Juvenile Spondyloarthropathies: Inflammation in Disguise
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Understanding Entheseal Changes: Definition and Life Course Changes Sébastien Villotte, Christopher J
Understanding Entheseal Changes: Definition and Life Course Changes Sébastien Villotte, Christopher J. Knüsel To cite this version: Sébastien Villotte, Christopher J. Knüsel. Understanding Entheseal Changes: Definition and Life Course Changes. International Journal of Osteoarchaeology, Wiley, 2013, Entheseal Changes and Occupation: Technical and Theoretical Advances and Their Applications, 23 (2), pp.135-146. 10.1002/oa.2289. hal-03147090 HAL Id: hal-03147090 https://hal.archives-ouvertes.fr/hal-03147090 Submitted on 19 Feb 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. International Journal of Osteoarchaeology Understanding Entheseal Changes: Definition and Life Course Changes Journal: International Journal of Osteoarchaeology Manuscript ID: OA-12-0089.R1 Wiley - ManuscriptFor type: Commentary Peer Review Date Submitted by the Author: n/a Complete List of Authors: Villotte, Sébastien; University of Bradford, AGES Knusel, Chris; University of Exeter, Department of Archaeology entheses, enthesopathy, Musculoskeletal Stress Markers (MSM), Keywords: senescence, activity, hormones, animal models, clinical studies http://mc.manuscriptcentral.com/oa Page 1 of 27 International Journal of Osteoarchaeology 1 2 3 Title: 4 5 Understanding Entheseal Changes: Definition and Life Course Changes 6 7 8 Short title: 9 10 Understanding Entheseal Changes 11 12 13 Keywords: entheses; enthesopathy; Musculoskeletal Stress Markers (MSM); senescence; 14 15 activity; hormones; animal models; clinical studies 16 17 18 Authors: For Peer Review 19 20 Villotte S. -
Evicore Spine Imaging Guidelines
CLINICAL GUIDELINES Spine Imaging Policy Version 1.0 Effective February 14, 2020 eviCore healthcare Clinical Decision Support Tool Diagnostic Strategies: This tool addresses common symptoms and symptom complexes. Imaging requests for individuals with atypical symptoms or clinical presentations that are not specifically addressed will require physician review. Consultation with the referring physician, specialist and/or individual’s Primary Care Physician (PCP) may provide additional insight. CPT® (Current Procedural Terminology) is a registered trademark of the American Medical Association (AMA). CPT® five digit codes, nomenclature and other data are copyright 2017 American Medical Association. All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in the CPT® book. AMA does not directly or indirectly practice medicine or dispense medical services. AMA assumes no liability for the data contained herein or not contained herein. © 2019 eviCore healthcare. All rights reserved. Spine Imaging Guidelines V1.0 Spine Imaging Guidelines Procedure Codes Associated with Spine Imaging 3 SP-1: General Guidelines 5 SP-2: Imaging Techniques 14 SP-3: Neck (Cervical Spine) Pain Without/With Neurological Features (Including Stenosis) and Trauma 22 SP-4: Upper Back (Thoracic Spine) Pain Without/With Neurological Features (Including Stenosis) and Trauma 26 SP-5: Low Back (Lumbar Spine) Pain/Coccydynia without Neurological Features 28 SP-6: Lower Extremity Pain with Neurological Features (Radiculopathy, Radiculitis, or Plexopathy and Neuropathy) With or Without Low Back (Lumbar Spine) Pain 32 SP-7: Myelopathy 36 SP-8: Lumbar Spine Spondylolysis/Spondylolisthesis 39 SP-9: Lumbar Spinal Stenosis 42 SP-10: Sacro-Iliac (SI) Joint Pain, Inflammatory Spondylitis/Sacroiliitis and Fibromyalgia 44 SP-11: Pathological Spinal Compression Fractures 47 SP-12: Spinal Pain in Cancer Patients 49 SP-13: Spinal Canal/Cord Disorders (e.g. -
Uncontrolled Gout Fact Sheet
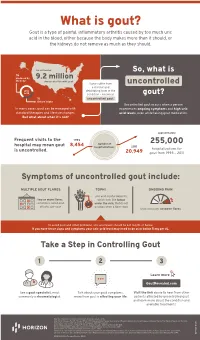
What is gout? Gout is a type of painful, inflammatory arthritis caused by too much uric acid in the blood, either because the body makes more than it should, or the kidneys do not remove as much as they should. An estimated So, what is ⅔ produced by 9.2 million the body Americans live with gout Some suffer from uncontrolled a chronic and uric debilitating form of the acid condition – known as gout? ⅓ uncontrolled gout. dietary intake Uncontrolled gout occurs when a person In many cases, gout can be managed with experiences ongoing symptoms and high uric standard therapies and lifestyle changes. acid levels, even while taking gout medication. But what about when it’s not? approximately Frequent visits to the 1993 number of 255,000 hospital may mean gout 8,454 hospitalizations 2011 is uncontrolled. hospitalizations for 20,949 gout from 1993 – 2011 Symptoms of uncontrolled gout include: MULTIPLE GOUT FLARES TOPHI ONGOING PAIN uric acid crystal deposits, two or more flares, which look like lumps sometimes called gout under the skin, that do not attacks, per year go away when a flare stops that continues between flares To avoid gout and other problems, uric acid levels should be 6.0 mg/dL or below. If you have these signs and symptoms your uric acid level may need to be at or below 5 mg per dL. Take a Step in Controlling Gout 1 2 3 Learn more GoutRevealed.com See a gout specialist, most Talk about your gout symptoms, Visit the link above to hear from other commonly a rheumatologist. -

Atraumatic Bilateral Achilles Tendon Rupture: an Association of Systemic
378 Kotnis, Halstead, Hormbrey Acute compartment syndrome may be a of the body of gastrocnemius has been result of any trauma to the limb. The trauma is reported in athletes.7 8 This, however, is the J Accid Emerg Med: first published as 10.1136/emj.16.5.378 on 1 September 1999. Downloaded from usually a result of an open or closed fracture of first reported case of acute compartment the bones, or a crush injury to the limb. Other syndrome caused by a gastrocnemius muscle causes include haematoma, gun shot or stab rupture in a non-athlete. wounds, animal or insect bites, post-ischaemic swelling, vascular damage, electrical injuries, burns, prolonged tourniquet times, etc. Other Conclusion causes of compartment syndrome are genetic, Soft tissue injuries and muscle tears occur fre- iatrogenic, or acquired coagulopathies, infec- quently in athletes. Most injuries result from tion, nephrotic syndrome or any cause of direct trauma. Indirect trauma resulting in decreased tissue osmolarity and capillary per- muscle tears and ruptures can cause acute meability. compartment syndrome in athletes. It is also Chronic compartment syndrome is most important to keep in mind the possibility of typically an exercise induced condition charac- similar injuries in a non-athlete as well. More terised by a relative inadequacy of musculofas- research is needed to define optimal manage- cial compartment size producing chronic or ment patterns and potential strategies for recurring pain and/or disability. It is seen in injury prevention. athletes, who often have recurring leg pain that Conflict of interest: none. starts after they have been exercising for some Funding: none. -

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

Etiopathogenesis of Sacroiliitis
Korean J Pain 2020;33(4):294-304 https://doi.org/10.3344/kjp.2020.33.4.294 pISSN 2005-9159 eISSN 2093-0569 Review Article Etiopathogenesis of sacroiliitis: implications for assessment and management Manuela Baronio1, Hajra Sadia2, Stefano Paolacci3, Domenico Prestamburgo4, Danilo Miotti5, Vittorio A. Guardamagna6, Giuseppe Natalini1, and Matteo Bertelli3,7,8 1Dipartimento di Anestesia, Rianimazione, Terapia Intensiva e del Dolore, Fondazione Poliambulanza, Brescia, Italy 2Atta-ur-Rahman School of Applied Biosciences, National University of Science and Technology, Islamabad, Pakistan 3MAGI’s Lab, Rovereto, Italy 4Ortopedia e Traumatologia, Ospedali Civili di Legnano e Cuggiono, Cuggiono, Italy 5Cure Palliative e Terapia del Dolore, ICS Maugeri, Pavia, Italy 6Cure Palliative e Terapia del Dolore, IRCCS IEO, Milano, Italy 7MAGI Euregio, Bolzano, Italy 8EBTNA-LAB, Rovereto, Italy Received January 16, 2020 Revised March 17, 2020 The sacroiliac joints connect the base of the sacrum to the ilium. When inflamed, Accepted April 16, 2020 they are suspected to cause low back pain. Inflammation of the sacroiliac joints is called sacroiliitis. The severity of the pain varies and depends on the degree of Handling Editor: Kyung Hoon Kim inflammation. Sacroiliitis is a hallmark of seronegative spondyloarthropathies. The presence or absence of chronic sacroiliitis is an important clue in the diagnosis of Correspondence low back pain. This article aims to provide a concise overview of the anatomy, physi- Stefano Paolacci ology, and molecular biology of sacroiliitis to aid clinicians in the assessment and MAGI’s Lab, Via delle Maioliche, 57/D, management of sacroiliitis. For this narrative review, we evaluated articles in Eng- Rovereto, Trentino 38068, Italy lish published before August 2019 in PubMed. -

9 Impingement and Rotator Cuff Disease
Impingement and Rotator Cuff Disease 121 9 Impingement and Rotator Cuff Disease A. Stäbler CONTENTS Shoulder pain and chronic reduced function are fre- quently heard complaints in an orthopaedic outpa- 9.1 Defi nition of Impingement Syndrome 122 tient department. The symptoms are often related to 9.2 Stages of Impingement 123 the unique anatomic relationships present around the 9.3 Imaging of Impingement Syndrome: Uri Imaging Modalities 123 glenohumeral joint ( 1997). Impingement of the 9.3.1 Radiography 123 rotator cuff and adjacent bursa between the humeral 9.3.2 Ultrasound 126 head and the coracoacromial arch are among the most 9.3.3 Arthrography 126 common causes of shoulder pain. Neer noted that 9.3.4 Magnetic Resonance Imaging 127 elevation of the arm, particularly in internal rotation, 9.3.4.1 Sequences 127 9.3.4.2 Gadolinium 128 causes the critical area of the cuff to pass under the 9.3.4.3 MR Arthrography 128 coracoacromial arch. In cadaver dissections he found 9.4 Imaging Findings in Impingement Syndrome alterations attributable to mechanical impingement and Rotator Cuff Tears 130 including a ridge of proliferative spurs and excres- 9.4.1 Bursal Effusion 130 cences on the undersurface of the anterior margin 9.4.2 Imaging Following Impingement Test Injection 131 Neer Neer 9.4.3 Tendinosis 131 of the acromion ( 1972). Thus it was who 9.4.4 Partial Thickness Tears 133 introduced the concept of an impingement syndrome 9.4.5 Full-Thickness Tears 134 continuum ranging from chronic bursitis and partial 9.4.5.1 Subacromial Distance 136 tears to complete tears of the supraspinatus tendon, 9.4.5.2 Peribursal Fat Plane 137 which may extend to involve other parts of the cuff 9.4.5.3 Intramuscular Cysts 137 Neer Matsen 9.4.6 Massive Tears 137 ( 1972; 1990). -

Bursae Around the Knee Joints Priyank S Chatra Department of Radiology, Yenepoya Medical College, Mangalore, Karnataka, India
MUSCULOSKELETAL RADIOLOGY Bursae around the knee joints Priyank S Chatra Department of Radiology, Yenepoya Medical College, Mangalore, Karnataka, India Correspondence: Dr. Priyank S. Chatra, Department of Radiology, Yenepoya Medical College, Deralakatte, Mangalore – 575 018, Karnataka, India. E-mail: [email protected] Abstract A bursa is a fluid-filled structure that is present between the skin and tendon or tendon and bone. The main function of a bursa is to reduce friction between adjacent moving structures. Bursae around the knee can be classified as those around the patella and those that occur elsewhere. In this pictorial essay we describe the most commonly encountered lesions and their MRI appearance. Key words: Iliotibial bursa; infrapatellar bursa; pes anserine bursa Introduction and the gastrocnemius-semimembranosus bursa. On MRI imaging, bursitis appears as an oblong fluid collection in A bursa is a fluid-filled structure that is present between its expected anatomical location. the skin and tendon or tendon and bone. The main function of a bursa is to reduce friction between adjacent Prepatellar Bursitis moving structures. Typically, bursae are located around large joints such as the shoulder, knee, hip, and elbow.[1] The prepatellar bursa is located between the patella and the Inflammation of this fluid-filled structure is called bursitis. overlying subcutaneous tissue. Chronic trauma in the form Trauma, infection, overuse, and hemorrhage are some of prolonged or repeated kneeling leads to inflammation of the common -

Arthritis (Overview)
ARTHRITIS Having arthritis can significantly affect your comfort & ability to walk and move with confidence. This is because it affects your joints, which are responsible for keeping you steady and moving efficiently. Your symptoms and causes will depend on the type of arthritis that you have. At Masterton Foot Clinic, our podiatrists work closely with patients with four types of arthritis. OSTEOARTHRITIS Osteoarthritis is the wear and tear arthritis that develops slowly over time as the cartilage that covers your bone ends wears down. The cause is largely from natural use over many years, though injuries, alignment issues within the joint and other diseases may result in it developing at a faster rate. We work with patients that want to feel more comfortable on their feet, despite having arthritis in their hip, knee, ankle and foot joints. RHEUMATOID ARTHRITIS Rheumatoid arthritis is an autoimmune disease that affects the joints. It occurs when your body’s immune system attacks the joints and causes damage, inflammation and pain. If the effects of rheumatoid arthritis remain uncontrolled, it can cause permanent changes in the appearance of the joints, especially at the feet and hands. We work with patients to help them manage the discomfort associated with rheumatoid arthritis, offloading prominent and painful areas that have developed due to changes in the joints. GOUT Gout is an inflammatory arthritis that results from a high concentration of uric acid in the blood. It is associated with a high intake of purine-containing foods like red meats, shellfish and red wine, hence it was previously referred to as the rich man’s disease. -

The Pathomechanics of Plantar Fasciitis
Sports Med 2006; 36 (7): 585-611 REVIEW ARTICLE 0112-1642/06/0007-0585/$39.95/0 2006 Adis Data Information BV. All rights reserved. The Pathomechanics of Plantar Fasciitis Scott C. Wearing,1 James E. Smeathers,1 Stephen R. Urry,1 Ewald M. Hennig2 and Andrew P. Hills1 1 Institute of Health and Biomedical Innovation, Queensland University of Technology, Kelvin Grove, Queensland, Australia 2 Biomechanik Labor, University Duisburg-Essen, Essen, Germany Contents Abstract ....................................................................................585 1. Anatomy of the Plantar Fascia ............................................................586 1.1 Gross Anatomy of the Plantar Fascia...................................................586 1.2 Histological Anatomy of the Plantar Fascia .............................................589 1.2.1 Neuroanatomy ................................................................590 1.2.2 Microcirculation ...............................................................590 1.2.3 The Enthesis ...................................................................590 2. Mechanical Properties of the Plantar Fascia ................................................592 2.1 Structural Properties ..................................................................593 2.2 Material Properties ...................................................................593 3. Mechanical Function of the Plantar Fascia .................................................594 3.1 Quasistatic Models of Plantar Fascial Function ..........................................594 -

'Dialysis Related Arthropathy': a Survey of 95 Patients Receiving Chronic Haemodialysis with Special Reference to 132 Microglobulin Related Amyloidosis
Ann Rheum Dis: first published as 10.1136/ard.48.5.409 on 1 May 1989. Downloaded from Annals of the Rheumatic Diseases, 1989; 48, 409-420 'Dialysis related arthropathy': a survey of 95 patients receiving chronic haemodialysis with special reference to 132 microglobulin related amyloidosis N P HURST,' R VAN DEN BERG,' A DISNEY,2 M ALCOCK,3 L ALBERTYN,3 M GREEN,' AND V PASCOE4 From the 'Rheumatology Unit, the 2Renal Unit, the 3Department of Radiology, and the 4Department of Pathology, The Queen Elizabeth Hospital, Woodville, South Australia SUMMARY Ninety five patients receiving chronic haemodialysis (CHD) were surveyed to determine the prevalence of rheumatic disease and, where possible, its aetiology. At least three distinct rheumatic syndromes were identified-a group of patients with a syndrome consisting of large and medium joint synovial swelling, restricted hips and shoulders, tenosynovitis, carpal tunnel syndrome, and bone cysts due to deposition of 132 microglobulin related amyloid (AMP2m); a second group with erosive azotaemic osteoarthropathy; and a third group with age related degenerative disease of small, large, and axial joints. The data presented suggest that in patients receiving CHD (a) the prevalence of AM2i2m deposition and the associated syndrome increases with duration of dialysis, but in patients who have been dialysed for more than 10 years the risk of developing AM2n2m is related to age; (b) AM2i2m deposition in subchondral cysts, but not synovium, causes joint destruction; also, AMp2m may be more prone to deposition in synovium of joints already damaged by other processes; (c) in the absence of synovial iron deposition synovial AM2n2m is not associated with an inflammatory infiltrate; (d) hyperparathyroidism and perhaps other factors such as synovial iron deposition are probably more important than AMgi2m as causes http://ard.bmj.com/ of peripheral joint degeneration and destructive spondyloarthropathy in patients receiving CHD. -

New ASAS Criteria for the Diagnosis of Spondyloarthritis: Diagnosing Sacroiliitis by Magnetic Resonance Imaging 9
Document downloaded from http://www.elsevier.es, day 10/02/2016. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. Radiología. 2014;56(1):7---15 www.elsevier.es/rx UPDATE IN RADIOLOGY New ASAS criteria for the diagnosis of spondyloarthritis: ଝ Diagnosing sacroiliitis by magnetic resonance imaging ∗ M.E. Banegas Illescas , C. López Menéndez, M.L. Rozas Rodríguez, R.M. Fernández Quintero Servicio de Radiodiagnóstico, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain Received 17 January 2013; accepted 10 May 2013 Available online 11 March 2014 KEYWORDS Abstract Radiographic sacroiliitis has been included in the diagnostic criteria for spondy- Sacroiliitis; loarthropathies since the Rome criteria were defined in 1961. However, in the last ten years, Diagnosis; magnetic resonance imaging (MRI) has proven more sensitive in the evaluation of the sacroiliac Magnetic resonance joints in patients with suspected spondyloarthritis and symptoms of sacroiliitis; MRI has proven imaging; its usefulness not only for diagnosis of this disease, but also for the follow-up of the disease and Axial spondy- response to treatment in these patients. In 2009, The Assessment of SpondyloArthritis inter- loarthropathies national Society (ASAS) developed a new set of criteria for classifying and diagnosing patients with spondyloarthritis; one important development with respect to previous classifications is the inclusion of MRI positive for sacroiliitis as a major diagnostic criterion. This article focuses on the radiologic part of the new classification. We describe and illustrate the different alterations that can be seen on MRI in patients with sacroiliitis, pointing out the limitations of the technique and diagnostic pitfalls.