Programs and Services for Suicide Prevention
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fresno County Community-Based Suicide Prevention Strategic Plan
Fresno County Community-Based Suicide Prevention Strategic Plan Written by DeQuincy A. Lezine, PhD and Noah J. Whitaker, MBA For those who struggle, those who have been lost, those left behind, may you find hope… Fresno Cares 2018 Introduction 4 Background and Rationale 5 How Suicide Impacts Fresno County 5 The Fresno County Suicide Prevention Collaborative 7 History 8 Capacity-Building 9 Suicide Prevention in Schools (AB 2246) 10 Workgroups 10 Data 11 Communication 11 Learning & Education 12 Health Care 13 Schools 14 Justice & First Responders 15 Understanding Suicide 16 Overview: the Suicidal crisis within life context 17 The Suicidal Crisis: Timeline of suicidal crisis and prevention 22 Levels of Influence: The Social-Ecological Model 23 Identifying and Characterizing Risk 24 Understanding How Risk Escalates Into Suicidal Thinking 26 Warning Signs: Recognizing when someone may be suicidal 27 Understanding How Suicidal Thinking Turns into Behavior 28 Understanding How a Suicide Attempt Becomes a Suicide 28 Understanding How Suicide Affects Personal Connections 29 Stopping the Crisis Path 30 Comprehensive Suicide Prevention in Fresno County 31 Health and Wellness Promotion 34 Prevention (Universal strategies) 34 Early Intervention (Selective strategies) 35 Clinical Intervention (Selective strategies) 35 Crisis Intervention and Postvention (Indicated strategies) 36 Where We are Now: Needs and Assets in Fresno County 37 Suicidal Thoughts and Feelings 37 Suicide Attempts 40 1 Suicide 41 Understanding -

Community Conversations to Inform Youth Suicide Prevention
2018 Community Conversations to Inform Youth Suicide Prevention A STUDY OF YOUTH SUICIDE IN FOUR COLORADO COUNTIES Presented to Attorney General Cynthia H. Coffman Colorado Office of the Attorney General By Health Management Associates 2 TABLE OF CONTENTS Acknowledgements............................................................................................................................................................. 3 Executive Summary..............................................................................................................................................................4 Introduction..........................................................................................................................................................................11 Scope of the Problem........................................................................................................................................................11 Key Stakeholder Interviews...........................................................................................................................................13 Community Focus Groups.............................................................................................................................................. 17 School Policies & Procedures........................................................................................................................................27 Traditional Media & Suicide.......................................................................................................................................... -

Answer Key: Suicide Prevention
Personal Health Series Suicide Quiz Answer Key 1. List four factors that can increase a teen’s risk of suicide: Any four of the following: a psychological disorder, especially depression, bipolar disorder, and alcohol and/or drug use; feelings of hopelessness and worthlessness; previous suicide attempt; family history of depression or suicide; emotional, physical, or sexual abuse; lack of a support network, poor relationships with parents or peers, and feelings of social isolation; dealing with bisexuality or homosexuality in an unsupportive family or community or hostile school environment; perfectionism. 2. True or false: If a person talks about suicide, it means he or she is just looking for attention and won’t go through with it. 3. True or false: The danger of suicide has passed when a person begins to cheer up. 4. List four warning signs that someone is thinking about suicide: Any four of the following: talking about suicide or death in general; hinting he/she might not be around anymore; talking about feeling hopeless or feeling guilty; pulling away from friends or family; writing songs, poems, or letters about death, separation, or loss; giving away treasured possessions; losing the desire to do favorite things or activities; having trouble concentrating or thinking clearly; changing eating or sleeping habits; engaging in risky or self-destructive behaviors; losing interest in school and/or extra-curricular activities. 5. True or false: Once a person is suicidal, he or she is suicidal forever. 6. True or false: Most teens who attempt suicide really intend to die. 7. True or false: If a friend tells you she’s considering suicide and swears you to secrecy, you have to keep your promise. -

Suicide Research: Selected Readings. Volume 2
SuicideResearchText-Vol2:SuicideResearchText-Vol2 8/6/10 11:00 AM Page i SUICIDE RESEARCH: SELECTED READINGS Volume 2 May 2009–October 2009 J. Sveticic, K. Andersen, D. De Leo Australian Institute for Suicide Research and Prevention WHO Collaborating Centre for Research and Training in Suicide Prevention National Centre of Excellence in Suicide Prevention SuicideResearchText-Vol2:SuicideResearchText-Vol2 8/6/10 11:00 AM Page ii First published in 2009 Australian Academic Press 32 Jeays Street Bowen Hills Qld 4006 Australia www.australianacademicpress.com.au Reprinted in 2010 Copyright for the Introduction and Comments sections is held by the Australian Institute for Suicide Research and Prevention, 2009. Copyright in all abstracts is retained by the current rights holder. Apart from any use as permitted under the Copyright Act, 1968, no part may be reproduced without prior permission from the Australian Institute for Suicide Research and Prevention. ISBN: 978-1-921513-53-4 SuicideResearchText-Vol2:SuicideResearchText-Vol2 8/6/10 11:00 AM Page iii Contents Foreword ................................................................................................vii Acknowledgments ..............................................................................viii Introduction Context ..................................................................................................1 Methodology ........................................................................................2 Key articles Alexopoulos et al, 2009. Reducing suicidal ideation -

Preventing Suicide: a Global Imperative
PreventingPreventing suicidesuicide A globalglobal imperativeimperative PreventingPreventing suicidesuicide A globalglobal imperativeimperative WHO Library Cataloguing-in-Publication Data Preventing suicide: a global imperative. 1.Suicide, Attempted. 2.Suicide - prevention and control. 3.Suicidal Ideation. 4.National Health Programs. I.World Health Organization. ISBN 978 92 4 156477 9 (NLM classification: HV 6545) © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are The mention of specific companies or of certain manufacturers’ available on the WHO website (www.who.int) or can be purchased products does not imply that they are endorsed or recommended by from WHO Press, World Health Organization, 20 Avenue Appia, the World Health Organization in preference to others of a similar 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 nature that are not mentioned. Errors and omissions excepted, the 4857; e-mail: [email protected]). names of proprietary products are distinguished by initial capital letters. Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be All reasonable precautions have been taken by the World Health addressed to WHO Press through the WHO website Organization to verify the information contained in this publication. (www.who.int/about/licensing/copyright_form/en/index.html). However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility The designations employed and the presentation of the material in for the interpretation and use of the material lies with the reader. In this publication do not imply the expression of any opinion no event shall the World Health Organization be liable for damages whatsoever on the part of the World Health Organization concerning arising from its use. -

Domestic Violence and Suicide
SUICIDE PREVENTION COALITION OF WARREN AND CLINTON COUNTIES Domestic Violence and Suicide Unlike the more usual domestic violence, murder-suicide includes both depression and suicidal thoughts. Murder-suicide is a shattering, violent event in which a person commits murder, and then shortly after commits suicide. What makes these acts particularly disturbing is that they take the lives of more than one person and often result in the death of family members. How are Domestic Violence and Murder-Suicide Murder-Suicide Facts: Related? More than 10 murder-suicides, almost all by gun, occur each week in the United States. 50 - 75% of the 1,200 to In an average six-month period, nearly 591 Americans die in 1,500 annual deaths 264 murder-suicides. resulting from murder- Almost all murder-suicides (92%) involve a firearm. suicide occur in spousal or 94% of offenders in murder-suicides are male. other intimate relation- 74% of all murder-suicides involve an intimate partner ships. (spouse, common-law spouse, ex-spouse, or boyfriend/ A home in which anyone girlfriend). Of these, roughly 96% are females killed by their has been hit or hurt is 4.4 intimate male partners. times more likely to be Murder-suicides almost always involve a firearm. the scene of a homicide RESOURCES Intervention provides Crisis Hotline (toll-free 24-hour): hope and assistance. 877-695-NEED or 877-695-6333 You can find help. Know the signs of Solutions Community Counseling & Recovery Centers someone at risk. Lebanon (975A Kingsview Dr.) 513-228-7800 Lebanon (204 Cook Rd.) 513-934-7119 Springboro (50 Greenwood Ln.) 937-746-1154 Together Seek help! We Can Make A There are several local Mason (201 Reading Rd.) 513-398-2551 Difference Wilmington (953 S. -

Surviving Suicide Loss
Surviving Suicide Loss ISSUE NO 1 | SPRING 2021 | VOLUME 1 IN THIS ISSUE Letter from the Chair ………….……….……….……………….……….………. 1 AAS Survivor of the Year ……….……….…………………..……….……..…. 1 Editor’s Note ....……………………….……….……………….……….…………... 2 Surviving Suicide Loss in the Age of Covid ……….……….…………...…. 2 What the Latest Research Tells Us ……………….…….……….……………. 3 Waiting for the Fog to Clear ……………….…………………..……….…..…… 4 AAS Survivor-Related Events ……………….…..……….…………………..…. 4 In the Early Morning Hours …………………………………………………..…... 6 IN SEARCH OF NEW BEGINNINGS Letter from the Chair I clearly remember attending my first AAS conference in 2005. Six months after losing my sister, I was scared, confused, thirsty for knowledge and ever so emotional. There I met so many people who are near and dear to me today. They welcomed me, remi- nisced with me and, most of all, inspired me. On my flight back, I had many thoughts and feelings. As I am Building Community sure many of you have experienced, writing was both helpful Seeing my article made me feel a part of this community in and healing. So I wrote down my musings from the conference and when back at home, I edited the piece and sent it to Ginny the best ways, surrounded by supportive and like-minded Sparrow. minded folks. As you may remember, Ginny was the extraordinary editor of the Thus, I am happy to have a part in reviving “Surviving Suicide” print newsletter Surviving Suicide, a publication sent to AAS Loss in digital form. I hope it will be a place where all of us can Division members from approximately 1998 through 2007. share our thoughts, our news, our hopes and fears, while hon- oring our loved ones and further building our community. -
National Guidelines: Responding to Grief, Trauma, and Distress After a Suicide
Responding to Grief, Trauma, and Distress After a Suicide: U.S. National Guidelines Survivors of Suicide Loss Task Force April 2015 Blank page Responding to Grief, Trauma, and Distress After a Suicide: U.S. National Guidelines Table of Contents Front Matter Acknowledgements ...................................................................................................................................... i Task Force Co-Leads, Members .................................................................................................................. ii Reviewers .................................................................................................................................................... ii Preface ....................................................................................................................................................... iii National Guidelines Executive Summary ..................................................................................................................................... 1 Introduction ................................................................................................................................................ 4 Terminology: “Postvention” and “Loss Survivor” ....................................................................................... 4 Development and Purpose of the Guidelines ............................................................................................. 6 Audience of the Guidelines ........................................................................................................................ -
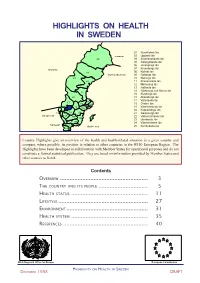
Sweden Part 1
HIGHLIGHTS ON HEALTH IN SWEDEN 01 Stockholms län 03 Uppsala län Finland 25 04 Södermanlands län 05 Östergötlands län 06 Jönköpings län 07 Kronobergs län Norway 08 Kalmar län 24 Gulf of Bothnia 09 Gotlands län 23 10 Blekinge län 22 11 Kristianstads län 12 Malmöhus län 13 Hallands län 14 Göteborgs och Bohus län 21 15 Älvsborgs län 20 16 Skaraborgs län 17 Värmlands län 17 03 18 Örebro län 19 01 18 19 Västmanlands län 04 20 Kopparbergs län 14 16 05 21 Gävleborgs län Skagerrak 15 06 22 Västernorrlands län 08 09 23 Jämtlands län 13 07 24 Västerbottens län Kattegat 11 10 Baltic sea 25 Norrbottens län 12 Country Highlights give an overview of the health and health-related situation in a given country and compare, where possible, its position in relation to other countries in the WHO European Region. The Highlights have been developed in collaboration with Member States for operational purposes and do not constitute a formal statistical publication. They are based on information provided by Member States and other sources as listed. Contents OVERVIEW ....................................................... 3 THE COUNTRY AND ITS PEOPLE ............................... 5 HEALTH STATUS ................................................ 11 LIFESTYLE ........................................................ 27 ENVIRONMENT ................................................... 31 HEALTH SYSTEM ................................................ 35 REFERENCES ..................................................... 40 WHO Regional Office for Europe European Commission -
Suicide Prevention, Intervention, and Postvention Protocols
Suicide Prevention, Intervention, and Postvention Protocols: A Toolkit for Maine Schools Protocol for Suicide Prevention, Intervention, and Postvention: A Toolkit for Maine Schools INTRODUCTION TO THE TOOLKIT Suicide Prevention, Intervention, and Postvention Toolkit for Maine Schools A School’s Legal Responsibility to Provide Suicide Prevention: LD 609: An Act to Increase Suicide Awareness and Prevention in Maine Schools, was signed into law by Governor Paul LePage on April 25, 2013, following unanimous passage in the legislature. The statute requires a 1-2 hour Suicide Prevention Awareness Education training be completed by all school personnel in each school administrative unit (SAU), island, charter, CTE Region and public school that is not in a school administrative unit. It also requires all school administrative units and each island, charter, approved private and public schools that are not in a school administrative unit to have at least two staff trained in a one-day course in suicide prevention and intervention training commonly referred to in Maine as “Gatekeeper Training.” A CTE Region must have at least one school personnel member who has successfully completed Gatekeeper training on site. The second school personnel member could be either on site or the CTE Region could have a legal agreement with one of the sending schools assigned to their region. In addition, the law recommends that schools develop and implement protocols for suicide prevention and intervention. As part of a comprehensive suicide prevention and intervention program, it is essential that schools have written protocols for responding to: A. Students presenting with warning signs of suicide B. A suicide attempt C. -

Understanding Risk & Protective Factors for Suicide
Understanding Risk and Protective Factors for Suicide: A Primer for Preventing Suicide Risk and protective factors play a critical role in suicide prevention. For clinicians, identifying risk and protective factors provides critical information to assess and manage suicide risk in individuals. For communities and prevention programs, identifying risk and protective factors provides direction about what to change or promote. Many lists of risk factors are available throughout the field of suicide prevention. This paper provides a brief overview of the importance of risk and protective factors as they relate to suicide and offers guidance about how communities can best use them to decrease suicide risk. Contents: What are risk and protective factors? Risk factors are not warning signs. What are major risk and protective factors for suicide? Why are risk and protective factors important? Using risk and protective factors in the strategic planning process Key points about risk and protective factors for suicide prevention Additional resources Further reading References What are risk and protective factors? Risk factors are characteristics that make it more likely that individuals will consider, attempt, or die by suicide. Protective factors are characteristics that make it less likely that individuals will consider, attempt, or die by suicide. Risk and protective factors are found at various levels: individual (e.g., genetic predispositions, mental disorders, personality traits), family (e.g., cohesion, dysfunction), and community (e.g., availability of mental health services). They may be fixed (those things that cannot be changed, such as a family history of suicide) or modifiable (those things that can be changed, such as depression). -

Physician Suicide: a Scoping Literature Review to Highlight Opportunities for Prevention
GLOBAL PSYCHIATRY — Vol 3 | Issue 2 | 2020 Tiffany I. Leung, MD, MPH, FACP, FAMIA1*, Rebecca Snyder, MSIS2, Sima S. Pendharkar, MD, MPH, FACP3‡, Chwen-Yuen Angie Chen, MD, FACP, FASAM4‡ Physician Suicide: A Scoping Literature Review to Highlight Opportunities for Prevention 1Faculty of Health, Medicine, and Life Sciences, Department of Internal Medicine, Maastricht University, Maastricht, The Netherlands 2Library Services, University of Texas Southwestern Medical Center, Dallas, TX, USA 3Division of Hospital Medicine, The Brooklyn Hospital Center, Icahn School of Medicine Mt. Sinai, Brooklyn, NY, USA 4Department of Primary Care and Population Health, Stanford University, Palo Alto, CA, USA *email: [email protected] ‡Indicates equal contributions as last authors to the production of this manuscript. DOI: 10.2478/gp-2020-0014 Received: 27 February 2020; Accepted: 12 May 2020 Abstract Objective: The aim of this scoping review is to map the current landscape of published research and perspectives on physician suicide. Findings could serve as a roadmap for further investigations and potentially inform efforts to prevent physician suicide. Methods: Ovid MEDLINE, PsycINFO, and Scopus were searched for English-language publications from August 21, 2017 through April 28, 2018. Inclusion criteria were a primary outcome or thesis focused on suicide (including suicide completion, attempts, and thoughts or ideation) among medical students, postgraduate trainees, or attending physicians. Opinion articles were included. Studies that were non-English or those that only mentioned physician burnout, mental health, or substance use disorders were excluded. Data extraction was performed by two authors. Results: The search yielded 1,596 articles, of which 347 articles passed to the full-text review round.