Ingrown Toenails: Digging out the Facts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proper Preop Makes for Easier Toenail Surgery
April 15, 2007 • www.familypracticenews.com Skin Disorders 25 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS sia using a digital block or a distal approach to take ef- Senior Writer fect. Premedication with NSAIDs, codeine, or dextro- propoxyphene also may be appropriate, he said. WASHINGTON — Proper early management of in- To cut away the offending section of nail, an English grown toenails may help to decrease the risk of recur- anvil nail splitter is inserted under the nail plate and the rence whether or not surgery is necessary, Dr. C. Ralph cut is made all the way to the proximal nail fold. The hy- Daniel III said at the annual meeting of the American pertrophic, granulated tissue should be cut away as well. Academy of Dermatology. Many ingrown toenails are recurrent, so Dr. Daniel per- “An ingrown nail is primarily acting as a foreign-body forms a chemical matricectomy in nearly all patients after reaction. That rigid spicule penetrates soft surrounding tis- making sure that the surgical field is dry and bloodless. sue” and produces swelling, granulation tissue, and some- The proximal nail fold can be flared back to expose more times a secondary infection, said Dr. Daniel of the de- of the proximal matrix if necessary. Dr. Daniel inserts a Cal- partments of dermatology at the University of Mississippi, giswab coated with 88% phenol or 10% sodium hydroxide Jackson, and the University of Alabama, Birmingham. and applies the chemical for 30 seconds to the portion of For the early management of stage I ingrown toenails the nail matrix that needs to be destroyed. -

Nail Problems
Nail Problems Components of the Nail Congenital Disorders Racket nails, characterized by a broad short thumb nail, is the commonest congenital nail defect, dominantly inherited and seen in 1% of the population. The basic abnormality is shortness of the underlying terminal phalanx. In the yellow nail syndrome, the nail changes begin in adult life, against a background of hypoplasia of the lymphatic system. Peripheral edema is usually present and pleural effusions may occur. The nails grow very slowly and become thickened and greenish-yellow; their surface is smooth but they are over curved from side to side. Acquired Nail Changes Beau's Lines Transverse lines or grooves in nail. Causes include any severe systemic illness or medications (chemotherapy), which affects growth of the nail matrix. Clinically: The grooves or lines move distally; the distance from the nail fold lets one assess the time of trauma. Onycholysis Separation of nail from nail bed. Causes include psoriasis, dermatitis, fungal infections; medications (photo-onycholysis from tetracyclines or psoralens), thyroid disease; rarely inherited. Idiopathic onycholysis is most common among women; painless separation of nail without apparent cause. Typically, the distal third separates and underlying nail bed becomes darker and thickened. Therapy: Cut nail very short to reduce leverage encouraging separation, apply antifungal solution. Usually self-limited process. Ingrown Nail Penetration of nail plate into tissue of lateral nail fold. Almost always involves great toes. Causes include congenital malformation of nail (pincer nail), improper trimming, and tightly fitting shoes. Clinically: Distorted nail with swelling, pain, and granulation tissue along the lateral nail fold. Therapy: Mild cases: Eliminate pressure, trim nail; topical antiseptics as foot soaks or on small piece of cotton wool pushed under affected nail. -

Comparative Study of Disinfectants for Use in Low-Cost Gravity Driven Household Water Purifiers Rajshree A
443 © IWA Publishing 2013 Journal of Water and Health | 11.3 | 2013 Comparative study of disinfectants for use in low-cost gravity driven household water purifiers Rajshree A. Patil, Shankar B. Kausley, Pradeep L. Balkunde and Chetan P. Malhotra ABSTRACT Point-of-use (POU) gravity-driven household water purifiers have been proven to be a simple, low- Rajshree A. Patil Shankar B. Kausley (corresponding author) cost and effective intervention for reducing the impact of waterborne diseases in developing Pradeep L. Balkunde Chetan P. Malhotra countries. The goal of this study was to compare commonly used water disinfectants for their TCS Innovation Labs – TRDDC, fi 54B, Hadapsar Industrial Estate, feasibility of adoption in low-cost POU water puri ers. The potency of each candidate disinfectant Pune - 411013, was evaluated by conducting a batch disinfection study for estimating the concentration of India E-mail: [email protected] disinfectant needed to inactivate a given concentration of the bacterial strain Escherichia coli ATCC 11229. Based on the concentration of disinfectant required, the size, weight and cost of a model purifier employing that disinfectant were estimated. Model purifiers based on different disinfectants were compared and disinfectants which resulted in the most safe, compact and inexpensive purifiers were identified. Purifiers based on bromine, tincture iodine, calcium hypochlorite and sodium dichloroisocyanurate were found to be most efficient, cost effective and compact with replacement parts costing US$3.60–6.00 for every 3,000 L of water purified and are thus expected to present the most attractive value proposition to end users. Key words | disinfectant, drinking water, E. -

Silver Nanoparticle Nanocomposite Filaments Produced by an In-Situ Reduction Reactive Melt Mixing Process
biomimetics Article Three-Dimensional Printed Antimicrobial Objects of Polylactic Acid (PLA)-Silver Nanoparticle Nanocomposite Filaments Produced by an In-Situ Reduction Reactive Melt Mixing Process Nectarios Vidakis 1, Markos Petousis 1,* , Emmanouel Velidakis 1, Marco Liebscher 2 and Lazaros Tzounis 3 1 Mechanical Engineering Department, Hellenic Mediterranean University, Estavromenos, 71004 Heraklion, Crete, Greece; [email protected] (N.V.); [email protected] (E.V.) 2 Institute of Construction Materials, Technische Universität Dresden, DE-01062 Dresden, Germany; [email protected] 3 Department of Materials Science and Engineering, University of Ioannina, 45110 Ioannina, Greece; [email protected] * Correspondence: [email protected]; Tel.: +30-2810-37-9227 Received: 14 August 2020; Accepted: 31 August 2020; Published: 2 September 2020 Abstract: In this study, an industrially scalable method is reported for the fabrication of polylactic acid (PLA)/silver nanoparticle (AgNP) nanocomposite filaments by an in-situ reduction reactive melt mixing method. The PLA/AgNP nanocomposite filaments have been produced initially + reducing silver ions (Ag ) arising from silver nitrate (AgNO3) precursor mixed in the polymer melt to elemental silver (Ag0) nanoparticles, utilizing polyethylene glycol (PEG) or polyvinyl pyrrolidone (PVP), respectively, as macromolecular blend compound reducing agents. PEG and PVP were added at various concentrations, to the PLA matrix. The PLA/AgNP filaments have been used to manufacture 3D printed antimicrobial (AM) parts by Fused Filament Fabrication (FFF). The 3D printed PLA/AgNP parts exhibited significant AM properties examined by the reduction in Staphylococcus aureus (S. aureus) and Escherichia coli (E. coli) bacteria viability (%) experiments at 30, 60, and 120 min duration of contact (p < 0.05; p-value (p): probability). -

Proper Preop Makes for Easier Toenail Surgery
20 Dermatologic Surgery S KIN & ALLERGY N EWS • April 2007 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS produces swelling, granulation tissue, and tor or a 1- to 2-mm curette. has served as a speaker, consultant, and in- Senior Writer sometimes a secondary infection, said Dr. He also uses a technique for early-stage vestigator for the company. Daniel of the departments of dermatol- ingrown toenails in which dental floss is in- A procedure that uses an acrylic-affixed WASHINGTON — Proper early man- ogy at the University of Mississippi, Jack- serted under the ingrown nail corner with- gutter splint has been reported to be suc- agement of ingrown toenails may help to son, and the University of Alabama, Birm- out anesthesia and is kept there to separate cessful for avoiding surgery, Dr. Daniel decrease the risk of recurrence whether or ingham. the nail edge from adjacent soft tissue (J. said. A plastic gutter tube is set under the not surgery is necessary, Dr. C. Ralph For the early management of stage I in- Am. Acad. Dermatol. 2004;50:939-40). ingrown part of the nail and acrylic is Daniel III said at the annual meeting of the grown toenails in which some granula- Dr. Daniel formerly was on the board of sculpted and allowed to polymerize American Academy of Dermatology. tion tissue but no infection is present, Dr. directors for Doak Dermatologics, a sub- around the ingrown part of the nail and “An ingrown nail is primarily acting as Daniel has trained his nurse to push wisps sidiary of Bradley Pharmaceuticals Inc., hold the gutter tube in place. -

Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition
Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition: Redness, warmth, tenderness and exudate coming from the areas adjacent to the nail plate. Initial Diagnosis and Management: History and physical examination. In chronic infection appropriate radiographic (foot or toe series to rule out distal phalanx osteomyelitis) and laboratory evaluation (CBC and ESR). Ongoing Management and Objectives: Primary care should consist of Epsom salt soaks, or soapy water, and antibiotics for ten days. If Epsom salt soaks and antibiotics are ineffective, the primary care provider has the following options: Reevaluate and refer to podiatry. Perform temporary avulsion/I&D. Perform permanent avulsion followed by chemical cautery (89% Phenol or 10% NaOH application – 3 applications maintained for 30 second intervals, alcohol dilution between each application). Aftercare for all of the above is continued soaks, daily tip cleaning and bandage application. Indications for Specialty Care Referral: After the reevaluation at the end of the antibiotic period the primary care provider can refer the patient to Podiatry for avulsion/ surgical care if they do not feel comfortable performing the procedure themselves. The patient should be given a prescription for antibiotics renewal and orders to continue soaks until avulsion can be performed. Test(s) to Prepare for Consult: Test(s) Consultant May Need To Do: Criteria for Return to Primary Care: After completion of the surgical procedure, patients will be returned to the primary care provider for follow-up. Revision History: Created Revised Disclaimer: Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be considered inclusive of all accepted methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. -

Silver As a Drinking-Water Disinfectant
Silver as a drinking-water disinfectant Silver as a drinking-water disinfectant Alternative drinking-water disinfectants: silver ISBN 978-92-4-151369-2 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Alternative drinking-water disinfectants: bromine, iodine and silver. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. -

Ingrown Toenails
POST-OP NAIL CARE The day following the procedure, remove the bandage and begin soaking the toe for 10-15 minutes at least once daily. If the bandage does not come off easily, soak in warm water with one (1) tablespoon Epson Salts. As you soak, use a cotton tipped applicator (Q-tip) to clean the nail groove. Also, gently pull the skin edges back from the area where the nail was removed to be sure that any draining is released. After drying the toes, apply a light amount of triple antibiotic ointment (Neosporin) or other topical anesthetic, and light gauze or a bandage (Band-aid). Gauze is best to absorb INGROWN drainage. After a few days, the toe may be Brian Gardner, D.P.M. TOENAILS overly moist and need to dry. Use less triple antibiotic, continue soaking, Podiatrist and dress with light gauze or a Dr. Brian Gardner specializes in bandage (Band-aid). As drying foot and ankle surgery, wound care, occurs, tenderness will usually biomechanics, sports medicine, decrease. Continue soaks until the diabetic foot care, area is no longer draining (usually and general foot care. several weeks, if the nail root was treated with a chemical). facebook.com/UintahBasinHealthcare www.ubh.org 435.725.2025, Roosevelt 435.781.2030, Vernal 250 W 300 N Clinic #2 Suite 203 (Level 2), Roosevelt, Utah 379 N 500 W, Vernal, Utah Nails grow from a root beneath the skin TREATMENT IMPORTANT called the “matrix.” This growth center TREATMENT INFORMATION can vary in size and shape. It may Initially, your doctor may be able to produce a nail which is flat, curved, trim the ingrown toenail. -
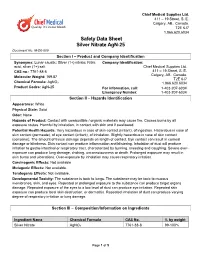
Safety Data Sheet Silver Nitrate Agn-25 Document No
Chief Medical Supplies Ltd. 411 – 19 Street, S. E. Calgary, AB., Canada. T2E 6J7 1.866.620.6034 Safety Data Sheet Silver Nitrate AgN-25 Document No. M-D6-009 Section I – Product and Company Identification Synonyms: Lunar caustic; Silver (1+) nitrate; Nitric Company Identification: acid, silver (1+) salt Chief Medical Supplies Ltd. CAS no.: 7761-88-8 411 – 19 Street, S. E. Calgary, AB., Canada. Molecular Weight: 169.87 T2E 6J7 Chemical Formula: AgNO3 1.866.620.6034 Product Codes: AgN-25 For information, call: 1-403-207-6034 Emergency Number: 1-403-207-6034 Section II – Hazards Identification Appearance: White Physical State: Solid Odor: None Hazards of Product: Contact with combustible / organic materials may cause fire. Causes burns by all exposure routes. Harmful by inhalation, in contact with skin and if swallowed. Potential Health Hazards: Very hazardous in case of skin contact (irritant), of ingestion. Hazardous in case of skin contact (permeate), of eye contact (irritant), of inhalation. Slightly hazardous in case of skin contact (corrosive). The amount of tissue damage depends on length of contact. Eye contact can result in corneal damage or blindness. Skin contact can produce inflammation and blistering. Inhalation of dust will produce irritation to gastro-intestinal or respiratory tract, characterized by burning, sneezing and coughing. Severe over- exposure can produce lung damage, choking, unconsciousness or death. Prolonged exposure may result in skin burns and ulcerations. Over-exposure by inhalation may cause respiratory irritation. Carcinogenic Effects: Not available Mutagenic Effects: Not available. Teratogenic Effects: Not available. Developmental Toxicity: The substance is toxic to lungs. -

Effects of Some Chemicals on Vase Life of Some Cut Flowers I
J. Plant Production, Mansoura Univ., Vol. 8 (1): 49 - 53, 2017 Effects of Some Chemicals on Vase Life of Some Cut Flowers I. Effect of 8-Hydroxyquinoline Sulfate, Silver Nitrate, Silver Nano Particles and Chitosan on Vase Life and Quality of Cut Rose Flowers (Rosa hybrida. Cv. “Black Magic”) Abdel-Kader, H. H.1; A. M. Hamza1; T. T. Elbaz2 and S. M. Eissa2 1 Veg. and Flor. Dept., Fac. of Agric., Mansoura Unive. 2 Ornam, Plants and Lands. Gard. Res. Dept., Hort. Res. Inst., Agric. Res. Cent., Giza ABSTRACT This investigation was carried out during 2015 and 2016 seasons to determine whether the selected chemical agents could be used to improve the postharvest quality of Rosa hybrida L.cv. “Black Magic” cut flowers. Freshly cut flowers were placed in glass cylinders containing 100 ml of preservative solutions [8-hydroxyquinoline sulfate (8-HQS) at 200 ppm, silver nitrate (AgNO3) at 10 ppm, Chitosan at 50, 75 or 100 ppm silver nano-particles (SN) at 5, 10 or 15 ppm, and distilled water as a control treatment].All preservative solutions and the control treatment included sucrose at 20 g/l. Compared to the control, treatments which contained of (AgNO3) or (SN) improved the quality and vase life of the flowers. They were more effective in promoting water uptake, increasing fresh weight of the flower and water balance so that the vase life of cut flowers were extended to 13.67 and 12 days during the first and second seasons, respectively. The results of bacterial count in the vase solution and the Scanning Electron Microscopy (SEM) pictures of the cut base of the stem indicated that (AgNO3) or (SN) strongly reduced bacterial population in both the vase solution and the cut stem base. -

Silver Nitrate Complexes of Nitrogen-Containing
Silver Nitrate Complexes of Nitrogen-Containing Heterocycles Hubert Schmidbaur*, Angelika Mair, Gerhard Müller*, Joachim Lachmann+, and Siegfried Gamper+ Anorganisch-chemisches Institut der Technischen Universität München, Lichtenbergstraße 4, D-8046 Garching Z. Naturforsch. 46b, 912-918 (1991); received February 19, 1991 Silver Complexes, Nitrogen Heterocycles, Pyrazole. Triazole, 8 -Amino-quinoline Pyrazole, 1,2,4-triazole, and 8 -amino-quinoline form complexes as neutral ligands with sil ver nitrate in slightly acidic aqueous medium. With pyrazole a 2:1 complex (1) is obtained. The crystal structure determination revealed an ionic structure with independent N 0 3~ anions and centrosymmetrical (pyr) 2Ag+ cations with a linear coordination geometry at the silver atoms. The reactions with 1,2,4-triazole and 8 -amino-quinoline yield dimeric 1:1 complexes (2, 3), in which the silver atoms are bridged by the ligands and have short contacts with nitrate oxygen atoms. The coordination geometry of the metals can thus be described as distorted tetrahedral. A 1 :1 complex with 2,3-diphenyl-1,2,4-triazole (2a) and a 2:1 complex with 8 -hydroxy-quino- line (4) have also been prepared, but not characterized in detail. Introduction prepared and characterized a series of complexes Complex formation of silver(I) cations by am of silver nitrate with pyrazole, (diphenyl)triazole, monia and amines has been well established in an 8 -amino-quinoline, and 8 -hydroxy-quinoline. alytical chemistry and chemical technology of sil ver for more than a century. However, nitrogen- Preparation and Properties of the Complexes containing heterocycles have also been among the early complexing agents. -

Supporting Information for Proteomics DOI 10.1002/Pmic.200500596
Supporting Information for Proteomics DOI 10.1002/pmic.200500596 Li-Tai Jin, Sun-Young Hwang, Gyurng-Soo Yoo and Jung-Kap Choi A mass spectrometry compatible silver staining method for protein incorporating a new silver sensitizer in sodium dodecyl sulfate-polyacrylamide electrophoresis gels ª 2006 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.proteomics-journal.com Supplementary Information A mass spectrometry compatible silver staining method for protein incorporating a new silver sensitizer in sodium dodecyl sulfate- polyacrylamide electrophoresis gels Li-Tai Jin, Sun-Young Hwang, Gyurng-Soo Yoo and Jung-Kap Choi College of Pharmacy, Chonnam National University, Kwangju 500-757, South Korea Correspondence: Prof. Jung-Kap Choi, Lab. of Analytical Biochemistry, College of Pharmacy, Chonnam National University, Yongbong-Dong 300, Buk- Ku, Kwangju 500-757, South Korea (Phone: +8262-530-2930; Fax: +8262-530- 2911; E-mail: [email protected]) Abbreviations used: EBT, eriochrome black T Keywords: Electrophoresis / Eriochrome black T / Mass spectrometry / Protein silver staining 1 1 Supplementary Introduction In life sciences, sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) is a reliable and widely used analytical technique for the separation and identification of proteins. Given the development of proteomics, the ability to analyze and identify protein in a gel matrix at high sensitivity is becoming more important [1,2]. Various protein staining methods have been developed based on visible organic dyes, fluorescent and silver based systems, and radiolabeling. Of these, organic dyes are easily used but have low sensitivities, with detection limits in the range of 1-50 ng for proteins [2,3]. Fluorescent staining methods are a little more sensitive than dye-based methods but for data reading, special instruments are necessary that involve UV.