Complement in Vasculitis and Glomerulonephritis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glomerulonephritis Management in General Practice
Renal disease • THEME Glomerulonephritis Management in general practice Nicole M Isbel MBBS, FRACP, is Consultant Nephrologist, Princess Alexandra lomerular disease remains an important cause Hospital, Brisbane, BACKGROUND Glomerulonephritis (GN) is an G and Senior Lecturer in important cause of both acute and chronic kidney of renal impairment (and is the commonest cause Medicine, University disease, however the diagnosis can be difficult of end stage kidney disease [ESKD] in Australia).1 of Queensland. nikky_ due to the variability of presenting features. Early diagnosis is essential as intervention can make [email protected] a significant impact on improving patient outcomes. OBJECTIVE This article aims to develop However, presentation can be variable – from indolent a structured approach to the investigation of patients with markers of kidney disease, and and asymptomatic to explosive with rapid loss of kidney promote the recognition of patients who need function. Pathology may be localised to the kidney or further assessment. Consideration is given to the part of a systemic illness. Therefore diagnosis involves importance of general measures required in the a systematic approach using a combination of clinical care of patients with GN. features, directed laboratory and radiological testing, DISCUSSION Glomerulonephritis is not an and in many (but not all) cases, a kidney biopsy to everyday presentation, however recognition establish the histological diagnosis. Management of and appropriate management is important to glomerulonephritis (GN) involves specific therapies prevent loss of kidney function. Disease specific directed at the underlying, often immunological cause treatment of GN may require specialist care, of the disease and more general strategies aimed at however much of the management involves delaying progression of kidney impairment. -

Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis
Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis MATTHEW D. GRIFFIN,* JOHANNES BJORNSSON,t and STEPHEN B. ERICKSON* *Department of Internal Medicine, Division of Nephrology, and tDepartment of Pathology, Mayo Clinic and Mayo Foundation, Rochester, Minnesota. Abstract. A 72-year-old man developed acute renal failure after peated surgical debridement. Spontaneous recovery of renal coronary bypass surgery that had been complicated by sternal function occurred after eradication of infection and final sur- osteomyelitis caused by the Staphylococcus aureus bacterium. gical wound repair. The relationship between acute bacterial Bacteremia and sepsis were not present. Renal biopsy demon- infections and glomerulonephritis and, in particular, the causal strated a florid, diffuse, proliferative glomerulonephritis with role of staphylococcal antigens in the pathogenesis of such glomerular immune complex deposition. Management in- lesions is discussed. (J Am Soc Nephrol 8: 1633-1639, 1997) cluded hemodialysis, prolonged antibiotic therapy, and re- Coagulase-positive staphylococcus (Staphylococcus aureus) is mg/dl]) and in the immediate postoperative period. Over the the most common causative organism in acute osteomyelitis following days, the patient’s serum creatinine concentration (1). Along with coagulase-negative staphylococcal species, it increased progressively, and hemodialysis was instituted on has also been implicated in the pathogenesis of immune com- day 23 after CABG. There was no past or family history of plex (IC)-mediated diffuse proliferative glomerulonephritis renal disease and no known drug allergies. Prior medical (DPGN) in a variety of infections. These include bacterial history had included degenerative disc disease, stable abdom- endocarditis, ventriculoatrial shunt infections, pneumonia, and inal aortic aneurysm, stable benign prostatic hyperplasia, and visceral abscesses with or without septicemia (2-6). -

Glomerulonephritis
Adolesc Med 16 (2005) 67–85 Glomerulonephritis Keith K. Lau, MDa,b, Robert J. Wyatt, MD, MSa,b,* aDivision of Pediatric Nephrology, Department of Pediatrics, University of Tennessee Health Sciences Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA bChildren’s Foundation Research Center at the Le Bonheur Children’s Medical Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA Early diagnosis of glomerulonephritis (GN) in the adolescent is important in initiating appropriate treatment and controlling chronic glomerular injury that may eventually lead to end-stage renal disease (ESRD). The spectrum of GN in adolescents is more similar to that seen in young and middle-aged adults than to that observed in prepubertal children. In this article, the authors discuss the clinical features associated with GN and the diagnostic evaluation required to determine the specific type of GN. With the exception of hereditary nephritis (Alport’s disease), virtually all types of GN are immunologically mediated with glomerular deposition of immunoglobulins and complement proteins. The inflammatory events leading to GN may be triggered by a number of factors. Most commonly, immune complexes deposit in the glomeruli or are formed in situ with the antigen as a structural component of the glomerulus. The immune complexes then initiate the production of proinflammatory mediators, such as complement proteins and cytokines. Subsequently, the processes of sclerosis within the glomeruli and fibrosis in the tubulointerstitial cells lead to chronic or even irreversible renal injury [1]. Less commonly, these processes occur without involvement of immune complexes—so-called ‘‘pauci-immune GN.’’ * Corresponding author. -
Nephritis Fact Sheet
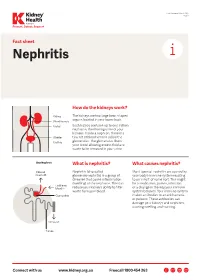
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine. -

Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy
PATHOPHYSIOLOGY of the RENAL BIOPSY www.jasn.org Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy Charles E. Alpers and Jolanta Kowalewska Department of Pathology, University of Washington, Seattle, Washington ABSTRACT extracellular accumulation of haphaz- Fibrillary glomerulonephritis is a now widely recognized diagnostic entity, occur- ardly arranged fibrils measuring ap- ring in approximately 1% of native kidney biopsies in several large biopsy series proximately 16 nm in thickness. Podo- obtained from Western countries. The distinctive features are infiltration of glo- cyte foot processes were diffusely merular structures by randomly arranged fibrils similar in appearance but larger effaced. There was no evidence of than amyloid fibrils and the lack of staining with histochemical dyes typically fibrillary deposits in the tubular base- reactive with amyloid. It is widely but not universally recognized to be distinct from ment membranes or interstitium. The immunotactoid glomerulopathy, an entity characterized by glomerular deposits of diagnosis of fibrillary glomerulone- immunoglobulin with substructural organization as microtubules and with clinical phritis was established on the basis of associations with lymphoplasmacytic disorders. The pathophysiologic basis for the ultrastructural findings in conjunc- organization of the glomerular deposits as fibrils or microtubules in these entities tion with the negative Congo Red stain remains obscure. and typical histologic and immunohis- J Am Soc Nephrol 19: 34–37, 2008. doi: -
Minimal Change Glomerulonephritis (GN)
Patient information – Minimal Change Glomerulonephritis Minimal Change Glomerulonephritis (GN) What is it? Your kidney biopsy has shown that your swelling and protein leak (nephrotic syndrome) is caused by a condition called ‘Minimal Change Glomerulonephritis’. This is an inflammation in the glomeruli (the network of blood capillaries) of the kidney, which shows very little change looking down the ordinary microscope. More specialised tests (such as electron microscopy) on the biopsy show characteristic changes to make this diagnosis. It is the commonest cause of nephrotic syndrome in children and causes about a quarter of those in adults. While the symptoms can be quite unpleasant, it does not cause long- term damage to the kidney function. While many types of nephrotic syndrome cannot be treated, Minimal Change GN will respond to steroid treatment. Initial treatment This stops the protein leak in 94 –100% of cases. The main treatment is high dose Prednisolone (steroids) tablets for up to 16 weeks (although usually less time). You will be seen every two weeks, and once the urine is clear of protein, the dose will be gradually reduced over the following six months. Prednisolone 1mg/kg of body weight (max 80mg) daily Lansoprazole 30mg daily Alendronate 70mg weekly Nystatin 1ml four times a day Septrin 480mg daily As steroids may have many side effects, you will also be given additional medication to protect you from some of the more serious ones. Some possible side effects of the steroids · Infection: Steroids make you more prone to ‘opportunist infection’ (so-called, because they only affect vulnerable people). You will be given antibiotics (Septrin and Fluconazole), to protect against thrush and pneumonia. -

A Narrative Review on C3 Glomerulopathy: a Rare Renal Disease
International Journal of Molecular Sciences Review A Narrative Review on C3 Glomerulopathy: A Rare Renal Disease Francesco Paolo Schena 1,2,*, Pasquale Esposito 3 and Michele Rossini 1 1 Department of Emergency and Organ Transplantation, Renal Unit, University of Bari, 70124 Bari, Italy; [email protected] 2 Schena Foundation, European Center for the Study of Renal Diseases, 70010 Valenzano, Italy 3 Department of Internal Medicine, Division of Nephrology, Dialysis and Transplantation, University of Genoa and IRCCS Ospedale Policlinico San Martino, 16132 Genova, Italy; [email protected] * Correspondence: [email protected] Received: 5 December 2019; Accepted: 10 January 2020; Published: 14 January 2020 Abstract: In April 2012, a group of nephrologists organized a consensus conference in Cambridge (UK) on type II membranoproliferative glomerulonephritis and decided to use a new terminology, “C3 glomerulopathy” (C3 GP). Further knowledge on the complement system and on kidney biopsy contributed toward distinguishing this disease into three subgroups: dense deposit disease (DDD), C3 glomerulonephritis (C3 GN), and the CFHR5 nephropathy. The persistent presence of microhematuria with or without light or heavy proteinuria after an infection episode suggests the potential onset of C3 GP. These nephritides are characterized by abnormal activation of the complement alternative pathway, abnormal deposition of C3 in the glomeruli, and progression of renal damage to end-stage kidney disease. The diagnosis is based on studying the complement system, relative genetics, and kidney biopsies. The treatment gap derives from the absence of a robust understanding of their natural outcome. Therefore, a specific treatment for the different types of C3 GP has not been established. -

Proteinuria and Nephrotic Syndrome
Proteinuria and Nephrotic Syndrome Rebecca Hjorten, MD Division of Nephrology Speaker Disclosures • Relevant Financial Relationships: No disclosure. • Relevant Nonfinancial Relationships: No disclosure. • I have no actual or potential conflict of interest in relation to this program/presentation. Division of NephrologyDivision of Nephrology Urine Dip Concern for Positive for Urine Positive for Glomerulonephritis Protein Protein AND Blood (GN) …PIGN, MPGN, IgA, HSP Lupus, ANCA vasculitis, Urine Positive for Anti-GBM Asymptomatic Protein AND NORMAL Concerning Ex. Nephrotic Syndrome False Positive Symptoms Non-Significant Levels Persistent of Urine Protein Asymptomatic Consider Proteinuria Further Orthostatic Proteinuria Evaluation and Referral to Transient Proteinuria Pediatric Nephrology Division of Nephrology Urine Dip Concern for Positive for Urine Positive for Glomerulonephritis Protein Protein AND Blood (GN) …PIGN, MPGN, IgA, HSP Lupus, ANCA vasculitis, Urine Positive for Anti-GBM Asymptomatic Protein AND NORMAL Concerning Ex. Nephrotic Syndrome False Positive Symptoms Non-Significant Levels Persistent of Urine Protein Asymptomatic Consider Proteinuria Further Orthostatic Proteinuria Evaluation and Referral to Transient Proteinuria Pediatric Nephrology Division of Nephrology Objectives • Asymptomatic Proteinuria without Hematuria • Identification of transient and orthostatic proteinuria • Initial workup and referral or persistent proteinuria • Nephrotic syndrome • Early recognition of nephrotic syndrome • Initiation of management • -

Acute Glomerulonephritis C S Vinen,Dbgoliveira
206 BEST PRACTICE Postgrad Med J: first published as 10.1136/pmj.79.930.206 on 1 April 2003. Downloaded from Acute glomerulonephritis C S Vinen,DBGOliveira ............................................................................................................................. Postgrad Med J 2003;79:206–213 Glomerulonephritis is an important cause of renal failure lung and glomerulus.2 In post-streptococcal thought to be caused by autoimmune damage to the glomerulonephritis antibodies are formed not to an endogenous antigen but to an exogenous kidney. While each type of glomerulonephritis begins streptococcal antigen planted in the glomerulus with a unique initiating stimulus, subsequent common at the time of infection.3 In systemic lupus erythematosus and IgA nephropathy, the antigen inflammatory and fibrotic events lead to a final pathway antibody reaction occurs not only in situ in the of progressive renal damage. In this article the different glomerulus but also systemically with subsequent forms of inflammatory glomerulonephritis and their trapping of complexes in the kidney. Finally in the glomerulonephritis seen in small vessel vasculitis, diagnosis are discussed. In a review of therapy both cellular rather than humoral immune responses immediate life saving treatment given when are thought to be stimulated, with inflammation glomerulonephritis causes acute renal failure and more often originating in organs distant to the kidney with a subsequent renal influx of T-cellsand mac- specific treatments designed to modify the underlying -

Acute Poststreptococcal Glomerulonephritis: Immune Deposit Disease * ALFRED F
Journal of Clinical Investigation Vol. 45, No. 2, 1966 Acute Poststreptococcal Glomerulonephritis: Immune Deposit Disease * ALFRED F. MICHAEL, JR.,t KEITH N. DRUMMOND,t ROBERT A. GOOD,§ AND ROBERT L. VERNIER || WITH THE TECHNICAL ASSISTANCE OF AGNES M. OPSTAD AND JOYCE E. LOUNBERG (From the Pediatric Research Laboratories of the Variety Club Heart Hospital and the Department of Pediatrics, University of Minnesota, Minneapolis, Minn.) The possible role of immunologic mechanisms in the kidney in acute glomerulonephritis have also acute poststreptococcal glomerulonephritis was revealed the presence of discrete electron dense suggested in 1908 by Schick (2), who compared masses adjacent to the epithelial surface of the the delay in appearance of serum sickness after glomerular basement membrane (11-18). injection of heterologous serum to the latent pe- The purpose of this paper is to describe immuno- riod between scarlet fever and onset of acute glo- fluorescent and electron microscopic observations merulonephritis. Evidence in support of this con- of the kidney in 16 children with acute poststrepto- cept is the depression of serum complement during coccal glomerulonephritis. This study demon- the early stages of the disease (3) and glomerular strates 1) the presence of discrete deposits of yG- localization of immunoglobulin. Immunofluores- and fl3c-globulins along the glomerular basement cent studies have revealed either no glomerular membrane and its epithelial surface that are similar deposition of a-globulin (4) or a diffuse involve- in size and location to the dense masses seen by ment of the capillary wall (5-9). Seegal, Andres, both thin section microscopy and electron micros- Hsu, and Zabriskie (10) demonstrated the pres- copy; 2) the characteristic and unique specificity of ence of 7 S y-globulin, /31c-globulin, and strepto- this lesion in acute poststreptococcal glomerulo- coccal antigen in the glomeruli of most patients nephritis, its difference from other glomerular dis- with this disease. -

Redalyc.Nephritic Syndrome Associated to Skin Infection
Colombia Médica ISSN: 0120-8322 [email protected] Universidad del Valle Colombia Barrios, Emil Julio; Guerrero, Gustavo Adolfo Nephritic syndrome associated to skin infection, hepatitis A, and pneumonia: a case report Colombia Médica, vol. 41, núm. 2, abril-junio, 2010, pp. 171-175 Universidad del Valle Cali, Colombia Available in: http://www.redalyc.org/articulo.oa?id=28316817009 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Colombia Médica Vol. 41 Nº 2, 2010 (Abril-Junio) Nephritic syndrome associated to skin infection, hepatitis A, and pneumonia: a case report EMIL JULIO B ARRIOS, MD1, G USTAVO ADOLFO G UERRERO, MD2 SUMMARY Introduction: Glomerulonephritis is the most common cause of acute and chronic renal disease. The prototype of acute glomerulonephritis is acute post-infectious glomerulonephritis. Recently, increased cases of glomerulopathy have been associated with bacterial, viral, and other infections. Acute nephritic syndrome is part of glomerulonephritis with an acute beginning, characterized by hematuria, hypertension, edema, and oliguria due to the reduction of glomerular filtration reflected in an increase of nitrogen compounds. Development: This paper shows a male infant at 2 years and 7 months of age with nephritic syndrome associated to a skin infection, pneumonia, and hepatitis A virus infection. Conclusion: Acute glomerulonephritis may be associated to streptococcus or another coincidental infection. Children with skin infection, hepatitis A, or pneumonia who reveal abnormal urinalysis, hypertension, azotemia, or oliguria should be evaluated for concomitant glomerulonephritis. -

Diffuse Proliferative Lupus Nephritis: Identification of Specific Pathologic Features Affecting Renal Outcome
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Kidney International, Vol. 25 (1984), pp. 689—6 95 Diffuse proliferative lupus nephritis: Identification of specific pathologic features affecting renal outcome HOWARD A. AUSTIN III, LARRY R. MUENZ, KATHLEEN M. JOYCE, TATIANA T. ANTONOVYCH, and JAMES E. BALOW Clinical Nephrology Service and Arthritis and Rheumatism Branch, National Institute of Arthritis, Diabetes and Digestive and Kidney Diseases; Clinical and Diagnostic Trials Section, National Cancer Institute, National Institutes of Health, Bethesda, Maiyland; and the Nephropathology Section, Armed Forces Institute of Pathology, Washington, D.C. Diffuse proliferative lupus nephritis: Identification of specific patholog- score semiquantitatif des caractéristiques histologiques individuelles et ic features affecting renal outcome. Prerandomization renal biopsy par des scores histologiques composites dérivés spéciflés par des Index specimens were examined in 102 patients upon entry into prospective d'ActivitC (Al) et de Chronicité (CI). Parmi les 72 malades atteints de therapeutic trials of lupus nephntis in an attempt to identify earlyDPGN/MPGN, l'AI composite était plus fortement prédictif d'une predictors of renal failure outcome. All 11 renal failures occurred insuffisance rCnale que les caracteristiques histologiques actives indivi- among the 72 individuals with diffuse proliferative or membranoproli- duelles; les croissants cellulaires et une nécrose fibrinoide étendue ferative glomerulonephritis (DPGN/MPGN); thus, these patients were donnaient des associations positives, alors que Ia proliferation endoca- at modestly, but significantly, increased risk of endstage renal disease pillaire, l'exsudation leucocytaire et des thrombus hyalins dans les compared to those with focal proliferative, membranous, or mesangial glomerules, ainsi que l'inflammation interstitielle en eux-mêmes, n'ap- glomerulonephritis.