingdom 2006; accepted 23 December 2006. barriers. Potential cross-kingdom pathogenic microorganisms must be able to First published online 26 February 2007. come into close and frequent contact with potential hosts, and must be able to overcome or evade host defences. Reproduction on, in, or near the new host will DOI:10.1111/j.1574-6976.2007.00065.x ensure the transmission or release of successful genotypes. -

Generic Amplification and Next Generation Sequencing Reveal
Dinçer et al. Parasites & Vectors (2017) 10:335 DOI 10.1186/s13071-017-2279-1 RESEARCH Open Access Generic amplification and next generation sequencing reveal Crimean-Congo hemorrhagic fever virus AP92-like strain and distinct tick phleboviruses in Anatolia, Turkey Ender Dinçer1†, Annika Brinkmann2†, Olcay Hekimoğlu3, Sabri Hacıoğlu4, Katalin Földes4, Zeynep Karapınar5, Pelin Fatoş Polat6, Bekir Oğuz5, Özlem Orunç Kılınç7, Peter Hagedorn2, Nurdan Özer3, Aykut Özkul4, Andreas Nitsche2 and Koray Ergünay2,8* Abstract Background: Ticks are involved with the transmission of several viruses with significant health impact. As incidences of tick-borne viral infections are rising, several novel and divergent tick- associated viruses have recently been documented to exist and circulate worldwide. This study was performed as a cross-sectional screening for all major tick-borne viruses in several regions in Turkey. Next generation sequencing (NGS) was employed for virus genome characterization. Ticks were collected at 43 locations in 14 provinces across the Aegean, Thrace, Mediterranean, Black Sea, central, southern and eastern regions of Anatolia during 2014–2016. Following morphological identification, ticks were pooled and analysed via generic nucleic acid amplification of the viruses belonging to the genera Flavivirus, Nairovirus and Phlebovirus of the families Flaviviridae and Bunyaviridae, followed by sequencing and NGS in selected specimens. Results: A total of 814 specimens, comprising 13 tick species, were collected and evaluated in 187 pools. Nairovirus and phlebovirus assays were positive in 6 (3.2%) and 48 (25.6%) pools. All nairovirus sequences were closely-related to the Crimean-Congo hemorrhagic fever virus (CCHFV) strain AP92 and formed a phylogenetically distinct cluster among related strains. -

2020 Taxonomic Update for Phylum Negarnaviricota (Riboviria: Orthornavirae), Including the Large Orders Bunyavirales and Mononegavirales
Archives of Virology https://doi.org/10.1007/s00705-020-04731-2 VIROLOGY DIVISION NEWS 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales Jens H. Kuhn1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Gaya K. Amarasinghe5 · Simon J. Anthony6,7 · Tatjana Avšič‑Županc8 · María A. Ayllón9,10 · Justin Bahl11 · Anne Balkema‑Buschmann12 · Matthew J. Ballinger13 · Tomáš Bartonička14 · Christopher Basler15 · Sina Bavari16 · Martin Beer17 · Dennis A. Bente18 · Éric Bergeron19 · Brian H. Bird20 · Carol Blair21 · Kim R. Blasdell22 · Steven B. Bradfute23 · Rachel Breyta24 · Thomas Briese25 · Paul A. Brown26 · Ursula J. Buchholz27 · Michael J. Buchmeier28 · Alexander Bukreyev18,29 · Felicity Burt30 · Nihal Buzkan31 · Charles H. Calisher32 · Mengji Cao33,34 · Inmaculada Casas35 · John Chamberlain36 · Kartik Chandran37 · Rémi N. Charrel38 · Biao Chen39 · Michela Chiumenti40 · Il‑Ryong Choi41 · J. Christopher S. Clegg42 · Ian Crozier43 · John V. da Graça44 · Elena Dal Bó45 · Alberto M. R. Dávila46 · Juan Carlos de la Torre47 · Xavier de Lamballerie38 · Rik L. de Swart48 · Patrick L. Di Bello49 · Nicholas Di Paola50 · Francesco Di Serio40 · Ralf G. Dietzgen51 · Michele Digiaro52 · Valerian V. Dolja53 · Olga Dolnik54 · Michael A. Drebot55 · Jan Felix Drexler56 · Ralf Dürrwald57 · Lucie Dufkova58 · William G. Dundon59 · W. Paul Duprex60 · John M. Dye50 · Andrew J. Easton61 · Hideki Ebihara62 · Toufc Elbeaino63 · Koray Ergünay64 · Jorlan Fernandes195 · Anthony R. Fooks65 · Pierre B. H. Formenty66 · Leonie F. Forth17 · Ron A. M. Fouchier48 · Juliana Freitas‑Astúa67 · Selma Gago‑Zachert68,69 · George Fú Gāo70 · María Laura García71 · Adolfo García‑Sastre72 · Aura R. Garrison50 · Aiah Gbakima73 · Tracey Goldstein74 · Jean‑Paul J. Gonzalez75,76 · Anthony Grifths77 · Martin H. Groschup12 · Stephan Günther78 · Alexandro Guterres195 · Roy A. -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

Rapid Identification of Known and New RNA Viruses from Animal Tissues
Rapid Identification of Known and New RNA Viruses from Animal Tissues Joseph G. Victoria1,2*, Amit Kapoor1,2, Kent Dupuis3, David P. Schnurr3, Eric L. Delwart1,2 1 Department of Molecular Virology, Blood Systems Research Institute, San Francisco, California, United States of America, 2 Department of Laboratory Medicine, University of California, San Francisco, California, United States of America, 3 Viral and Rickettsial Disease Laboratory, Division of Communicable Disease Control, California State Department of Public Health, Richmond, California, United States of America Abstract Viral surveillance programs or diagnostic labs occasionally obtain infectious samples that fail to be typed by available cell culture, serological, or nucleic acid tests. Five such samples, originating from insect pools, skunk brain, human feces and sewer effluent, collected between 1955 and 1980, resulted in pathology when inoculated into suckling mice. In this study, sequence-independent amplification of partially purified viral nucleic acids and small scale shotgun sequencing was used on mouse brain and muscle tissues. A single viral agent was identified in each sample. For each virus, between 16% to 57% of the viral genome was acquired by sequencing only 42–108 plasmid inserts. Viruses derived from human feces or sewer effluent belonged to the Picornaviridae family and showed between 80% to 91% amino acid identities to known picornaviruses. The complete polyprotein sequence of one virus showed strong similarity to a simian picornavirus sequence in the provisional Sapelovirus genus. Insects and skunk derived viral sequences exhibited amino acid identities ranging from 25% to 98% to the segmented genomes of viruses within the Reoviridae family. Two isolates were highly divergent: one is potentially a new species within the orthoreovirus genus, and the other is a new species within the orbivirus genus. -

Discovery of a Polyomavirus in European Badgers (Meles Meles) and the Evolution of Host Range in the Family Polyomaviridae
Journal of General Virology (2015), 96, 1411–1422 DOI 10.1099/vir.0.000071 Discovery of a polyomavirus in European badgers (Meles meles) and the evolution of host range in the family Polyomaviridae Sarah C. Hill,13 Aisling A. Murphy,23 Matthew Cotten,3 Anne L. Palser,3 Phillip Benson,2 Sandrine Lesellier,4 Eamonn Gormley,5 Ce´line Richomme,6 Sylvia Grierson,7 Deirdre Ni Bhuachalla,5 Mark Chambers,4,8 Paul Kellam,3,9 Marı´a-Laura Boschiroli,10 Bernhard Ehlers,114 Michael A. Jarvis24 and Oliver G. Pybus14 Correspondence 1Department of Zoology, University of Oxford, UK Bernhard Ehlers 2School of Biomedical and Healthcare Sciences, Plymouth University, UK [email protected] 3 Michael A. Jarvis Wellcome Trust Sanger Institute, UK [email protected] 4Bacteriology Department, Animal and Plant Health Agency, UK Oliver G. Pybus 5School of Veterinary Medicine, University College Dublin (UCD), Ireland [email protected] 6ANSES, Nancy Laboratory for Rabies and Wildlife, France 7Department of Virology, Animal and Plant Health Agency, UK 8School of Veterinary Medicine, University of Surrey, UK 9MRC/UCL Centre for Medical Molecular Virology, University College London, UK 10University Paris-Est, ANSES, Laboratory for Animal Health, Bovine Tuberculosis National Reference Laboratory, France 11Robert Koch Institute, Division 12 ‘Measles, Mumps, Rubella and Viruses Affecting Immunocompromised Patients’, Germany Polyomaviruses infect a diverse range of mammalian and avian hosts, and are associated with a variety of symptoms. However, it is unknown whether the viruses are found in all mammalian families and the evolutionary history of the polyomaviruses is still unclear. Here, we report the discovery of a novel polyomavirus in the European badger (Meles meles), which to our knowledge represents the first polyomavirus to be characterized in the family Mustelidae, and within a European carnivoran. -

And Giant Guitarfish (Rhynchobatus Djiddensis)
VIRAL DISCOVERY IN BLUEGILL SUNFISH (LEPOMIS MACROCHIRUS) AND GIANT GUITARFISH (RHYNCHOBATUS DJIDDENSIS) BY HISTOPATHOLOGY EVALUATION, METAGENOMIC ANALYSIS AND NEXT GENERATION SEQUENCING by JENNIFER ANNE DILL (Under the Direction of Alvin Camus) ABSTRACT The rapid growth of aquaculture production and international trade in live fish has led to the emergence of many new diseases. The introduction of novel disease agents can result in significant economic losses, as well as threats to vulnerable wild fish populations. Losses are often exacerbated by a lack of agent identification, delay in the development of diagnostic tools and poor knowledge of host range and susceptibility. Examples in bluegill sunfish (Lepomis macrochirus) and the giant guitarfish (Rhynchobatus djiddensis) will be discussed here. Bluegill are popular freshwater game fish, native to eastern North America, living in shallow lakes, ponds, and slow moving waterways. Bluegill experiencing epizootics of proliferative lip and skin lesions, characterized by epidermal hyperplasia, papillomas, and rarely squamous cell carcinoma, were investigated in two isolated poopulations. Next generation genomic sequencing revealed partial DNA sequences of an endogenous retrovirus and the entire circular genome of a novel hepadnavirus. Giant Guitarfish, a rajiform elasmobranch listed as ‘vulnerable’ on the IUCN Red List, are found in the tropical Western Indian Ocean. Proliferative skin lesions were observed on the ventrum and caudal fin of a juvenile male quarantined at a public aquarium following international shipment. Histologically, lesions consisted of papillomatous epidermal hyperplasia with myriad large, amphophilic, intranuclear inclusions. Deep sequencing and metagenomic analysis produced the complete genomes of two novel DNA viruses, a typical polyomavirus and a second unclassified virus with a 20 kb genome tentatively named Colossomavirus. -

Characterizing and Evaluating the Zoonotic Potential of Novel Viruses Discovered in Vampire Bats
viruses Article Characterizing and Evaluating the Zoonotic Potential of Novel Viruses Discovered in Vampire Bats Laura M. Bergner 1,2,* , Nardus Mollentze 1,2 , Richard J. Orton 2 , Carlos Tello 3,4, Alice Broos 2, Roman Biek 1 and Daniel G. Streicker 1,2 1 Institute of Biodiversity, Animal Health and Comparative Medicine, College of Medical, Veterinary and Life Sciences, University of Glasgow, Glasgow G12 8QQ, UK; [email protected] (N.M.); [email protected] (R.B.); [email protected] (D.G.S.) 2 MRC–University of Glasgow Centre for Virus Research, Glasgow G61 1QH, UK; [email protected] (R.J.O.); [email protected] (A.B.) 3 Association for the Conservation and Development of Natural Resources, Lima 15037, Peru; [email protected] 4 Yunkawasi, Lima 15049, Peru * Correspondence: [email protected] Abstract: The contemporary surge in metagenomic sequencing has transformed knowledge of viral diversity in wildlife. However, evaluating which newly discovered viruses pose sufficient risk of infecting humans to merit detailed laboratory characterization and surveillance remains largely speculative. Machine learning algorithms have been developed to address this imbalance by ranking the relative likelihood of human infection based on viral genome sequences, but are not yet routinely Citation: Bergner, L.M.; Mollentze, applied to viruses at the time of their discovery. Here, we characterized viral genomes detected N.; Orton, R.J.; Tello, C.; Broos, A.; through metagenomic sequencing of feces and saliva from common vampire bats (Desmodus rotundus) Biek, R.; Streicker, D.G. and used these data as a case study in evaluating zoonotic potential using molecular sequencing Characterizing and Evaluating the data. -
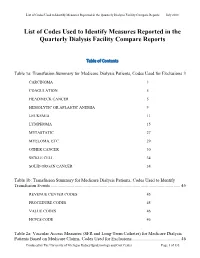
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -

The Viruses of Wild Pigeon Droppings
The Viruses of Wild Pigeon Droppings Tung Gia Phan1,2, Nguyen Phung Vo1,3,A´ kos Boros4,Pe´ter Pankovics4,Ga´bor Reuter4, Olive T. W. Li6, Chunling Wang5, Xutao Deng1, Leo L. M. Poon6, Eric Delwart1,2* 1 Blood Systems Research Institute, San Francisco, California, United States of America, 2 Department of Laboratory Medicine, University of California San Francisco, San Francisco, California, United States of America, 3 Pharmacology Department, School of Pharmacy, Ho Chi Minh City University of Medicine and Pharmacy, Ho Chi Minh, Vietnam, 4 Regional Laboratory of Virology, National Reference Laboratory of Gastroenteric Viruses, A´ NTSZ Regional Institute of State Public Health Service, Pe´cs, Hungary, 5 Stanford Genome Technology Center, Stanford, California, United States of America, 6 Centre of Influenza Research and School of Public Health, University of Hong Kong, Hong Kong SAR Abstract Birds are frequent sources of emerging human infectious diseases. Viral particles were enriched from the feces of 51 wild urban pigeons (Columba livia) from Hong Kong and Hungary, their nucleic acids randomly amplified and then sequenced. We identified sequences from known and novel species from the viral families Circoviridae, Parvoviridae, Picornaviridae, Reoviridae, Adenovirus, Astroviridae, and Caliciviridae (listed in decreasing number of reads), as well as plant and insect viruses likely originating from consumed food. The near full genome of a new species of a proposed parvovirus genus provisionally called Aviparvovirus contained an unusually long middle ORF showing weak similarity to an ORF of unknown function from a fowl adenovirus. Picornaviruses found in both Asia and Europe that are distantly related to the turkey megrivirus and contained a highly divergent 2A1 region were named mesiviruses.