Accessory Navicular Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proper Preop Makes for Easier Toenail Surgery
April 15, 2007 • www.familypracticenews.com Skin Disorders 25 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS sia using a digital block or a distal approach to take ef- Senior Writer fect. Premedication with NSAIDs, codeine, or dextro- propoxyphene also may be appropriate, he said. WASHINGTON — Proper early management of in- To cut away the offending section of nail, an English grown toenails may help to decrease the risk of recur- anvil nail splitter is inserted under the nail plate and the rence whether or not surgery is necessary, Dr. C. Ralph cut is made all the way to the proximal nail fold. The hy- Daniel III said at the annual meeting of the American pertrophic, granulated tissue should be cut away as well. Academy of Dermatology. Many ingrown toenails are recurrent, so Dr. Daniel per- “An ingrown nail is primarily acting as a foreign-body forms a chemical matricectomy in nearly all patients after reaction. That rigid spicule penetrates soft surrounding tis- making sure that the surgical field is dry and bloodless. sue” and produces swelling, granulation tissue, and some- The proximal nail fold can be flared back to expose more times a secondary infection, said Dr. Daniel of the de- of the proximal matrix if necessary. Dr. Daniel inserts a Cal- partments of dermatology at the University of Mississippi, giswab coated with 88% phenol or 10% sodium hydroxide Jackson, and the University of Alabama, Birmingham. and applies the chemical for 30 seconds to the portion of For the early management of stage I ingrown toenails the nail matrix that needs to be destroyed. -

The Nearly Invisible Intraneural Cyst: a New and Emerging Part of the Spectrum
NEUROSURGICAL FOCUS Neurosurg Focus 42 (3):E10, 2017 The nearly invisible intraneural cyst: a new and emerging part of the spectrum Thomas J. Wilson, MD,1 Marie-Noëlle Hébert-Blouin, MD,2 Naveen S. Murthy, MD,3 Joaquín J. García, MD,4 Kimberly K. Amrami, MD,3 and Robert J. Spinner, MD1 Departments of 1Neurosurgery, 3Radiology, and 4Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota; and 2Department of Neurosurgery, McGill University Health Centre, Montreal, Quebec, Canada OBJECTIVE The authors have observed that a subset of patients referred for evaluation of peroneal neuropathy with “negative” findings on MRI of the knee have subtle evidence of a peroneal intraneural ganglion cyst on subsequent closer inspection. The objective of this study was to introduce the nearly invisible peroneal intraneural ganglion cyst and provide illustrative cases. The authors further wanted to identify clues to the presence of a nearly invisible cyst. METHODS Illustrative cases demonstrating nearly invisible peroneal intraneural ganglion cysts were retrospectively reviewed and are presented. Case history and physical examination, imaging, and intraoperative findings were reviewed for each case. The outcomes of interest were the size and configuration of peroneal intraneural ganglion cysts over time, relative to various interventions that were performed, and in relation to physical examination and electrodiagnostic find- ings. RESULTS The authors present a series of cases that highlight the dynamic nature of peroneal intraneural ganglion cysts and introduce the nearly invisible cyst as a new and emerging part of the spectrum. The cases demonstrate changes in size and morphology over time of both the intraneural and extraneural compartments of these cysts. -

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

Nail Problems
Nail Problems Components of the Nail Congenital Disorders Racket nails, characterized by a broad short thumb nail, is the commonest congenital nail defect, dominantly inherited and seen in 1% of the population. The basic abnormality is shortness of the underlying terminal phalanx. In the yellow nail syndrome, the nail changes begin in adult life, against a background of hypoplasia of the lymphatic system. Peripheral edema is usually present and pleural effusions may occur. The nails grow very slowly and become thickened and greenish-yellow; their surface is smooth but they are over curved from side to side. Acquired Nail Changes Beau's Lines Transverse lines or grooves in nail. Causes include any severe systemic illness or medications (chemotherapy), which affects growth of the nail matrix. Clinically: The grooves or lines move distally; the distance from the nail fold lets one assess the time of trauma. Onycholysis Separation of nail from nail bed. Causes include psoriasis, dermatitis, fungal infections; medications (photo-onycholysis from tetracyclines or psoralens), thyroid disease; rarely inherited. Idiopathic onycholysis is most common among women; painless separation of nail without apparent cause. Typically, the distal third separates and underlying nail bed becomes darker and thickened. Therapy: Cut nail very short to reduce leverage encouraging separation, apply antifungal solution. Usually self-limited process. Ingrown Nail Penetration of nail plate into tissue of lateral nail fold. Almost always involves great toes. Causes include congenital malformation of nail (pincer nail), improper trimming, and tightly fitting shoes. Clinically: Distorted nail with swelling, pain, and granulation tissue along the lateral nail fold. Therapy: Mild cases: Eliminate pressure, trim nail; topical antiseptics as foot soaks or on small piece of cotton wool pushed under affected nail. -

Original Article Pictorial Atlas of Symptomatic Accessory Ossicles by 18F-Sodium Fluoride (Naf) PET-CT
Am J Nucl Med Mol Imaging 2017;7(6):275-282 www.ajnmmi.us /ISSN:2160-8407/ajnmmi0069278 Original Article Pictorial atlas of symptomatic accessory ossicles by 18F-Sodium Fluoride (NaF) PET-CT Sharjeel Usmani1, Cherry Sit2, Gopinath Gnanasegaran2, Tim Van den Wyngaert3, Fahad Marafi4 1Department of Nuclear Medicine & PET/CT Imaging, Kuwait Cancer Control Center, Khaitan, Kuwait; 2Royal Free Hospital NHS Trust, London, UK; 3Antwerp University Hospital, Belgium; 4Jaber Al-Ahmad Molecular Imaging Center, Kuwait Received August 7, 2017; Accepted December 15, 2017; Epub December 20, 2017; Published December 30, 2017 Abstract: Accessory ossicles are developmental variants which are often asymptomatic. When incidentally picked up on imaging, they are often inconsequential and rarely a cause for concern. However, they may cause pain or discomfort due to trauma, altered stress, and over-activity. Nuclear scintigraphy may play a role in the diagnosis and localizing pain generators. 18F-Sodium Fluoride (NaF) is a PET imaging agent used in bone imaging. Although commonly used in imaging patients with cancer imaging malignancy, 18F-NaF may be useful in the evaluation of benign bone and joint conditions. In this article, we would like to present a spectrum of clinical cases and review the potential diagnostic utility of 18F-NaF in the assessment of symptomatic accessory ossicles in patients referred for staging cancers. Keywords: 18F-NaF PET/CT, accessory ossicles, hybrid imaging Introduction Accessory ossicles are developmental variants which are often asymptomatic. When inciden- Bone and joint pain is a common presentation tally picked up on imaging, they are often incon- in both primary and secondary practice. -

The Pathomechanics of Plantar Fasciitis
Sports Med 2006; 36 (7): 585-611 REVIEW ARTICLE 0112-1642/06/0007-0585/$39.95/0 2006 Adis Data Information BV. All rights reserved. The Pathomechanics of Plantar Fasciitis Scott C. Wearing,1 James E. Smeathers,1 Stephen R. Urry,1 Ewald M. Hennig2 and Andrew P. Hills1 1 Institute of Health and Biomedical Innovation, Queensland University of Technology, Kelvin Grove, Queensland, Australia 2 Biomechanik Labor, University Duisburg-Essen, Essen, Germany Contents Abstract ....................................................................................585 1. Anatomy of the Plantar Fascia ............................................................586 1.1 Gross Anatomy of the Plantar Fascia...................................................586 1.2 Histological Anatomy of the Plantar Fascia .............................................589 1.2.1 Neuroanatomy ................................................................590 1.2.2 Microcirculation ...............................................................590 1.2.3 The Enthesis ...................................................................590 2. Mechanical Properties of the Plantar Fascia ................................................592 2.1 Structural Properties ..................................................................593 2.2 Material Properties ...................................................................593 3. Mechanical Function of the Plantar Fascia .................................................594 3.1 Quasistatic Models of Plantar Fascial Function ..........................................594 -

White Lesions of the Oral Cavity and Derive a Differential Diagnosis Four for Various White Lesions
2014 self-study course four course The Ohio State University College of Dentistry is a recognized provider for ADA, CERP, and AGD Fellowship, Mastership and Maintenance credit. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at www.ada.org/goto/cerp. The Ohio State University College of Dentistry is approved by the Ohio State Dental Board as a permanent sponsor of continuing dental education ABOUT this FREQUENTLY asked COURSE… QUESTIONS… Q: Who can earn FREE CE credits? . READ the MATERIALS. Read and review the course materials. A: EVERYONE - All dental professionals in your office may earn free CE contact . COMPLETE the TEST. Answer the credits. Each person must read the eight question test. A total of 6/8 course materials and submit an questions must be answered correctly online answer form independently. for credit. us . SUBMIT the ANSWER FORM Q: What if I did not receive a ONLINE. You MUST submit your confirmation ID? answers ONLINE at: A: Once you have fully completed your p h o n e http://dent.osu.edu/sterilization/ce answer form and click “submit” you will be directed to a page with a . RECORD or PRINT THE 614-292-6737 unique confirmation ID. CONFIRMATION ID This unique ID is displayed upon successful submission Q: Where can I find my SMS number? of your answer form. -

Issue # 157 28 June 2019 Cold Feet to Return to ITV for a Ninth Series
04/08/2020 Media Weekly Broadcast Issue # 157 28 June 2019 Cold Feet to return to ITV for a ninth series ITV confirmed that BAFTA winning comedy drama, Cold Feet, has been recommissioned for a ninth series from acclaimed creator and writer Mike Bullen and award-winning producers Big Talk Productions. Six further episodes of the Manchester-based series will begin shooting later this year. The Association of Commercial Read more Television in Europe (ACT) is a trade body for the commercial broadcasting sector in Europe. Formed in 1989, the ACT has 27 member companies active in 37 Mediaset’s online channel TgCom24 is the European countries, operating and distributing several most followed online newsroom in Italy thousand free-to-air and pay-tv channels and new media services. With 13% of Italian viewers accessing it at least three times a week and 24% visiting it in the last week, Mediaset’s channel TgCom24 ranks number one online newsroom in Italy in 2019. Looking at the Groups’s news channels as a whole, Mediaset is the favoured choice for 74% of Italians viewers. As trust in online news is undermined by the disinformation phenomenon, Mediaset proves to be a reliable source of information for its viewers. Read more RTL Group: My Brilliant Achievement On 18 June 2019, My Brilliant Friend, a production from Fremantle label Wildside, won the outstanding Drama TV Series award at the 2019 Golden Nymph awards in Monte Carlo. oy99madskp.preview.infomaniak.website/oldsite/acte.be/_old/newsletters/164/50/Issue-157bf6b.html?cntnt01template=webversion-newsletter 1/3 04/08/2020 Media Weekly Broadcast Read more Sky awards £125,000 to five new Women in Technology Scholars Sky has announced its second cohort of Women in Technology Scholars, awarding five talented women a total of £125,000 to accelerate a business idea which harnesses technology innovation. -
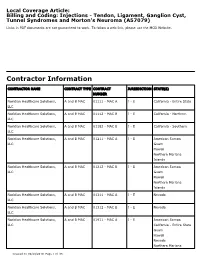
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Foot Pain in Scleroderma
Foot Pain in Scleroderma Dr Begonya Alcacer-Pitarch LMBRU Postdoctoral Research Fellow 20th Anniversary Scleroderma Family Day 16th May 2015 Leeds Institute of Rheumatic and Musculoskeletal Medicine Presentation Content n Introduction n Different types of foot pain n Factors contributing to foot pain n Impact of foot pain on Quality of Life (QoL) Leeds Institute of Rheumatic and Musculoskeletal Medicine Scleroderma n Clinical features of scleroderma – Microvascular (small vessel) and macrovascular (large vessel) damage – Fibrosis of the skin and internal organs – Dysfunction of the immune system n Unknown aetiology n Female to male ratio 4.6 : 1 n The prevalence of SSc in the UK is 8.21 per 100 000 Leeds Institute of Rheumatic and Musculoskeletal Medicine Foot Involvement in SSc n Clinically 90% of SSc patients have foot involvement n It typically has a later involvement than hands n Foot involvement is less frequent than hand involvement, but is potentially disabling Leeds Institute of Rheumatic and Musculoskeletal Medicine Different Types of Foot Pain Leeds Institute of Rheumatic and Musculoskeletal Medicine Ischaemic Pain (vascular) Microvascular disease (small vessel) n Intermittent pain – Raynaud’s (spasm) • Cold • Throb • Numb • Tingle • Pain n Constant pain – Vessel center narrows • Distal pain (toes) • Gradually increasing pain • Intolerable pain when necrosis is present Leeds Institute of Rheumatic and Musculoskeletal Medicine Ischaemic Pain (vascular) Macrovascular disease (large vessels) n Intermittent and constant pain – Peripheral Arterial Disease • Intermittent claudication – Muscle pain (ache, cramp) during walking • Aching or burning pain • Night and rest pain • Cramps Leeds Institute of Rheumatic and Musculoskeletal Medicine Ulcer Pain n Ulcer development – Constant pain n Infected ulcer – Unexpected/ excess pain or tenderness Leeds Institute of Rheumatic and Musculoskeletal Medicine Neuropathic Pain n Nerve damage is not always obvious. -

December 2018 When Cold Feet Isn’T Just Nerves
CALL US TODAY – 407-339-7759 • 352-589-9550 (LAKE CO.) News and Updates December 2018 When Cold Feet Isn’t Just Nerves People often talk about cold feet in terms of walking down the aisle or engaging in a stressful event, but what’s going on when your feet just feel cold for seemingly no reason? Many causes of cold feet are nothing to worry about, but others can be sign of an underlying problem. It pays to talk with a podiatrist about your condition if it keeps returning or causes you concerns for other reasons. Among the most common causes of cold feet is poor circulation. The feet, being far from your heart, already have a bigger challenge receiving warm blood fl ow. If a condition is causing your general circulation to be slower, your feet will be among the fi rst to feel it. A potential cause of interrupted circulation is Raynaud’s phenomenon which causes blood vessels in the hands and/or feet to suddenly constrict and spasm, reducing blood fl ow. While sometimes associated with another condition, Raynaud’s phenomenon can also happen entirely on its own to an otherwise healthy person. Also, in some cases, certain medications can mimic this effect. If you are sensing cold, but your feet don’t actually feel cold to the touch, that may be the sign that something is amiss neurologically. The nerves that sense temperature may not be operating as they should and damaged in some way (neuropathy). If that cold feeling also comes with tingling or numbness, the odds of a nerve problem become even more likely.