Skull – Communication
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Middle Cranial Fossa Sphenoidal Region Dural Arteriovenous Fistulas: Anatomic and Treatment Considerations
ORIGINAL RESEARCH INTERVENTIONAL Middle Cranial Fossa Sphenoidal Region Dural Arteriovenous Fistulas: Anatomic and Treatment Considerations Z.-S. Shi, J. Ziegler, L. Feng, N.R. Gonzalez, S. Tateshima, R. Jahan, N.A. Martin, F. Vin˜uela, and G.R. Duckwiler ABSTRACT BACKGROUND AND PURPOSE: DAVFs rarely involve the sphenoid wings and middle cranial fossa. We characterize the angiographic findings, treatment, and outcome of DAVFs within the sphenoid wings. MATERIALS AND METHODS: We reviewed the clinical and radiologic data of 11 patients with DAVFs within the sphenoid wing that were treated with an endovascular or with a combined endovascular and surgical approach. RESULTS: Nine patients presented with ocular symptoms and 1 patient had a temporal parenchymal hematoma. Angiograms showed that 5 DAVFs were located on the lesser wing of sphenoid bone, whereas the other 6 were on the greater wing of the sphenoid bone. Multiple branches of the ICA and ECA supplied the lesions in 7 patients. Four patients had cortical venous reflux and 7 patients had varices. Eight patients were treated with transarterial embolization using liquid embolic agents, while 3 patients were treated with transvenous embo- lization with coils or in combination with Onyx. Surgical disconnection of the cortical veins was performed in 2 patients with incompletely occluded DAVFs. Anatomic cure was achieved in all patients. Eight patients had angiographic and clinical follow-up and none had recurrence of their lesions. CONCLUSIONS: DAVFs may occur within the dura of the sphenoid wings and may often have a presentation similar to cavernous sinus DAVFs, but because of potential associations with the cerebral venous system, may pose a risk for intracranial hemorrhage. -

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -
Imaging of Nontraumatic Temporal Bone Emergencies Nitesh Shekhrajka, MD and Gul Moonis, MD
Imaging of Nontraumatic Temporal Bone Emergencies Nitesh Shekhrajka, MD and Gul Moonis, MD This section aims to cover the non-traumatic pathologies affecting the temporal bone including external auditory canal, middle ear and inner ear which usually need emergent clinical attention. Many of the conditions in this section are secondary to infections in differ- ent clinical settings with resultant complications which may leave temporary or permanent sequelae if not suspected, timely diagnosed or treated. Semin Ultrasound CT MRI 40:116-124 © 2018 Elsevier Inc. All rights reserved. External Auditory Canal There is abnormal soft tissue thickening and enhancement along the margins of the EAC, auricle, and periauricular soft Malignant Otitis Externa tissue. There is effacement of the fat planes around the stylo- his is a more aggressive form of acute otitis externa mastoid foramen and infratemporal fossa5. The involvement T which affects the elderly, diabetic, and immunocompro- of the stylomastoid foramen may result in facial nerve mised patients.1 The term “Malignant” is a misnomer used to involvement. Opacification of middle ear cavity and mastoid describe the aggressive clinical nature and high mortality in air cells are frequently seen (Fig. 1). this condition. It is also referred to as necrotizing otitis If the disease extends inferiorly to involve the subtemporal externa (NOE). In most cases, the causative pathogen is Pseu- soft tissues, parotid, masticator, and parapharyngeal spaces, domonas aeruginosa2 which is not normally found in the imaging will demonstrate abnormal soft tissue enhancement, external acoustic meatus (EAC) but Aspergillus fumigatus is diffuse enlargement of the surrounding muscles, parotid also implicated in immunocompromised patients.3 enlargement, and effacement of the fat planes with or with- The infection begins as an area of granulation at the junc- out abscess. -

The Morphometric Study of Occurrence and Variations of Foramen Ovale S
Research Article The morphometric study of occurrence and variations of foramen ovale S. Ajrish George*, M. S. Thenmozhi ABSTRACT Background: Foramen vale is one of the important foramina present in the sphenoid bone. Anatomically it is located in the greater wing of the sphenoid bone. The foramen ovale is situated posterolateral to the foramen rotundum and anteromedial to the foramen spinosum. The foramen spinosum is present posterior to the foramen ovale. The carotid canal is present posterior and medial to the foramen spinosum and the foramen rotundum is present anterior to the foramen ovale. The structures which pass through the foramen ovale are the mandibular nerve, emissary vein, accessory middle meningeal artery, and lesser petrosal nerve. The sphenoid bone has a body, a pair of greater wing, pair of lesser wing, pair of lateral pterygoid plate, and a pair of medial pterygoid plate. Aim: The study involves the assessment of any additional features in foramen ovale in dry South Indian skulls. Materials and Methods: This study involves examination of dry adult skulls. First, the foramen ovale is located, and then it is carefully examined for presence of alterations and additional features, and is recorded following computing the data and analyzing it. Results: The maximum length of foramen ovale on the right and left was 10.1 mm, 4.3 mm, respectively. The minimum length of the foramen in right and left was 9.1 mm, 3.2 mm, respectively. The maximum width of foramen ovale on the right and left was 4.8 mm and 2.3 mm, respectively. The minimum width of the foramen in the right and the left side was 5.7 mm and 2.9 mm, respectively. -
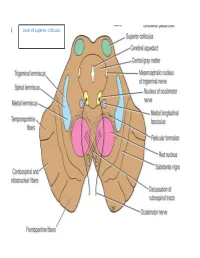
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Gluteal Region-II
Gluteal Region-II Dr Garima Sehgal Associate Professor King George’s Medical University UP, Lucknow Structures in the Gluteal region • Bones & joints • Ligaments Thickest muscle • Muscles • Vessels • Nerves Thickest nerve • Bursae Learning Objectives By the end of this teaching session Gluteal region –II all the MBBS 1st year students must be able to: • Enumerate the nerves of gluteal region • Write a short note on nerves of gluteal region • Describe the location & relations of sciatic nerve in gluteal region • Enumerate the arteries of gluteal region • Write a short note on arteries of gluteal region • Enumerate the arteries taking part in trochanteric and cruciate anastomosis • Write a short note on trochanteric and cruciate anastomosis • Enumerate the structures passing through greater sciatic foramen • Enumerate the structures passing through lesser sciatic foramen • Enumerate the bursae in relation to gluteus maximus • Enumerate the structures deep to gluteus maximus • Discuss applied anatomy Nerves of Gluteal region (all nerves in gluteal region are branches of sacral plexus) Superior gluteal nerve (L4,L5, S1) Inferior gluteal nerve (L5, S1, S2) FROM DORSAL DIVISIONS Perforating cutaneous nerve (S2,S3) Nerve to quadratus femoris (L4,L5, S1) Nerve to obturator internus (L5, S1, S2) FROM VENTRAL DIVISIONS Pudendal nerve (S2,S3,S4) Sciatic nerve (L4,L5,S1,S2,S3) Posterior cutaneous nerve of thigh FROM BOTH DORSAL &VENTRAL (S1,S2) & (S2,S3) DIVISIONS 1. Superior Gluteal nerve (L4,L5,S1- dorsal division) 1 • Enters through the greater 3 sciatic foramen • Above piriformis 2 • Runs forwards between gluteus medius & gluteus minimus • SUPPLIES: 1. Gluteus medius 2. Gluteus minimus 3. Tensor fasciae latae 2. -

Craniotomy for Anterior Cranial Fossa Meningiomas: Historical Overview
Neurosurg Focus 36 (4):E14, 2014 ©AANS, 2014 Craniotomy for anterior cranial fossa meningiomas: historical overview SAUL F. MORALES-VALERO, M.D., JAMIE J. VAN GOMPEL, M.D., IOANNIS LOUMIOTIS, M.D., AND GIUSEPPE LANZINO, M.D. Department of Neurologic Surgery, Mayo Clinic, Mayo Medical School, Rochester, Minnesota The surgical treatment of meningiomas located at the base of the anterior cranial fossa is often challenging, and the evolution of the surgical strategy to resect these tumors parallels the development of craniotomy, and neurosur- gery in general, over the past century. Early successful operations to treat these tumors were pioneered by prominent figures such as Sir William Macewen and Francesco Durante. Following these early reports, Harvey Cushing made significant contributions, allowing a better understanding and treatment of meningiomas in general, but particularly those involving the anterior cranial base. Initially, large-sized unilateral or bilateral craniotomies were necessary to approach these deep-seated lesions. Technical advances such as the introduction of electrosurgery, the operating microscope, and refined microsurgical instruments allowed neurosurgeons to perform less invasive surgical proce- dures with better results. Today, a wide variety of surgical strategies, including endoscopic surgery and radiosurgery, are used to treat these tumors. In this review, the authors trace the evolution of craniotomy for anterior cranial fossa meningiomas. (http://thejns.org/doi/abs/10.3171/2014.1.FOCUS13569) KEY WORDS • intracranial meningiomas • craniotomy • history • anterior cranial fossa ENINGIOMAS of the anterior cranial fossa represent has a few distinct clinical features. However, in practice, 12%–20% of all intracranial meningiomas.5,30 this group of tumors often represents a continuum. -

Ardipithecus Ramidus and the Evolution of the Human Cranial Base
Ardipithecus ramidus and the evolution of the human cranial base William H. Kimbela,1, Gen Suwab, Berhane Asfawc, Yoel Raka,d, and Tim D. Whitee,1 aInstitute of Human Origins and School of Human Evolution and Social Change, Arizona State University, Tempe, AZ 85287; bThe University Museum, University of Tokyo, Bunkyo-ku, Tokyo 113-0033, Japan; cRift Valley Research Service, Addis Ababa, Ethiopia; dDepartment of Anatomy and Anthropology, Sackler School of Medicine, Tel Aviv University, 69978 Ramat Aviv, Israel; and eDepartment of Integrative Biology, Human Evolution Research Center, University of California, Berkeley, CA 94720 Contributed by Tim D. White, December 5, 2013 (sent for review October 14, 2013) The early Pliocene African hominoid Ardipithecus ramidus was di- We report here results of a metrical and morphological study agnosed as a having a unique phylogenetic relationship with the of the Ar. ramidus basicranium as another test of its hypothesized Australopithecus + Homo clade based on nonhoning canine teeth, phylogenetic affinity with Australopithecus and Homo. We ana- a foreshortened cranial base, and postcranial characters related to lyzed the length and breadth of the external cranial base and the facultative bipedality. However, pedal and pelvic traits indicating structural relationship between the petrous and tympanic elements substantial arboreality have raised arguments that this taxon may of the temporal bone in Ar. ramidus, Australopithecus (including instead be an example of parallel evolution of human-like traits Paranthropus of some authors), and mixed-sex samples of extant among apes around the time of the chimpanzee–human split. Here African hominoid (Gorilla gorilla, Pan troglodytes, Pan paniscus) we investigated the basicranial morphology of Ar. -

Entrapment Neuropathy of the Central Nervous System. Part II. Cranial
Entrapment neuropathy of the Cranial nerves central nervous system. Part II. Cranial nerves 1-IV, VI-VIII, XII HAROLD I. MAGOUN, D.O., F.A.A.O. Denver, Colorado This article, the second in a series, significance because of possible embarrassment considers specific examples of by adjacent structures in that area. The same entrapment neuropathy. It discusses entrapment can occur en route to their desti- nation. sources of malfunction of the olfactory nerves ranging from the The first cranial nerve relatively rare anosmia to the common The olfactory nerves (I) arise from the nasal chronic nasal drip. The frequency of mucosa and send about twenty central proces- ocular defects in the population today ses through the cribriform plate of the ethmoid bone to the inferior surface of the olfactory attests to the vulnerability of the optic bulb. They are concerned only with the sense nerves. Certain areas traversed by of smell. Many normal people have difficulty in each oculomotor nerve are pointed out identifying definite odors although they can as potential trouble spots. It is seen perceive them. This is not of real concern. The how the trochlear nerves are subject total loss of smell, or anosmia, is the significant to tension, pressure, or stress from abnormality. It may be due to a considerable variety of causes from arteriosclerosis to tu- trauma to various bony components morous growths but there is another cause of the skull. Finally, structural which is not usually considered. influences on the abducens, facial, The cribriform plate fits within the ethmoid acoustic, and hypoglossal nerves notch between the orbital plates of the frontal are explored. -

Lab #23 Anal Triangle
THE BONY PELVIS AND ANAL TRIANGLE (Grant's Dissector [16th Ed.] pp. 141-145) TODAY’S GOALS: 1. Identify relevant bony features/landmarks on skeletal materials or pelvic models. 2. Identify the sacrotuberous and sacrospinous ligaments. 3. Describe the organization and divisions of the perineum into two triangles: anal triangle and urogenital triangle 4. Dissect the ischiorectal (ischioanal) fossa and define its boundaries. 5. Identify the inferior rectal nerve and artery, the pudendal (Alcock’s) canal and the external anal sphincter. DISSECTION NOTES: The perineum is the diamond-shaped area between the upper thighs and below the inferior pelvic aperture and pelvic diaphragm. It is divided anatomically into 2 triangles: the anal triangle and the urogenital (UG) triangle (Dissector p. 142, Fig. 5.2). The anal triangle is bounded by the tip of the coccyx, sacrotuberous ligaments, and a line connecting the right and left ischial tuberosities. It contains the anal canal, which pierced the levator ani muscle portion of the pelvic diaphragm. The urogenital triangle is bounded by the ischiopubic rami to the inferior surface of the pubic symphysis and a line connecting the right and left ischial tuberosities. This triangular space contains the urogenital (UG) diaphragm that transmits the urethra (in male) and urethra and vagina (in female). A. Anal Triangle Turn the cadaver into the prone position. Make skin incisions as on page 144, Fig. 5.4 of the Dissector. Reflect skin and superficial fascia of the gluteal region in one flap to expose the large gluteus maximus muscle. This muscle has proximal attachments to the posteromedial surface of the ilium, posterior surfaces of the sacrum and coccyx, and the sacrotuberous ligament. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

A New Radiological Classification for the Risk Assessment of Anterior Skull
www.nature.com/scientificreports OPEN A new radiological classifcation for the risk assessment of anterior skull base injury in endoscopic sinus surgery Baharudin Abdullah 1*, Shiun Chuen Chew1, Mohd Ezane Aziz2, Norasnieda Md Shukri1, Salina Husain3, Sng Weirong Joshua4, De Yun Wang4 & Kornkiat Snidvongs5 Keros and Gera classifcations are widely used to assess the risk of skull base injury during endoscopic sinus surgery. Although, both classifcations are useful preoperatively to stratify risk of patients going for surgery, it is not practical to measure the respective lengths during surgery. In this study, we aimed to propose a new radiological classifcation (Thailand-Malaysia-Singapore (TMS)) to assess the anatomical risk of anterior skull base injury using the orbital foor (OF) as a reference. A total of 150 computed tomography images of paranasal sinuses (300 sides) were reviewed. The TMS classifcation was categorized into 3 types by measuring OF to cribriform plate and OF to ethmoid roof. Most patients were classifed as TMS type 1, Keros type 2 and Gera class II, followed by patients classifed as TMS type 3, Keros type 1 and Gera class 1. TMS has signifcant correlation with Keros classifcation (p < 0.05). There was no signifcant correlation between Keros and Gera classifcations (p = 0.33) and between TMS and Gera classifcations (p = 0.80). The TMS classifcation has potential to be used for risk assessment of skull base injury among patients undergoing ESS. It serves as an additional assessment besides the Keros and Gera classifcations. Endoscopic sinus surgery (ESS) has an overall complication rate of 0.5% with the specifc complications of cere- brospinal fuid leak, orbital injury, haemorrhage requiring surgery, blood transfusion and toxic shock syndrome at 0.09%, 0.09%, 0.10%, 0.18%, and 0.02%, respectively1.