Proper Preop Makes for Easier Toenail Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proper Preop Makes for Easier Toenail Surgery
April 15, 2007 • www.familypracticenews.com Skin Disorders 25 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS sia using a digital block or a distal approach to take ef- Senior Writer fect. Premedication with NSAIDs, codeine, or dextro- propoxyphene also may be appropriate, he said. WASHINGTON — Proper early management of in- To cut away the offending section of nail, an English grown toenails may help to decrease the risk of recur- anvil nail splitter is inserted under the nail plate and the rence whether or not surgery is necessary, Dr. C. Ralph cut is made all the way to the proximal nail fold. The hy- Daniel III said at the annual meeting of the American pertrophic, granulated tissue should be cut away as well. Academy of Dermatology. Many ingrown toenails are recurrent, so Dr. Daniel per- “An ingrown nail is primarily acting as a foreign-body forms a chemical matricectomy in nearly all patients after reaction. That rigid spicule penetrates soft surrounding tis- making sure that the surgical field is dry and bloodless. sue” and produces swelling, granulation tissue, and some- The proximal nail fold can be flared back to expose more times a secondary infection, said Dr. Daniel of the de- of the proximal matrix if necessary. Dr. Daniel inserts a Cal- partments of dermatology at the University of Mississippi, giswab coated with 88% phenol or 10% sodium hydroxide Jackson, and the University of Alabama, Birmingham. and applies the chemical for 30 seconds to the portion of For the early management of stage I ingrown toenails the nail matrix that needs to be destroyed. -

Nail Problems
Nail Problems Components of the Nail Congenital Disorders Racket nails, characterized by a broad short thumb nail, is the commonest congenital nail defect, dominantly inherited and seen in 1% of the population. The basic abnormality is shortness of the underlying terminal phalanx. In the yellow nail syndrome, the nail changes begin in adult life, against a background of hypoplasia of the lymphatic system. Peripheral edema is usually present and pleural effusions may occur. The nails grow very slowly and become thickened and greenish-yellow; their surface is smooth but they are over curved from side to side. Acquired Nail Changes Beau's Lines Transverse lines or grooves in nail. Causes include any severe systemic illness or medications (chemotherapy), which affects growth of the nail matrix. Clinically: The grooves or lines move distally; the distance from the nail fold lets one assess the time of trauma. Onycholysis Separation of nail from nail bed. Causes include psoriasis, dermatitis, fungal infections; medications (photo-onycholysis from tetracyclines or psoralens), thyroid disease; rarely inherited. Idiopathic onycholysis is most common among women; painless separation of nail without apparent cause. Typically, the distal third separates and underlying nail bed becomes darker and thickened. Therapy: Cut nail very short to reduce leverage encouraging separation, apply antifungal solution. Usually self-limited process. Ingrown Nail Penetration of nail plate into tissue of lateral nail fold. Almost always involves great toes. Causes include congenital malformation of nail (pincer nail), improper trimming, and tightly fitting shoes. Clinically: Distorted nail with swelling, pain, and granulation tissue along the lateral nail fold. Therapy: Mild cases: Eliminate pressure, trim nail; topical antiseptics as foot soaks or on small piece of cotton wool pushed under affected nail. -

Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition
Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition: Redness, warmth, tenderness and exudate coming from the areas adjacent to the nail plate. Initial Diagnosis and Management: History and physical examination. In chronic infection appropriate radiographic (foot or toe series to rule out distal phalanx osteomyelitis) and laboratory evaluation (CBC and ESR). Ongoing Management and Objectives: Primary care should consist of Epsom salt soaks, or soapy water, and antibiotics for ten days. If Epsom salt soaks and antibiotics are ineffective, the primary care provider has the following options: Reevaluate and refer to podiatry. Perform temporary avulsion/I&D. Perform permanent avulsion followed by chemical cautery (89% Phenol or 10% NaOH application – 3 applications maintained for 30 second intervals, alcohol dilution between each application). Aftercare for all of the above is continued soaks, daily tip cleaning and bandage application. Indications for Specialty Care Referral: After the reevaluation at the end of the antibiotic period the primary care provider can refer the patient to Podiatry for avulsion/ surgical care if they do not feel comfortable performing the procedure themselves. The patient should be given a prescription for antibiotics renewal and orders to continue soaks until avulsion can be performed. Test(s) to Prepare for Consult: Test(s) Consultant May Need To Do: Criteria for Return to Primary Care: After completion of the surgical procedure, patients will be returned to the primary care provider for follow-up. Revision History: Created Revised Disclaimer: Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be considered inclusive of all accepted methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. -

Ingrown Toenails
POST-OP NAIL CARE The day following the procedure, remove the bandage and begin soaking the toe for 10-15 minutes at least once daily. If the bandage does not come off easily, soak in warm water with one (1) tablespoon Epson Salts. As you soak, use a cotton tipped applicator (Q-tip) to clean the nail groove. Also, gently pull the skin edges back from the area where the nail was removed to be sure that any draining is released. After drying the toes, apply a light amount of triple antibiotic ointment (Neosporin) or other topical anesthetic, and light gauze or a bandage (Band-aid). Gauze is best to absorb INGROWN drainage. After a few days, the toe may be Brian Gardner, D.P.M. TOENAILS overly moist and need to dry. Use less triple antibiotic, continue soaking, Podiatrist and dress with light gauze or a Dr. Brian Gardner specializes in bandage (Band-aid). As drying foot and ankle surgery, wound care, occurs, tenderness will usually biomechanics, sports medicine, decrease. Continue soaks until the diabetic foot care, area is no longer draining (usually and general foot care. several weeks, if the nail root was treated with a chemical). facebook.com/UintahBasinHealthcare www.ubh.org 435.725.2025, Roosevelt 435.781.2030, Vernal 250 W 300 N Clinic #2 Suite 203 (Level 2), Roosevelt, Utah 379 N 500 W, Vernal, Utah Nails grow from a root beneath the skin TREATMENT IMPORTANT called the “matrix.” This growth center TREATMENT INFORMATION can vary in size and shape. It may Initially, your doctor may be able to produce a nail which is flat, curved, trim the ingrown toenail. -

Customizable Wallet Cards
reason, we’ll refund your cost. your refund we’ll reason, cost. your refund we’ll reason, cost. your refund we’ll reason, cost. your refund we’ll reason, If you aren’t satisfied, for any any for satisfied, aren’t you If any for satisfied, aren’t you If any for satisfied, aren’t you If any for satisfied, aren’t you If waiting. No waiting. No waiting. No waiting. No apps to download. download. to apps No download. to apps No download. to apps No download. to apps No video required. required. video No required. deo vi No required. deo vi No required. deo vi No ne. li on t bu ne. li on t bu ne. li on t bu ne. li on t bu isit – – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik Fold line Fold Your 24/7 Your 24/7 Your 24/7 Your 24/7 online clinic online clinic online clinic online clinic A visit is just $45.* Insurance is accepted and Insurance is accepted and Insurance is accepted and Insurance is accepted and Insurance is accepted. applies to your deductible. appInsurancelies to your is accepted.deductible. appInsurancelies to your is deductible.accepted. appInsurancelies to your is deductible.accepted. *No*No cost cost if we can’tcan't treat trea you.t you. *No*No cost cost ifif we can’tcan't treat trea tyou. you. *No*No costcost if wewe can’tcan't treat treat you. -

Procedural Review of Toenail Excision Scott Klosterman, DO, Candace Prince, OSM 4
Osteopathic Family Physician (2012) 4, 18-23 Procedural review of toenail excision Scott Klosterman, DO, Candace Prince, OSM 4 From Spartanburg Regional Family Medicine Residency Program, Spartanburg, SC KEYWORDS: Toenail removal is a common procedure that family physicians routinely perform in the office. This article Toenail removal; highlights the acute and chronic indications for toenail removal and its contraindications, potential compli- Paronychia; cations, and procedural details including digital block anesthesia. A sample consent form and patient Onychomycrosis; educational handout are provided as well as the current diagnostic International Classification of Diseases, Ingrown toenail; 9th revision, and current procedural terminology codes for the clinician to use. Matrixectomy © 2012 Elsevier Inc. All rights reserved. Family physicians are often the primary health care con- a partial or complete matrixectomy (permanent nail removal) tact for patients with toenail problems. Toenail complaints may be necessary for these chronic conditions, and with on- ranging from paronychia to onychomycosis affect every age ychocryptosis because of its high rate of recurrence.2,4,11 Fi- group, and surgical excision of the nail may be an appro- nally, in cases of growths or discoloration beneath the nail, nail priate treatment option. Our purpose is to review the indi- plate removal with biopsy may be needed to rule out malignant cations and procedural details for toenail removal, provide a neoplasms, although biopsy techniques of the nail and nail bed concise patient consent form and educational handout for are outside the scope of this review.2,3 postprocedural care, and review the current International Classification of Diseases, 9th revision (ICD-9) and current procedural terminology (CPT) coding for such procedures. -
Ingrown Toenails: Digging out the Facts
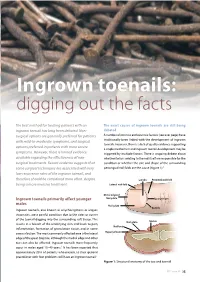
Ingrown toenails: digging out the facts The best method for treating patients with an The exact causes of ingrown toenails are still being ingrown toenail has long been debated. Non- debated surgical options are generally preferred for patients A number of intrinsic and extrinsic factors (see over page) have with mild-to-moderate symptoms, and surgical traditionally been linked with the development of ingrown toenails. However, there is a lack of quality evidence supporting options preferred in patients with more severe a single mechanism and ingrown toenail development may be symptoms. However, there is limited evidence triggered by multiple factors. There is ongoing debate about available regarding the effectiveness of non- whether factors relating to the nail itself are responsible for the surgical treatments. Recent evidence suggests that condition or whether the size and shape of the surrounding some surgical techniques are associated with very periungual nail folds are the cause (Figure 1).3 low recurrence rates of the ingrown toenail, and therefore should be considered more often, despite Lunula Proximal nail fold being a more invasive treatment. Lateral nail fold Distal edge of Ingrown toenails primarily affect younger Nail plate Eponychium males Nail plate The Foot Series Cuticle Ingrown toenails, also known as onychocryptosis or unguis incarnates, are a painful condition due to the sides or corner of the toenail digging into the surrounding soft tissue. This Nail plate Matrix results in a breach of the underlying skin and leads to pain, Nail bed inflammation, formation of granulation tissue, and in some cases infection. The most commonly affected area is the lateral Hyponychium edge of the great (big) toe, although the medial edge and other toes can also be affected. -

Results of the Mogensen's Lateral Wedge Resection Technique in The
Eklem Hastalıkları ve Cerrahisi Joint Dis Rel Surg Joint Diseases and Related Surgery Original Article / Çalışma - Araştırma 2007;18(3):116-120 Results of the Mogensen’s lateral wedge resection technique in the treatment of ingrown toenail Ayak tırnak batmasının tedavisinde Mogensen’in lateral kama rezeksiyon tekniğinin sonuçları Ercan Çetinus, M.D.,1 Murat Uzel, M.D.,1 Erkal Bilgiç, M.D.,1 Sezai Şaşmaz, M.D.,2 Özer Arıcan, M.D.,2 Ahmet Karaoğuz, M.D.1 Departments of 1Orthopedics and Traumatology, and 2Dermatology, Medicine Faculty of Kahramanmaraş Sütçü İmam University Objectives: There are many options for the treatment Amaç: Ayak tırnak batmalarında basit konservatif yak- of ingrown toenail, ranging from simple conservative laşımlardan, kapsamlı cerrahi girişimlere kadar birçok approaches to extensive surgical procedures, but stage tedavi seçeneği olmakla birlikte, evre 3 tırnak batmaları 3 ingrown toenails are best treated surgically. The aim en iyi cerrahi olarak tedavi edilmektedir. Bu çalışmada, of this study was to evaluate the results of lateral wedge ayak başparmağında tırnak batması olan bir grup hasta- resection described by Mogensen in patients with ingrown da, Mogensen tarafından tarif edilen lateral kama rezek- toenail of the great toe. siyon tekniğinin sonuçları değerlendirildi. Patients and methods: The study included 21 con- Hastalar ve yöntemler: Ayak başparmağında evre 3 secutive patients (11 females, 10 males; mean age 23±10 tırnak batması nedeniyle 21 ardışık hasta (11 kadın, 10 years; range 12 to 45 years) who were treated with the erkek; ort. yaş 23±10; dağılım 12-45) Mogensen’in late- Mogensen’s lateral wedge resection technique for stage 3 ral kama rezeksiyon tekniği ile tedavi edildi. -

Minor Procedures
MINOR PROCEDURES ELIZABETH BLUNT, RN, PHD, FNP-BC COLLEEN STELLABOTTE, RN, MSN, FNP-BC Today’s Agenda Digital block Subungual hematoma Ingrown toenail management Nail removal Abscess I & D Indication for Digital Blocks •Patients with crush injuries •Need x-rays •Need extensive wound exploration •Tendon injuries requiring evaluation •Multiple lacerations in same digit •Multiple foreign bodies in same digit •Partial or total nail removal Local Anesthetics •Mechanism of action • Infiltrate tissue and diffuse across neural sheaths and membranes • Interfere with neuronal depolarization • Prevent Na influx • No action potential, no nerve impulse •Onset of Action • Technique of injection, concentration, total dose • Knowledge of anatomy is important • Injection between dermis and subcutaneous tissue = immediate anesthesia •Duration of action • Increased with epinephrine • Do not use epinephrine in fingers, toes, nose, penis, ears • Increased with long acting anesthetics such as Bupivicaine and Marcaine Wound Anesthesia GOAL = Reduce Pain and Anxiety • Type of anesthetic used • Needle size 27 or 30-gauge • Inexperienced – start with 25-gauge • 25-gauge or 27-gauge ½-inch needle • pH - buffering • Temperature of solution • Speed and depth of injection Three Major Techniques for Digital Block • Dorsal surface • Indicated when only the nail is involved • Aberrant anatomy may make the technique less than optimal • Web space • Need larger volume of anesthetic • Less control of instillation • Medial/lateral • Focused area of instillation • Volume parameters -

Complicated Onychomycosis and Ingrown Nail: Complex Treatment (Case Series)
Праці НТШ Proc. Shevchenko Sci. Soc. Медичні науки 2017, 2 (L) Medical sciences 2017, 2 (L) Оригінальні дослідження: клінічні науки Research: Clinical sciences УДК 616.577-002.36 COMPLICATED ONYCHOMYCOSIS AND INGROWN NAIL: COMPLEX TREATMENT (CASE SERIES) Oleg Nadashkevitch, Andrij Vergun, Bohdan Parashchuk, Oksana Vergun Danylo Halytsky Lviv National Medical University, Lviv, Ukraine, [email protected] The aim of research is optimal sequence of surgical treatment, local and system therapy after moving away of the staggered nails at destructive onychomycosis, complicated by the secondary ingrown nail for some patients with the complicated mycotic defeat of nails. Materials and methods. Over a fi ve-year period 325 cases of incarnated onychomycosis, 182 cases late relapses of onychocryptosis (after previous surgeries at other clinics) were performed. Patients with such combined pathology got fi ve-day system «pulses» of 400 mg/day itraconazole therapy at a simultaneous use of hepatoprotectors and correction of comorbid pathology. Results. Three variants of dermatophytoma are differentiated: front center – with up to 25% eroded nail – 65 cases, subtotal – from 25 to 70% (without capturing the growth plate) – 138 cases, total – from 70 to 90% (with affected growth plate of the nail) – other cases. Surgical treatment provided in addition to standard decompression stage (complete removal of the nail plate), cutting pathologic eponychial tissues, hypergranulations and dermatophytoma, contained antirecurrent component (partial marginal matrixectomy in the ingrowth area) to prevent from repeated ingrowth. Conclusions. In all cases of mycotic onychocryptosis (secondary ingrown toenail) underwent a comprehensive treatment of comorbid pathology, system therapy of itraconazole to operative treatment (basic onychial defeats sanation) and in a postoperative period, sanation of other nails for prevention of mycotic reinfection was carried out by ciclopirox & amorolfi ne nail lacquer. -

EMBRACE EVERY POSSIBILITY FIRST BLUE LASER in the WORLD for Both Surgery and Therapy
EMBRACE EVERY POSSIBILITY FIRST BLUE LASER IN THE WORLD For Both Surgery and Therapy FIRST BLUE LASER IN THE WORLD WITH 3 WAVELENGTHS FOR SURGERY AND THERAPY K-Laser Blue Derma is a three-wavelength device that mainly exploits the 445 nm one. Unlike all other infra-red lasers, K-Laser is not based on water absorption but rather on the absorption of melanin and haemoglobin. This feature allows obtaining many advantages in the surgical field. Thanks to its higher energy coefficient, compared to infra-red laser, it has increased antiseptic and biostimulating properties. The 445 nm wavelength is combined with 660 nm and 970 nm ones since they support superficial and deep tissue biostimulation. ADVANTAGES: no maintenance, low cost of consumption material and maximum safety. All surgical components can be sterilised. K-Laser Blue Derma: 445 nm - 660 nm - 970 nm Absorption coefficient Absorption 445 660 970 The 445nm wavelength interacts with the molecules at systemic level and is absorbed by both haemoglobin and melanin much better than with an infra-red laser. The blue wavelength is also effective on numerous bacterial strains, 445 nm thus exploiting its antiseptic properties and achieving excellent results in tissues incision, both for surgical and vascular purposes. It is also useful in treating diabetic ulcers and bedsores. The 660nm wavelength can transfer an optimal dosage of energy to the tissue. This energy is thus stored at cellular 660 nm level with subsequent increase in both bacterial proliferation and metabolism. Thus, it allows obtaining remarkable results in the healing of wounds,diabetic and vascular ulcers. -

Virtuwell: How It Works and Conditions Treated (PDF)
How long have How it works you had your symptoms? Just like a doctor’s visit, but online. No video required. No apps to download. No waiting. That’s Virtuwell – your 24/7 online clinic. Step 1 Answer a few questions We guide you through questions online that are straightforward and easy to answer. We’ll ask about your symptoms, medications and allergies too. Step 2 Diagnosis by real people, really fast Board-certified nurse practitioners review your answers, make a diagnosis and recommend the care you’ll need. Prescriptions are sent to your favorite pharmacy. Step 3 Payment & insurance Just enter your credit card, and insurance information if you have it. We’ll submit the insurance claim for you. Step 4 Start feeling better That’s it! In about an hour, you’ll get a text and email the second your treatment plan is ready. Questions? The nurse practitioners are available by phone to help. Our customer service team is always available to listen and help. If you aren’t satisfied, for any reason, we’ll refund your cost. Because we believe happiness is a big part of good health. Learn more at virtuwell.com/how-it-works 16486 (02/02) ©2020 Virtuwell Our services We treat over 60 conditions safely online by asking the same questions you’d hear in a doctor’s office. We treat kids ages 2+ for most conditions. Sinus, Cough & Allergy Skin & Rash Eye & Ear Bronchitis Acne (Age 12+) Ear Infection (Age 5+) Common Cold Athlete’s Foot Eustachian Tube Dysfunction Laryngitis Boils Pink Eye Pet Allergies Burns Stye Seasonal Allergies Canker & Cold Sore Swimmer’s