HV Chapter 33-Nail Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proper Preop Makes for Easier Toenail Surgery
April 15, 2007 • www.familypracticenews.com Skin Disorders 25 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS sia using a digital block or a distal approach to take ef- Senior Writer fect. Premedication with NSAIDs, codeine, or dextro- propoxyphene also may be appropriate, he said. WASHINGTON — Proper early management of in- To cut away the offending section of nail, an English grown toenails may help to decrease the risk of recur- anvil nail splitter is inserted under the nail plate and the rence whether or not surgery is necessary, Dr. C. Ralph cut is made all the way to the proximal nail fold. The hy- Daniel III said at the annual meeting of the American pertrophic, granulated tissue should be cut away as well. Academy of Dermatology. Many ingrown toenails are recurrent, so Dr. Daniel per- “An ingrown nail is primarily acting as a foreign-body forms a chemical matricectomy in nearly all patients after reaction. That rigid spicule penetrates soft surrounding tis- making sure that the surgical field is dry and bloodless. sue” and produces swelling, granulation tissue, and some- The proximal nail fold can be flared back to expose more times a secondary infection, said Dr. Daniel of the de- of the proximal matrix if necessary. Dr. Daniel inserts a Cal- partments of dermatology at the University of Mississippi, giswab coated with 88% phenol or 10% sodium hydroxide Jackson, and the University of Alabama, Birmingham. and applies the chemical for 30 seconds to the portion of For the early management of stage I ingrown toenails the nail matrix that needs to be destroyed. -

Nail Problems
Nail Problems Components of the Nail Congenital Disorders Racket nails, characterized by a broad short thumb nail, is the commonest congenital nail defect, dominantly inherited and seen in 1% of the population. The basic abnormality is shortness of the underlying terminal phalanx. In the yellow nail syndrome, the nail changes begin in adult life, against a background of hypoplasia of the lymphatic system. Peripheral edema is usually present and pleural effusions may occur. The nails grow very slowly and become thickened and greenish-yellow; their surface is smooth but they are over curved from side to side. Acquired Nail Changes Beau's Lines Transverse lines or grooves in nail. Causes include any severe systemic illness or medications (chemotherapy), which affects growth of the nail matrix. Clinically: The grooves or lines move distally; the distance from the nail fold lets one assess the time of trauma. Onycholysis Separation of nail from nail bed. Causes include psoriasis, dermatitis, fungal infections; medications (photo-onycholysis from tetracyclines or psoralens), thyroid disease; rarely inherited. Idiopathic onycholysis is most common among women; painless separation of nail without apparent cause. Typically, the distal third separates and underlying nail bed becomes darker and thickened. Therapy: Cut nail very short to reduce leverage encouraging separation, apply antifungal solution. Usually self-limited process. Ingrown Nail Penetration of nail plate into tissue of lateral nail fold. Almost always involves great toes. Causes include congenital malformation of nail (pincer nail), improper trimming, and tightly fitting shoes. Clinically: Distorted nail with swelling, pain, and granulation tissue along the lateral nail fold. Therapy: Mild cases: Eliminate pressure, trim nail; topical antiseptics as foot soaks or on small piece of cotton wool pushed under affected nail. -

Nail Anatomy and Physiology for the Clinician 1
Nail Anatomy and Physiology for the Clinician 1 The nails have several important uses, which are as they are produced and remain stored during easily appreciable when the nails are absent or growth. they lose their function. The most evident use of It is therefore important to know how the fi ngernails is to be an ornament of the hand, but healthy nail appears and how it is formed, in we must not underestimate other important func- order to detect signs of pathology and understand tions, such as the protective value of the nail plate their pathogenesis. against trauma to the underlying distal phalanx, its counterpressure effect to the pulp important for walking and for tactile sensation, the scratch- 1.1 Nail Anatomy ing function, and the importance of fi ngernails and Physiology for manipulation of small objects. The nails can also provide information about What we call “nail” is the nail plate, the fi nal part the person’s work, habits, and health status, as of the activity of 4 epithelia that proliferate and several well-known nail features are a clue to sys- differentiate in a specifi c manner, in order to form temic diseases. Abnormal nails due to biting or and protect a healthy nail plate [1 ]. The “nail onychotillomania give clues to the person’s emo- unit” (Fig. 1.1 ) is composed by: tional/psychiatric status. Nail samples are uti- • Nail matrix: responsible for nail plate production lized for forensic and toxicology analysis, as • Nail folds: responsible for protection of the several substances are deposited in the nail plate nail matrix Proximal nail fold Nail plate Fig. -

Proper Preop Makes for Easier Toenail Surgery
20 Dermatologic Surgery S KIN & ALLERGY N EWS • April 2007 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS produces swelling, granulation tissue, and tor or a 1- to 2-mm curette. has served as a speaker, consultant, and in- Senior Writer sometimes a secondary infection, said Dr. He also uses a technique for early-stage vestigator for the company. Daniel of the departments of dermatol- ingrown toenails in which dental floss is in- A procedure that uses an acrylic-affixed WASHINGTON — Proper early man- ogy at the University of Mississippi, Jack- serted under the ingrown nail corner with- gutter splint has been reported to be suc- agement of ingrown toenails may help to son, and the University of Alabama, Birm- out anesthesia and is kept there to separate cessful for avoiding surgery, Dr. Daniel decrease the risk of recurrence whether or ingham. the nail edge from adjacent soft tissue (J. said. A plastic gutter tube is set under the not surgery is necessary, Dr. C. Ralph For the early management of stage I in- Am. Acad. Dermatol. 2004;50:939-40). ingrown part of the nail and acrylic is Daniel III said at the annual meeting of the grown toenails in which some granula- Dr. Daniel formerly was on the board of sculpted and allowed to polymerize American Academy of Dermatology. tion tissue but no infection is present, Dr. directors for Doak Dermatologics, a sub- around the ingrown part of the nail and “An ingrown nail is primarily acting as Daniel has trained his nurse to push wisps sidiary of Bradley Pharmaceuticals Inc., hold the gutter tube in place. -

Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition
Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition: Redness, warmth, tenderness and exudate coming from the areas adjacent to the nail plate. Initial Diagnosis and Management: History and physical examination. In chronic infection appropriate radiographic (foot or toe series to rule out distal phalanx osteomyelitis) and laboratory evaluation (CBC and ESR). Ongoing Management and Objectives: Primary care should consist of Epsom salt soaks, or soapy water, and antibiotics for ten days. If Epsom salt soaks and antibiotics are ineffective, the primary care provider has the following options: Reevaluate and refer to podiatry. Perform temporary avulsion/I&D. Perform permanent avulsion followed by chemical cautery (89% Phenol or 10% NaOH application – 3 applications maintained for 30 second intervals, alcohol dilution between each application). Aftercare for all of the above is continued soaks, daily tip cleaning and bandage application. Indications for Specialty Care Referral: After the reevaluation at the end of the antibiotic period the primary care provider can refer the patient to Podiatry for avulsion/ surgical care if they do not feel comfortable performing the procedure themselves. The patient should be given a prescription for antibiotics renewal and orders to continue soaks until avulsion can be performed. Test(s) to Prepare for Consult: Test(s) Consultant May Need To Do: Criteria for Return to Primary Care: After completion of the surgical procedure, patients will be returned to the primary care provider for follow-up. Revision History: Created Revised Disclaimer: Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be considered inclusive of all accepted methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Ingrown Toenails
POST-OP NAIL CARE The day following the procedure, remove the bandage and begin soaking the toe for 10-15 minutes at least once daily. If the bandage does not come off easily, soak in warm water with one (1) tablespoon Epson Salts. As you soak, use a cotton tipped applicator (Q-tip) to clean the nail groove. Also, gently pull the skin edges back from the area where the nail was removed to be sure that any draining is released. After drying the toes, apply a light amount of triple antibiotic ointment (Neosporin) or other topical anesthetic, and light gauze or a bandage (Band-aid). Gauze is best to absorb INGROWN drainage. After a few days, the toe may be Brian Gardner, D.P.M. TOENAILS overly moist and need to dry. Use less triple antibiotic, continue soaking, Podiatrist and dress with light gauze or a Dr. Brian Gardner specializes in bandage (Band-aid). As drying foot and ankle surgery, wound care, occurs, tenderness will usually biomechanics, sports medicine, decrease. Continue soaks until the diabetic foot care, area is no longer draining (usually and general foot care. several weeks, if the nail root was treated with a chemical). facebook.com/UintahBasinHealthcare www.ubh.org 435.725.2025, Roosevelt 435.781.2030, Vernal 250 W 300 N Clinic #2 Suite 203 (Level 2), Roosevelt, Utah 379 N 500 W, Vernal, Utah Nails grow from a root beneath the skin TREATMENT IMPORTANT called the “matrix.” This growth center TREATMENT INFORMATION can vary in size and shape. It may Initially, your doctor may be able to produce a nail which is flat, curved, trim the ingrown toenail. -

Pedicure: Nail Enhancements
All Hair Services Include Shampoo All Services Based on Student Availability Long Hair is Extra & Senior Price Available Hair Cuts: Color: (Does Not Include Cut & Style) Hair Cut (Hood dryer) $6.50 Retouch/Tint/PM Shine $14.50 With Blowdry $13.50 Additional Application $8.00 With Blowdry & Flat Iron $21.50 Color (All over color) $20.00 Foils Each $4.00 Hair Styles: Hair Length to Collar $38.00 Shampoo/Set $6.75 Hair Length to Shoulder $48.00 Spiral Rod Set $20.00 Hair Length past Shoulder $58.00 Shampoo/ Blowdry $9.00 Frosting with Cap $17.50 With Thermal Iron $13.00 Men’s Comb Highlight with Cut $15.00 With Flat Iron $15.00 With Press & Curl $18.00 Perms & Relaxers: (Includes Cut & Style) Wrap Only $6.50 Regular or Normal Hair $20.95 Wrap with Roller Set $10.50 Resistant or Tinted Hair $26.00 Fingerwaves with Style $17.50 Spiral or Piggyback $36.00 Twists $3.00 Relaxer $35.00 Straight Back $20.00 Curled $15.00 Other Hair Services: Spiral $20.00 Shampoo Only $2.00 French Braids with Blowdry $15.00 Line-up $3.00 Under 10 Braids $20.00 Deep Condition $5.00 Over 10 Braids $25.00 Keratin Treatment $15.00 Braid Removal $15.00 Updo or French Roll $20.00 Manicure: Spa Manicure $9.50 Waxing: French Manicure $8.00 Brow $6.00 Manicure $6.42 Lip $5.00 Chin $5.00 Pedicure: Full Face $15.00 Spa Pedicure $20.00 Half Leg $15.00 French Pedicure $17.00 Full Leg $30.00 Pedicure $15.00 Underarm $15.00 Half Arm $10.00 Nail Enhancements: Full Arm $15.00 Shellac (French $2) $15.00 Mid Back & Up $15.00 Overlay (Natural Nail) $12.00 Full Back $25.00 Acrylic Full Set $16.50 Bikini $25.00 Gel Full Set $18.00 Fill-in Gel & Acrylic $12.00 Massages: Nail Repair( Per Nail) $2.00 Relaxation $15.00 Soak Off $3.00 Deep Tissue $19.95 Nail Art (Per Nail) $1.00 Other Nail Services: Nails & Waxing Services Taxable Polish Change $4.00 Nails Clipped $5.00 Paraffin Dip Wax $5.00 . -
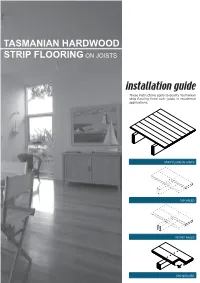
Tasmanian Hardwood Strip Flooring on Joists Guide for Installing
TASMANIAN HARDWOOD STRIP FLOORING ON JOISTS installation guide These instructions apply to quality Tasmanian strip flooring fixed over joists in residential applications. STRIP FLOOR ON JOISTS TOP NAILED SECRET NAILED END MATCHED TOOLS Simple tools are adequate in most applications. Necessary tools are: Tool Requirement Checklist Pencil, tape measure and square Hammer, punch and nail bag Stringline, spirit level and straight edge Hand saw and jig saw Safety glasses, dust mask and knee pads Spacers (about 100mm long and 2 mm thick) Rubber mallet, broom and vacuum cleaner Framing chisel For specialist applications, a drop saw, an air power staple gun, a power actuated fastener system and a cramping system may be useful. MATERIALS Use quality boards of the correct thickness. Grade descriptions for strip flooring are set out in the Australian Standard AS 2796 and are available at: www.tastimber.tas.gov.au. Boards at least 19 mm thick are needed to span 450 mm. Board width - Only secret nail boards up to 85 mm cover width. Secret nailed flooring is fixed through the tongue of specially profiled boards. Since they are only secured with one fastener per joist or batten, their width is limited to 85 mm cover. Board over 85 cover must be top nailed with two fasteners per joist. Use the correct nails for the job. The nail sizes required by Australian Standard 1684 are: Nail sizes for T & G flooring to joists* Nail sizes for T & G flooring to plywood substrate* Nailing Softwood Hardware & Strip flooring Rec. nailing (min.15mm substrate) joists cypress joists thicknes (mm) Hand 65 x 2.8 mm 50 x 2.8 mm 38 x 16 guage chisel point staples or driven bullet head bullet head 19 or 20 38 x 2.2 mm nails at 300mm spacing 32 x 16 guage chisel point staples or Machine 12,19 or 20 driven 65 x 2.5 mm 50 x 2.5 mm 30 x 2.2 mm nails at 200mm spacing *Alternative fasteners can be used for substrates types not listed subject to manufacturers’ recommendation. -

Regional Handwashing Policy
SOUTHERN CALIFORNIA GRADUATE MEDICAL EDUCATION POLICY AND PROCEDURE POLICY INFECTION PREVENTION AND CONTROL POLICIES EFFECTIVE DATE: SECTION: AND PROCEDURES 7/1/2014 TITLE: Hand Health & Hygiene Page: 1 of 8 BACKGROUND Studies have shown that handwashing causes a reduction in the carriage of potential pathogens on the hands. Microorganisms proliferate on the hands within the moist environment of gloves. Handwashing results in the reduction of patient morbidity and mortality from health care associated infections. The Centers for Disease Control and Prevention states that handwashing is the single most important procedure for preventing health-care associated infections. Artificial nails are more likely than natural nails to harbor pathogens that can lead to health care associated infections. There are four types of hand washing (see body of policy for detailed instructions): TYPE PURPOSE METHOD Routine Handwashing To remove soil and transient Wash hands with soap and microorganisms. water for at least 15 seconds. Hand antisepsis To remove soil and remove or Wash hands with antimicrobial destroy transient soap and water for at least 15 microorganisms. seconds. Hand rub/degerming To destroy transient and Rub alcohol-based hand resident microorganisms on degermer into hands vigorously UNSOILED hands. until dry. Surgical hand scrub To remove or destroy transient Wash hands and forearms with microorganisms and reduce antimicrobial soap and water resident flora. with brush to achieve friction. Or alcohol-based preparation rubbed vigorously -

White Nail As a Static Physical Finding: Revitalization of Physical Examination
Case Report White Nail as a Static Physical Finding: Revitalization of Physical Examination Ryuichi Ohta 1,* and Chiaki Sano 2 1 Community Care, Unnan City Hospital, 699-1221 96-1 Iida, Daito-cho, Unnan 699-1221, Shimane Prefecture, Japan 2 Department of Community Medicine Management, Faculty of Medicine, Shimane University, 89-1 Enya cho, Izumo 693-8501, Shimane Prefecture, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-9050605330 Abstract: Physical examinations are critical for diagnosis and should be differentiated into static and dynamic categories. One of the static findings is white nail, such as Terry’s and Lindsay’s nails. Here, we report the cases of two older patients with acute diseases who had nail changes that aided evaluation of their clinical course. Two elderly women who presented with acute conditions were initially thought to have normal serum albumin levels. They were found to have white nail with differences in nail involvement of the first finger, which subsequently revealed their hypoalbuminemia. The clinical courses were different following the distribution of nail whitening. Our findings show that examination of a white nail could indicate the previous clinical status more clearly than laboratory data. It can be useful for evaluating preclinical conditions in patients with acute diseases. Further evaluation is needed to establish the relationship between clinical outcomes and the presence of white nail in acute conditions among older patients. Citation: Ohta, R.; Sano, C. White Keywords: Lindsay’s nail; nail findings; nutritional assessment; physical examination; Terry’s nail; Nail as a Static Physical Finding: white nail Revitalization of Physical Examination. -

Customizable Wallet Cards
reason, we’ll refund your cost. your refund we’ll reason, cost. your refund we’ll reason, cost. your refund we’ll reason, cost. your refund we’ll reason, If you aren’t satisfied, for any any for satisfied, aren’t you If any for satisfied, aren’t you If any for satisfied, aren’t you If any for satisfied, aren’t you If waiting. No waiting. No waiting. No waiting. No apps to download. download. to apps No download. to apps No download. to apps No download. to apps No video required. required. video No required. deo vi No required. deo vi No required. deo vi No ne. li on t bu ne. li on t bu ne. li on t bu ne. li on t bu isit – – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik Fold line Fold Your 24/7 Your 24/7 Your 24/7 Your 24/7 online clinic online clinic online clinic online clinic A visit is just $45.* Insurance is accepted and Insurance is accepted and Insurance is accepted and Insurance is accepted and Insurance is accepted. applies to your deductible. appInsurancelies to your is accepted.deductible. appInsurancelies to your is deductible.accepted. appInsurancelies to your is deductible.accepted. *No*No cost cost if we can’tcan't treat trea you.t you. *No*No cost cost ifif we can’tcan't treat trea tyou. you. *No*No costcost if wewe can’tcan't treat treat you.