Molluscum Contagiosum from Wikipedia, the Free Encyclopedia Jump To: Navigation, Search
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proper Preop Makes for Easier Toenail Surgery
April 15, 2007 • www.familypracticenews.com Skin Disorders 25 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS sia using a digital block or a distal approach to take ef- Senior Writer fect. Premedication with NSAIDs, codeine, or dextro- propoxyphene also may be appropriate, he said. WASHINGTON — Proper early management of in- To cut away the offending section of nail, an English grown toenails may help to decrease the risk of recur- anvil nail splitter is inserted under the nail plate and the rence whether or not surgery is necessary, Dr. C. Ralph cut is made all the way to the proximal nail fold. The hy- Daniel III said at the annual meeting of the American pertrophic, granulated tissue should be cut away as well. Academy of Dermatology. Many ingrown toenails are recurrent, so Dr. Daniel per- “An ingrown nail is primarily acting as a foreign-body forms a chemical matricectomy in nearly all patients after reaction. That rigid spicule penetrates soft surrounding tis- making sure that the surgical field is dry and bloodless. sue” and produces swelling, granulation tissue, and some- The proximal nail fold can be flared back to expose more times a secondary infection, said Dr. Daniel of the de- of the proximal matrix if necessary. Dr. Daniel inserts a Cal- partments of dermatology at the University of Mississippi, giswab coated with 88% phenol or 10% sodium hydroxide Jackson, and the University of Alabama, Birmingham. and applies the chemical for 30 seconds to the portion of For the early management of stage I ingrown toenails the nail matrix that needs to be destroyed. -

Nail Problems
Nail Problems Components of the Nail Congenital Disorders Racket nails, characterized by a broad short thumb nail, is the commonest congenital nail defect, dominantly inherited and seen in 1% of the population. The basic abnormality is shortness of the underlying terminal phalanx. In the yellow nail syndrome, the nail changes begin in adult life, against a background of hypoplasia of the lymphatic system. Peripheral edema is usually present and pleural effusions may occur. The nails grow very slowly and become thickened and greenish-yellow; their surface is smooth but they are over curved from side to side. Acquired Nail Changes Beau's Lines Transverse lines or grooves in nail. Causes include any severe systemic illness or medications (chemotherapy), which affects growth of the nail matrix. Clinically: The grooves or lines move distally; the distance from the nail fold lets one assess the time of trauma. Onycholysis Separation of nail from nail bed. Causes include psoriasis, dermatitis, fungal infections; medications (photo-onycholysis from tetracyclines or psoralens), thyroid disease; rarely inherited. Idiopathic onycholysis is most common among women; painless separation of nail without apparent cause. Typically, the distal third separates and underlying nail bed becomes darker and thickened. Therapy: Cut nail very short to reduce leverage encouraging separation, apply antifungal solution. Usually self-limited process. Ingrown Nail Penetration of nail plate into tissue of lateral nail fold. Almost always involves great toes. Causes include congenital malformation of nail (pincer nail), improper trimming, and tightly fitting shoes. Clinically: Distorted nail with swelling, pain, and granulation tissue along the lateral nail fold. Therapy: Mild cases: Eliminate pressure, trim nail; topical antiseptics as foot soaks or on small piece of cotton wool pushed under affected nail. -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

Proper Preop Makes for Easier Toenail Surgery
20 Dermatologic Surgery S KIN & ALLERGY N EWS • April 2007 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS produces swelling, granulation tissue, and tor or a 1- to 2-mm curette. has served as a speaker, consultant, and in- Senior Writer sometimes a secondary infection, said Dr. He also uses a technique for early-stage vestigator for the company. Daniel of the departments of dermatol- ingrown toenails in which dental floss is in- A procedure that uses an acrylic-affixed WASHINGTON — Proper early man- ogy at the University of Mississippi, Jack- serted under the ingrown nail corner with- gutter splint has been reported to be suc- agement of ingrown toenails may help to son, and the University of Alabama, Birm- out anesthesia and is kept there to separate cessful for avoiding surgery, Dr. Daniel decrease the risk of recurrence whether or ingham. the nail edge from adjacent soft tissue (J. said. A plastic gutter tube is set under the not surgery is necessary, Dr. C. Ralph For the early management of stage I in- Am. Acad. Dermatol. 2004;50:939-40). ingrown part of the nail and acrylic is Daniel III said at the annual meeting of the grown toenails in which some granula- Dr. Daniel formerly was on the board of sculpted and allowed to polymerize American Academy of Dermatology. tion tissue but no infection is present, Dr. directors for Doak Dermatologics, a sub- around the ingrown part of the nail and “An ingrown nail is primarily acting as Daniel has trained his nurse to push wisps sidiary of Bradley Pharmaceuticals Inc., hold the gutter tube in place. -

Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition
Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition: Redness, warmth, tenderness and exudate coming from the areas adjacent to the nail plate. Initial Diagnosis and Management: History and physical examination. In chronic infection appropriate radiographic (foot or toe series to rule out distal phalanx osteomyelitis) and laboratory evaluation (CBC and ESR). Ongoing Management and Objectives: Primary care should consist of Epsom salt soaks, or soapy water, and antibiotics for ten days. If Epsom salt soaks and antibiotics are ineffective, the primary care provider has the following options: Reevaluate and refer to podiatry. Perform temporary avulsion/I&D. Perform permanent avulsion followed by chemical cautery (89% Phenol or 10% NaOH application – 3 applications maintained for 30 second intervals, alcohol dilution between each application). Aftercare for all of the above is continued soaks, daily tip cleaning and bandage application. Indications for Specialty Care Referral: After the reevaluation at the end of the antibiotic period the primary care provider can refer the patient to Podiatry for avulsion/ surgical care if they do not feel comfortable performing the procedure themselves. The patient should be given a prescription for antibiotics renewal and orders to continue soaks until avulsion can be performed. Test(s) to Prepare for Consult: Test(s) Consultant May Need To Do: Criteria for Return to Primary Care: After completion of the surgical procedure, patients will be returned to the primary care provider for follow-up. Revision History: Created Revised Disclaimer: Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be considered inclusive of all accepted methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. -
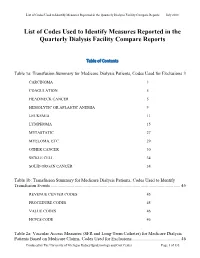
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -

Client Services Manual Public Health Laboratory
CLIENT SERVICES MANUAL PUBLIC HEALTH LABORATORY COUNTY OF SANTA CLARA 2220 MOORPARK AVE, 2ND FLOOR SAN JOSE, CA 95128 (P) 408.885.4272 | (F) 408.885.4275 http://www.sccgov.org/sites /sccphd/en-us/HealthProviders/Lab Patricia Dadone, Public Health Laboratory Director Sara H. Cody, MD, Health Officer and Public Health Director Table of Contents 1 GENERAL INFORMATION ............................................................................................... 1.1 ROLE .............................................................................................................................................................. 1.1 MISSION STATEMENT ..................................................................................................................................... 1.1 ABBREVIATIONS.............................................................................................................................................. 1.2 LABORATORY CERTIFICATIONS ........................................................................................................................ 1.4 CLIENT SERVICES ............................................................................................................................................ 1.5 Hours of Operation: .............................................................................................................................. 1.5 Supplies .................................................................................................................................................. -

Specimen Type, Collection Methods, and Diagnostic Assays Available For
Specimen type, collection methods, and diagnostic assays available for the detection of poxviruses from human specimens by the Poxvirus and Rabies Branch, Centers for Disease Control and Prevention1. Specimen Orthopoxvirus Parapoxvirus Yatapoxvirus Molluscipoxvirus Specimen type collection method PCR6 Culture EM8 IHC9,10 Serology11 PCR12 EM8 IHC9,10 PCR13 EM8 PCR EM8 Lesion material Fresh or frozen Swab 5 Lesion material [dry or in media ] [vesicle / pustule Formalin fixed skin, scab / crust, etc.] Paraffin block Fixed slide(s) Container Lesion fluid Swab [vesicle / pustule [dry or in media5] fluid, etc.] Touch prep slide Blood EDTA2 EDTA tube 7 Spun or aliquoted Serum before shipment Spun or aliquoted Plasma before shipment CSF3,4 Sterile 1. The detection of poxviruses by electron microscopy (EM) and immunohistochemical staining (IHC) is performed by the Infectious Disease Pathology Branch of the CDC. 2. EDTA — Ethylenediaminetetraacetic acid. 3. CSF — Cerebrospinal fluid. 4. In order to accurately interpret test results generated from CSF specimens, paired serum must also be submitted. 5. If media is used to store and transport specimens a minimal amount should be used to ensure as little dilution of DNA as possible. 6. Orthopoxvirus generic real-time polymerase chain reaction (PCR) assays will amplify DNA from numerous species of virus within the Orthopoxvirus genus. Species-specific real-time PCR assays are available for selective detection of DNA from variola virus, vaccinia virus, monkeypox virus, and cowpox virus. 7. Blood is not ideal for the detection of orthopoxviruses by PCR as the period of viremia has often passed before sampling occurs. 8. EM can reveal the presence of a poxvirus in clinical specimens or from virus culture, but this technique cannot differentiate between virus species within the same genus. -

Ingrown Toenails
POST-OP NAIL CARE The day following the procedure, remove the bandage and begin soaking the toe for 10-15 minutes at least once daily. If the bandage does not come off easily, soak in warm water with one (1) tablespoon Epson Salts. As you soak, use a cotton tipped applicator (Q-tip) to clean the nail groove. Also, gently pull the skin edges back from the area where the nail was removed to be sure that any draining is released. After drying the toes, apply a light amount of triple antibiotic ointment (Neosporin) or other topical anesthetic, and light gauze or a bandage (Band-aid). Gauze is best to absorb INGROWN drainage. After a few days, the toe may be Brian Gardner, D.P.M. TOENAILS overly moist and need to dry. Use less triple antibiotic, continue soaking, Podiatrist and dress with light gauze or a Dr. Brian Gardner specializes in bandage (Band-aid). As drying foot and ankle surgery, wound care, occurs, tenderness will usually biomechanics, sports medicine, decrease. Continue soaks until the diabetic foot care, area is no longer draining (usually and general foot care. several weeks, if the nail root was treated with a chemical). facebook.com/UintahBasinHealthcare www.ubh.org 435.725.2025, Roosevelt 435.781.2030, Vernal 250 W 300 N Clinic #2 Suite 203 (Level 2), Roosevelt, Utah 379 N 500 W, Vernal, Utah Nails grow from a root beneath the skin TREATMENT IMPORTANT called the “matrix.” This growth center TREATMENT INFORMATION can vary in size and shape. It may Initially, your doctor may be able to produce a nail which is flat, curved, trim the ingrown toenail. -

VACCINIA VIRUS O1L VIRULENCE GENE and PROTEIN LOCALIZATION by Shayna Mooney a Senior Honors Project Presented to the Honors Co
VACCINIA VIRUS O1L VIRULENCE GENE AND PROTEIN LOCALIZATION by Shayna Mooney A Senior Honors Project Presented to the Honors College East Carolina University In Partial Fulfillment of the Requirements for Graduation with Honors by Shayna Mooney Greenville, NC May 2015 Approved by: Dr. Rachel Roper Department of Microbiology and Immunology, Brody School of Medicine Mooney 2 Abstract Smallpox killed an estimated 500 million people in the twentieth century alone. Although this fatal disease was eradicated from the world over thirty years ago, its potential use as a bioterrorism agent remains a concern. In addition, monkeypox continues to cause human outbreaks in Africa, and in the US in 2003. Vaccinia virus, the live virus vaccine for smallpox and monkeypox, is dangerous for immunocompromised individuals, and a safer vaccine is needed. The Roper lab studies how poxviruses cause disease in mammals and which genes contribute to virulence. The vaccinia virus O1L gene is highly conserved in poxviruses, and we have shown that it is required for full virulence in mice. When the O1L gene is removed from the wild type virus, the virus becomes attenuated, and immune responses are improved. Very little is known about this protein including its molecular weight, location within the cell and its function. We raised anti O1L peptide antibodies in rabbits and are using these to investigate the localization of the O1L protein using immunofluorescence techniques. In accordance with preliminary data from western blot analysis, we hypothesized that the O1L protein is located in the nucleus of the cell. Through immunofluorescence, the O1L protein was detected in the nucleus and cytoplasm of the cell. -

Risk Groups: Viruses (C) 1988, American Biological Safety Association
Rev.: 1.0 Risk Groups: Viruses (c) 1988, American Biological Safety Association BL RG RG RG RG RG LCDC-96 Belgium-97 ID Name Viral group Comments BMBL-93 CDC NIH rDNA-97 EU-96 Australia-95 HP AP (Canada) Annex VIII Flaviviridae/ Flavivirus (Grp 2 Absettarov, TBE 4 4 4 implied 3 3 4 + B Arbovirus) Acute haemorrhagic taxonomy 2, Enterovirus 3 conjunctivitis virus Picornaviridae 2 + different 70 (AHC) Adenovirus 4 Adenoviridae 2 2 (incl animal) 2 2 + (human,all types) 5 Aino X-Arboviruses 6 Akabane X-Arboviruses 7 Alastrim Poxviridae Restricted 4 4, Foot-and- 8 Aphthovirus Picornaviridae 2 mouth disease + viruses 9 Araguari X-Arboviruses (feces of children 10 Astroviridae Astroviridae 2 2 + + and lambs) Avian leukosis virus 11 Viral vector/Animal retrovirus 1 3 (wild strain) + (ALV) 3, (Rous 12 Avian sarcoma virus Viral vector/Animal retrovirus 1 sarcoma virus, + RSV wild strain) 13 Baculovirus Viral vector/Animal virus 1 + Togaviridae/ Alphavirus (Grp 14 Barmah Forest 2 A Arbovirus) 15 Batama X-Arboviruses 16 Batken X-Arboviruses Togaviridae/ Alphavirus (Grp 17 Bebaru virus 2 2 2 2 + A Arbovirus) 18 Bhanja X-Arboviruses 19 Bimbo X-Arboviruses Blood-borne hepatitis 20 viruses not yet Unclassified viruses 2 implied 2 implied 3 (**)D 3 + identified 21 Bluetongue X-Arboviruses 22 Bobaya X-Arboviruses 23 Bobia X-Arboviruses Bovine 24 immunodeficiency Viral vector/Animal retrovirus 3 (wild strain) + virus (BIV) 3, Bovine Bovine leukemia 25 Viral vector/Animal retrovirus 1 lymphosarcoma + virus (BLV) virus wild strain Bovine papilloma Papovavirus/ -

Supporting Information
Supporting Information Rosenberg et al. 10.1073/pnas.1307243110 SI Results and Discussion domestic ungulates (horses, cows, sheep, goats, camels, and pigs) Of the 83 arboviruses, nonhuman vertebrate hosts have been and rodents in both groups might be a consequence of spatial identified for 70 (84%); the remaining 13 are presumed to be proximity to humans. Sentinel monkeys were often used in pro- zoonoses because there is no indication they can be transmitted cedures to isolate arboviruses, which might account for their directly between humans by vectors (Table S1). Animal hosts have higher representation among arboviruses. In contrast, there are been identified for at least 57 (44%) of the 130 nonarboviruses; an few published records of bats being routinely sampled during additional 5 (8%) are presumed on epidemiological evidence to arbovirus studies, and only two arboviruses (3%) have been iso- have nonhuman reservoirs (Table S1). A number of viruses infect lated from bats. The reason a much larger number of arbovirus more than one nonhuman vertebrate host species and it is likely species (n = 16) have been isolated from birds than have that the variety of hosts is wider than has been recorded. The nonarbovirus species (n = 1) might, however, be characteristic of predominant host groups for arboviruses (n = 70) are nonhuman the pathogenicity of the togaviruses and flaviviruses, which are primates (31%), rodents (29%), ungulates (26%), and birds (23%); much more common among the arboviruses. The most prominent for the nonarboviruses (n = 57), they are rodents (30%), ungu- vectors of arboviruses were mosquitoes (67%), ticks (19%), and lates (26%), bats (23%), and primates (16%).