Report for the Hemodialysis Vascular Access: Standardized Fistula Rate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Known Infectious Causes of Vasculitis in Man
PATHOGENESIS Known infectious causes of vasculitis in man STANLEY J. NAIDES, MD n array of pathogens is known to cause vasculi- and our ability to intervene in disease processes, have ren- tis in man.1,2 For several of these agents, vas- dered some causes of vasculitis far less common. culitis is the major manifestation of disease. The Amajority, however, typically present as infec- ■ VIRAL CAUSES OF VASCULITIS tious processes in which vasculitis is an occasional mani- Our knowledge of viral pathogenesis has exploded in the festation of disease. For many, vasculitis may be a compo- last quarter of the twentieth century, accelerated in large nent of disease pathogenesis but is not a prominent feature part by epidemics of “emerging” viral diseases. Hepatitis C of the clinical presentation. The various agents—viruses, virus, discovered in 1989, has worldwide prevalence.3 The bacteria, and fungi—share a common target, blood vessels. 10- to 20-year latent period before hepatic or rheumatic The involvement of vessels may be direct, with vascular manifestations of disease explains the increasing number structures serving as targets. Many infectious pathogens of cases of hepatitis C virus–mediated vasculitis currently have tissue tropism that includes endothelium. Other being seen in the United States following the epidemic of agents may bind to the vessel wall because the vascular en- new infections in the 1980s.4 Prior to the discovery and dothelium expresses specific receptors for the pathogen or characterization of hepatitis C virus in the late 1980s, the another moiety with which the pathogen travels. Even triad of arthritis, palpable purpura, and type II cryoglobu- when the agent does not enter the endothelial cell, the im- linemia was given the sobriquet “essential mixed cryo- mune response to the agent may be focused at the vessel globulinemia” and considered an idiopathic vasculitis. -

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Healthcare Providers* Report Immediately by Phone!
Effective July 2008 COMMUNICABLE AND OTHER INFECTIOUS DISEASES REPORTABLE IN MASSACHUSETTS BY HEALTHCARE PROVIDERS* *The list of reportable diseases is not limited to those designated below and includes only those which are primarily reportable by clinical providers. A full list of reportable diseases in Massachusetts is detailed in 105 CMR 300.100. REPORT IMMEDIATELY BY PHONE! This includes both suspect and confirmed cases. All cases should be reported to your local board of health; if unavailable, call the Massachusetts Department of Public Health: Telephone: (617) 983-6800 Confidential Fax: (617) 983-6813 • REPORT PROMPTLY (WITHIN 1-2 BUSINESS DAYS). This includes both suspect and confirmed cases. All cases should be reported to your local board of health; if unavailable, call the Massachusetts Department of Public Health: Telephone: (617) 983-6800 Confidential Fax: (617) 983-6813 • Anaplasmosis • Leptospirosis Anthrax • Lyme disease Any case of an unusual illness thought to have Measles public health implications • Melioidosis Any cluster/outbreak of illness, including but not Meningitis, bacterial, community acquired limited to foodborne illness • Meningitis, viral (aseptic), and other infectious Botulism (non-bacterial) Brucellosis Meningococcal disease, invasive • Chagas disease (Neisseria meningitidis) • Creutzfeldt-Jakob disease (CJD) and variant CJD Monkeypox or other orthopox virus Diphtheria • Mumps • Ehrlichiosis • Pertussis • Encephalitis, any cause Plague • Food poisoning and toxicity (includes poisoning -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Identification of Microorganisms Using Nucleic Acid Probes
Identification of Microorganisms Using Page 1 of 45 Nucleic Acid Probes Medical Policy An Independent Licensee of the Blue Cross and Blue Shield Association Title: Identification of Microorganisms Using Nucleic Acid Probes See Also: Influenza Virus Diagnostic Testing and Treatment in the Outpatient Setting Professional Institutional Original Effective Date: July 8, 2008 Original Effective Date: July 16, 2009 Revision Date(s): June 16, 2009; Revision Date(s): March 1, 2012; March 1, 2012; June 5, 2012; June 5, 2012; November 19, 2012; November 19, 2012; January 15, 2013; January 15, 2013; November 12, 2013 November 12, 2013 Current Effective Date: November 12, 2013 Current Effective Date: November 12, 2013 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. Treating health care providers are independent contractors and are neither employees nor agents of Blue Cross and Blue Shield of Kansas and are solely responsible for diagnosis, treatment and medical advice. If your patient is covered under a different Blue Cross and Blue Shield plan, please refer to the Medical Policies of that plan. -

Rhinoscleroma in an Immigrant from Egypt: a Case Report
387 BRIEF COMMUNICATION Rhinoscleroma in an Immigrant From Egypt: A Case Report Edgardo Bonacina, MD,∗ Leonardo Chianura, MD, DTM&H,† Maurizio Sberna, MD,‡ Giuseppe Ortisi, MD,§ Giovanna Gelosa, MD,|| Alberto Citterio, MD,‡ Giovanni Gesu, MD,§ and Massimo Puoti, MD† Downloaded from https://academic.oup.com/jtm/article/19/6/387/1795562 by guest on 23 September 2021 Departments of ∗Pathological Anatomy; †Infectious Diseases; ‡Neuroradiology; §Microbiology, and; ||Otorinolaringoiatry, Niguarda Ca` Granda Hospital, Milano, Italy DOI: 10.1111/j.1708-8305.2012.00659.x Rhinoscleroma is a chronic indolent granulomatous infection of the nose and the upper respiratory tract caused by Klebsiella rhinoscleromatis; this condition is endemic to many regions of the world including North Africa. We present a case of rhinoscleroma in a 51-year-old Egyptian immigrant with 1-month history of epistaxis. We would postulate that with increased travel from areas where rhinoscleroma is endemic to other non-endemic areas, diagnosis of this condition will become more common. hough rarely observed, rhinoscleroma has to be nasal fossae and ethmoid sinuses with complete bony T taken into consideration in travelers returning destruction of bilateral nasal turbinates (Figure 1). with ear, nose, and throat presentations, particularly Endoscopic biopsy was performed under local anesthe- after traveling to developing countries or regions where sia. Histopathologic examination revealed numerous this condition is endemic.1,2 foamy macrophages (Mikulicz cells) containing bacteria (Figure 2); no fungal hyphae were found.3 Staphylococcus Case Report aureus and Klebsiella rhinoscleromatis were isolated by culture of the tissue biopsy. A diagnosis of rhinoscle- A 51-year-old Egyptian male immigrant presented on roma was made. -

Syphilis As Seen by a Hospital Physician
284 Prof. Monro?Syphilis as seen by a Hospital Physician. SYPHILIS AS SEEN BY A HOSPITAL PHYSICIAN* By T. K. MONRO, M.A., M.D., Professor of Medicine, University of Glasgow. \ " / Mr. President and Gentlemen,?I thank you heartily for the honour you have done me in inviting me to be Honorary President of this Faculty for the session which is now opening. I was duly informed by Dr. Wardlaw that my principal duty as incumbent of this honourable office was to deliver an address to the Faculty, and as his invitation reached me while I was on holiday, with other objects in view, I had time to contemplate the responsibility I had undertaken, and to consider how I was to face it. In getting over the usual initial difficulty as to the choice of a subject, some assistance was afforded me by the President's instruction that the address ought to be one for the general practitioner. Quite a number of subjects would be appropriate from this point of view. I should have been glad to say some- thing on oral sepsis, a condition often spoken of, and no doubt often wrongly blamed, but also apt to be overlooked. Dentists do not always realise how completely one may be misled by the absence of subjective and objective evidence; so that even an experienced man may pass as innocuous a tooth which subse- quent extraction shows to have disease at its root. Medical men sometimes make a mistake in the opposite direction, by insisting, without sufficient justification, on the removal of teeth, e.g., in epileptiform neuralgia. -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -
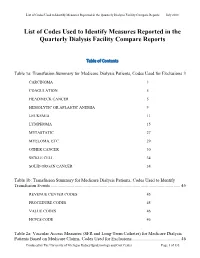
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -

Medical Management of Biological Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES FORT DETRICK FREDERICK, MARYLAND Emergency Response Numbers National Response Center: 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Helpline: 1-410-436-4484 or (Edgewood Ops Center – for military use) DSN 584-4484 USAMRIID’s Emergency Response Line: 1-888-872-7443 CDC'S Emergency Response Line: 1-770-488-7100 Handbook Download Site An Adobe Acrobat Reader (pdf file) version of this handbook can be downloaded from the internet at the following url: http://www.usamriid.army.mil USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 Lead Editor Lt Col Jon B. Woods, MC, USAF Contributing Editors CAPT Robert G. Darling, MC, USN LTC Zygmunt F. Dembek, MS, USAR Lt Col Bridget K. Carr, MSC, USAF COL Ted J. Cieslak, MC, USA LCDR James V. Lawler, MC, USN MAJ Anthony C. Littrell, MC, USA LTC Mark G. Kortepeter, MC, USA LTC Nelson W. Rebert, MS, USA LTC Scott A. Stanek, MC, USA COL James W. Martin, MC, USA Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 PREFACE TO THE SIXTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. -

Client Services Manual Public Health Laboratory
CLIENT SERVICES MANUAL PUBLIC HEALTH LABORATORY COUNTY OF SANTA CLARA 2220 MOORPARK AVE, 2ND FLOOR SAN JOSE, CA 95128 (P) 408.885.4272 | (F) 408.885.4275 http://www.sccgov.org/sites /sccphd/en-us/HealthProviders/Lab Patricia Dadone, Public Health Laboratory Director Sara H. Cody, MD, Health Officer and Public Health Director Table of Contents 1 GENERAL INFORMATION ............................................................................................... 1.1 ROLE .............................................................................................................................................................. 1.1 MISSION STATEMENT ..................................................................................................................................... 1.1 ABBREVIATIONS.............................................................................................................................................. 1.2 LABORATORY CERTIFICATIONS ........................................................................................................................ 1.4 CLIENT SERVICES ............................................................................................................................................ 1.5 Hours of Operation: .............................................................................................................................. 1.5 Supplies .................................................................................................................................................. -

Rickettsialpox-A Newly Recognized Rickettsial Disease V
Public Health Reports Vol. 62 * MAY 30, 1947 * No. 22 Printed With the Approval of the Bureau of the Budget as Required by Rule 42 of the Joint-Committee on Printing RICKETTSIALPOX-A NEWLY RECOGNIZED RICKETTSIAL DISEASE V. RECOVERY OF RICKETTSIA AKARI FROM A HOUSE MOUSE (MUS MUSCULUS)1 By ROBERT J. HUEBNER, Senior Assistant Surgeon, WILLIAm L. JELLISON, Parasitologist, CHARLES ARMSTRONG, Medical Director, United States Public Health Service Ricketttia akari, the causative agent of rickettsialpox, was isolated from the blood of persons ill with this disease (1) and from rodent mites Allodermanyssus sanguineus Hirst inhabiting the domicile of ill per- sons (2). This paper describes the isolation of R. akari from a house mouse (Mus musculus) trapped on the same premises-a housing development in the citr of New York where more than 100 cases of rickettsialpox have occurred (3), (4), (5), (6). Approximately 60 house mice were trapped in the basements of this housing development where rodent harborage existed in store rooms and in incinerator ashpits. Engorged mites were occasionally found attached to the mice, the usual site of attachment being the rump. Mites were frequently found inside the box traps after the captured mice were removed. Early attempts to isolate the etiological agent of rickettisalpox from these mice were complicated by the presence of choriomeningitis among them. Twelve successive suspensions of mouse tissue, repre- senting 16 house mice, inoculated intracerebrally into laboratory mice (Swiss strain) and intraperitoneally into guinea pigs resulted in the production of a highly lethal disease in both species which was identified immunologically as choriomeningitis.