Iga Nephropathy Information for Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinicopathologic Characteristics of Iga Nephropathy with Steroid-Responsive Nephrotic Syndrome
J Korean Med Sci 2009; 24 (Suppl 1): S44-9 Copyright � The Korean Academy ISSN 1011-8934 of Medical Sciences DOI: 10.3346/jkms.2009.24.S1.S44 Clinicopathologic Characteristics of IgA Nephropathy with Steroid-responsive Nephrotic Syndrome Nephrotic syndrome is an unusual manifestation of IgA Nephropathy (IgAN). Some Sun Moon Kim, Kyung Chul Moon*, cases respond to steroid treatment. Here we describe a case-series of IgAN patients Kook-Hwan Oh, Kwon Wook Joo, with steroid-responsive nephrotic syndrome. Twelve patients with IgAN with steroid- Yon Su Kim, Curie Ahn, responsive nephrotic syndrome were evaluated and followed up. All patients pre- Jin Suk Han, and Suhnggwon Kim sented with generalized edema. Renal insufficiency was found in two patients. The Departments of Internal Medicine, and Pathology*, renal biopsy of eight patients revealed wide foot process effacement in addition to Seoul National University College of Medicine, Seoul, the typical features of IgAN. They showed complete remission after steroid thera- Korea py. Seven relapses were reported in five patients; six of the relapsed cases respond- ed to steroid therapy. Compared with steroid-non-responsive patients, the patients with steroid-responsive nephrotic syndrome had shorter symptom duration, more Received : 1 September 2008 weight gain, more proteinuria, and lower histologic grade than did those that had Accepted : 10 December 2008 steroid-non-responsive nephrotic syndrome at presentation. None of the respon- ders progressed to end stage renal disease, whereas five (38%) non-responders required dialysis or renal transplantation. Patients with IgAN who have steroid-respon- Address for correspondence sive nephrotic syndrome likely have both minimal change disease and IgAN. -

Glomerulonephritis Management in General Practice
Renal disease • THEME Glomerulonephritis Management in general practice Nicole M Isbel MBBS, FRACP, is Consultant Nephrologist, Princess Alexandra lomerular disease remains an important cause Hospital, Brisbane, BACKGROUND Glomerulonephritis (GN) is an G and Senior Lecturer in important cause of both acute and chronic kidney of renal impairment (and is the commonest cause Medicine, University disease, however the diagnosis can be difficult of end stage kidney disease [ESKD] in Australia).1 of Queensland. nikky_ due to the variability of presenting features. Early diagnosis is essential as intervention can make [email protected] a significant impact on improving patient outcomes. OBJECTIVE This article aims to develop However, presentation can be variable – from indolent a structured approach to the investigation of patients with markers of kidney disease, and and asymptomatic to explosive with rapid loss of kidney promote the recognition of patients who need function. Pathology may be localised to the kidney or further assessment. Consideration is given to the part of a systemic illness. Therefore diagnosis involves importance of general measures required in the a systematic approach using a combination of clinical care of patients with GN. features, directed laboratory and radiological testing, DISCUSSION Glomerulonephritis is not an and in many (but not all) cases, a kidney biopsy to everyday presentation, however recognition establish the histological diagnosis. Management of and appropriate management is important to glomerulonephritis (GN) involves specific therapies prevent loss of kidney function. Disease specific directed at the underlying, often immunological cause treatment of GN may require specialist care, of the disease and more general strategies aimed at however much of the management involves delaying progression of kidney impairment. -

A New Vision of Iga Nephropathy: the Missing Link
International Journal of Molecular Sciences Review A New Vision of IgA Nephropathy: The Missing Link Fabio Sallustio 1,2,* , Claudia Curci 2,3,* , Vincenzo Di Leo 3 , Anna Gallone 2, Francesco Pesce 3 and Loreto Gesualdo 3 1 Interdisciplinary Department of Medicine (DIM), University of Bari “Aldo Moro”, 70124 Bari, Italy 2 Department of Basic Medical Sciences, Neuroscience and Sense Organs, University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] 3 Nephrology, Dialysis and Transplantation Unit, DETO, University “Aldo Moro”, 70124 Bari, Italy; [email protected] (V.D.L.); [email protected] (F.P.); [email protected] (L.G.) * Correspondence: [email protected] (F.S.); [email protected] (C.C.) Received: 7 December 2019; Accepted: 24 December 2019; Published: 26 December 2019 Abstract: IgA Nephropathy (IgAN) is a primary glomerulonephritis problem worldwide that develops mainly in the 2nd and 3rd decade of life and reaches end-stage kidney disease after 20 years from the biopsy-proven diagnosis, implying a great socio-economic burden. IgAN may occur in a sporadic or familial form. Studies on familial IgAN have shown that 66% of asymptomatic relatives carry immunological defects such as high IgA serum levels, abnormal spontaneous in vitro production of IgA from peripheral blood mononuclear cells (PBMCs), high serum levels of aberrantly glycosylated IgA1, and an altered PBMC cytokine production profile. Recent findings led us to focus our attention on a new perspective to study the pathogenesis of this disease, and new studies showed the involvement of factors driven by environment, lifestyle or diet that could affect the disease. -

Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis
Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis MATTHEW D. GRIFFIN,* JOHANNES BJORNSSON,t and STEPHEN B. ERICKSON* *Department of Internal Medicine, Division of Nephrology, and tDepartment of Pathology, Mayo Clinic and Mayo Foundation, Rochester, Minnesota. Abstract. A 72-year-old man developed acute renal failure after peated surgical debridement. Spontaneous recovery of renal coronary bypass surgery that had been complicated by sternal function occurred after eradication of infection and final sur- osteomyelitis caused by the Staphylococcus aureus bacterium. gical wound repair. The relationship between acute bacterial Bacteremia and sepsis were not present. Renal biopsy demon- infections and glomerulonephritis and, in particular, the causal strated a florid, diffuse, proliferative glomerulonephritis with role of staphylococcal antigens in the pathogenesis of such glomerular immune complex deposition. Management in- lesions is discussed. (J Am Soc Nephrol 8: 1633-1639, 1997) cluded hemodialysis, prolonged antibiotic therapy, and re- Coagulase-positive staphylococcus (Staphylococcus aureus) is mg/dl]) and in the immediate postoperative period. Over the the most common causative organism in acute osteomyelitis following days, the patient’s serum creatinine concentration (1). Along with coagulase-negative staphylococcal species, it increased progressively, and hemodialysis was instituted on has also been implicated in the pathogenesis of immune com- day 23 after CABG. There was no past or family history of plex (IC)-mediated diffuse proliferative glomerulonephritis renal disease and no known drug allergies. Prior medical (DPGN) in a variety of infections. These include bacterial history had included degenerative disc disease, stable abdom- endocarditis, ventriculoatrial shunt infections, pneumonia, and inal aortic aneurysm, stable benign prostatic hyperplasia, and visceral abscesses with or without septicemia (2-6). -

Glomerulonephritis
Adolesc Med 16 (2005) 67–85 Glomerulonephritis Keith K. Lau, MDa,b, Robert J. Wyatt, MD, MSa,b,* aDivision of Pediatric Nephrology, Department of Pediatrics, University of Tennessee Health Sciences Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA bChildren’s Foundation Research Center at the Le Bonheur Children’s Medical Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA Early diagnosis of glomerulonephritis (GN) in the adolescent is important in initiating appropriate treatment and controlling chronic glomerular injury that may eventually lead to end-stage renal disease (ESRD). The spectrum of GN in adolescents is more similar to that seen in young and middle-aged adults than to that observed in prepubertal children. In this article, the authors discuss the clinical features associated with GN and the diagnostic evaluation required to determine the specific type of GN. With the exception of hereditary nephritis (Alport’s disease), virtually all types of GN are immunologically mediated with glomerular deposition of immunoglobulins and complement proteins. The inflammatory events leading to GN may be triggered by a number of factors. Most commonly, immune complexes deposit in the glomeruli or are formed in situ with the antigen as a structural component of the glomerulus. The immune complexes then initiate the production of proinflammatory mediators, such as complement proteins and cytokines. Subsequently, the processes of sclerosis within the glomeruli and fibrosis in the tubulointerstitial cells lead to chronic or even irreversible renal injury [1]. Less commonly, these processes occur without involvement of immune complexes—so-called ‘‘pauci-immune GN.’’ * Corresponding author. -

Iga Nephropathy in Systemic Lupus Erythematosus Patients
r e v b r a s r e u m a t o l . 2 0 1 6;5 6(3):270–273 REVISTA BRASILEIRA DE REUMATOLOGIA w ww.reumatologia.com.br Case report IgA nephropathy in systemic lupus erythematosus patients: case report and literature review Leonardo Sales da Silva, Bruna Laiza Fontes Almeida, Ana Karla Guedes de Melo, Danielle Christine Soares Egypto de Brito, Alessandra Sousa Braz, ∗ Eutília Andrade Medeiros Freire School of Medicine, Universidade Federal da Paraíba, João Pessoa, PB, Brazil a r t i c l e i n f o a b s t r a c t Article history: Systemic erythematosus lupus (SLE) is a multisystemic autoimmune disease which has Received 1 August 2014 nephritis as one of the most striking manifestations. Although it can coexist with other Accepted 19 October 2014 autoimmune diseases, and determine the predisposition to various infectious complica- Available online 16 February 2015 tions, SLE is rarely described in association with non-lupus nephropathies etiologies. We report the rare association of SLE and primary IgA nephropathy (IgAN), the most frequent Keywords: primary glomerulopathy in the world population. The patient was diagnosed with SLE due to the occurrence of malar rash, alopecia, pleural effusion, proteinuria, ANA 1: 1280, nuclear Systemic lupus erythematosus IgA nephropathy fine speckled pattern, and anticardiolipin IgM and 280 U/mL. Renal biopsy revealed mesan- Glomerulonephritis gial hypercellularity with isolated IgA deposits, consistent with primary IgAN. It was treated with antimalarial drug, prednisone and inhibitor of angiotensin converting enzyme, show- ing good progress. Since they are relatively common diseases, the coexistence of SLE and IgAN may in fact be an uncommon finding for unknown reasons or an underdiagnosed con- dition. -

Iga Vasculitis and Iga Nephropathy: Same Disease?
Journal of Clinical Medicine Review IgA Vasculitis and IgA Nephropathy: Same Disease? Evangeline Pillebout 1,2 1 Nephrology Unit, Saint-Louis Hospital, 75010 Paris, France; [email protected] 2 INSERM 1149, Center of Research on Inflammation, 75870 Paris, France Abstract: Many authors suggested that IgA Vasculitis (IgAV) and IgA Nephropathy (IgAN) would be two clinical manifestations of the same disease; in particular, that IgAV would be the systemic form of the IgAN. A limited number of studies have included sufficient children or adults with IgAN or IgAV (with or without nephropathy) and followed long enough to conclude on differences or similarities in terms of clinical, biological or histological presentation, physiopathology, genetics or prognosis. All therapeutic trials available on IgAN excluded patients with vasculitis. IgAV and IgAN could represent different extremities of a continuous spectrum of the same disease. Due to skin rash, patients with IgAV are diagnosed precociously. Conversely, because of the absence of any clinical signs, a renal biopsy is practiced for patients with an IgAN to confirm nephropathy at any time of the evolution of the disease, which could explain the frequent chronic lesions at diagnosis. Nevertheless, the question that remains unsolved is why do patients with IgAN not have skin lesions and some patients with IgAV not have nephropathy? Larger clinical studies are needed, including both diseases, with a common histological classification, and stratified on age and genetic background to assess renal prognosis and therapeutic strategies. Keywords: IgA Vasculitis; IgA Nephropathy; adults; children; presentation; physiopathology; genetics; prognosis; treatment Citation: Pillebout, E. IgA Vasculitis and IgA Nephropathy: Same 1. -

Henoch-Schonlein Purpura and Iga Nephropathy: Are They the Same Disease?
Henoch-Schonlein Purpura and IgA Nephropathy: are they the same disease? Shaun Jackson, MD Division of Pediatric Nephrology and Pediatric Rheumatology, Dept. of Pediatrics, University of Washington; Seattle Children’s Hospital Division of Nephrology HSP nephritis vs. IgA nephropathy? Division of NephrologyDivision of Nephrology Disease spectrum or distinct entities? 1. Case report: Single patient with biopsy-proven IgA nephropathy then HSP nephritis. 2. Care report: Identical twins with adenovirus infection and subsequent development of HSP nephritis (rash, abdominal pain, plus renal disease) and renal-limited IgA nephropathy. 1. Ravelli, et al. Nephron 1996;72:111–112 2. Meadow, et al. Journal of Pediatrics 106 (1) 1985. Division of NephrologyDivision of Nephrology Pathogenesis: HSP and IgA nephropathy * Davin, J.-C. & Coppo, R. Nat. Rev. Nephrol. 2014. * Rodrigues,et al. Clin J Am Soc Nephrol 12: 677–686, 2017. Division of NephrologyDivision of Nephrology Henoch Schönlein Purpura vs. IgA nephropathy Despite similar histopathology findings and possibly overlapping pathophysiology, HSP and IgA nephropathy have distinct clinical presentations, epidemiology, and long-term prognoses. Division of NephrologyDivision of Nephrology Henoch Schönlein Purpura (HSP): A case… • Phone call No. 1 (ED): 5 yo F with pain and swelling of bilateral knees, wrists and ankles for last 2 days. Mild URI symptoms for last week. No fever or rash. No sick contacts. • Phone call No. 2 (PCP): 2 days later, called by patient’s primary care physician. Joints still swollen…”is this JRA?” • Phone call No. 3 (ED): Back to Seattle Children’s ED with persistent joint pain/swelling and new rash…demanding that something be done. -
Nephritis Fact Sheet
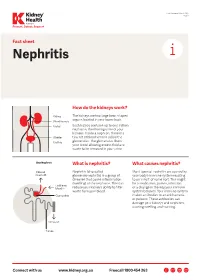
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine. -

Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy
PATHOPHYSIOLOGY of the RENAL BIOPSY www.jasn.org Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy Charles E. Alpers and Jolanta Kowalewska Department of Pathology, University of Washington, Seattle, Washington ABSTRACT extracellular accumulation of haphaz- Fibrillary glomerulonephritis is a now widely recognized diagnostic entity, occur- ardly arranged fibrils measuring ap- ring in approximately 1% of native kidney biopsies in several large biopsy series proximately 16 nm in thickness. Podo- obtained from Western countries. The distinctive features are infiltration of glo- cyte foot processes were diffusely merular structures by randomly arranged fibrils similar in appearance but larger effaced. There was no evidence of than amyloid fibrils and the lack of staining with histochemical dyes typically fibrillary deposits in the tubular base- reactive with amyloid. It is widely but not universally recognized to be distinct from ment membranes or interstitium. The immunotactoid glomerulopathy, an entity characterized by glomerular deposits of diagnosis of fibrillary glomerulone- immunoglobulin with substructural organization as microtubules and with clinical phritis was established on the basis of associations with lymphoplasmacytic disorders. The pathophysiologic basis for the ultrastructural findings in conjunc- organization of the glomerular deposits as fibrils or microtubules in these entities tion with the negative Congo Red stain remains obscure. and typical histologic and immunohis- J Am Soc Nephrol 19: 34–37, 2008. doi: -

Recurrent Adult Onset Henoch-Schonlein Purpura: a Case Report
UC Davis Dermatology Online Journal Title Recurrent adult onset Henoch-Schonlein Purpura: a case report Permalink https://escholarship.org/uc/item/1r12k2z1 Journal Dermatology Online Journal, 22(8) Authors Gaskill, Neil Guido, Bruce Mago, Cynthia Publication Date 2016 DOI 10.5070/D3228032191 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 22 Number 8 August 2016 Case Report Recurrent adult onset Henoch-Schonlein Purpura: a case report Neil Gaskill1 DO, Bruce Guido2 MD, Cynthia Magro3 MD 1Delaware County Memorial Hospital, Drexel Hill, PA 2Ashtabula County Medical Center, Ashtabula, OH 3Department of Pathology, Weill Cornell Medicine, New York Dermatology Online Journal 22 (8): 5 Correspondence: Cynthia Magro MD Weill Cornell Medicine Department of Pathology & Laboratory Medicine 1300 York Avenue, F-309 New York, NY 10065 Tel. 212-746-6434 Fax. 212-746-8570 Email: [email protected] Abstract Henoch-Schonlein purpura is an immunoglobulin A (IgA)-immune complex mediated leukocytoclastic vasculitis that classically manifests with palpable purpura, abdominal pain, arthritis, and hematuria or proteinuria. The condition is much more predominant in children (90% of cases) and commonly follows an upper respiratory infection. We present a case of recurrent Henoch- Schonlein purpura (HSP) complicated by nephritis in an adult female initially categorized as IgA nephropathy (IgAN). We review the pathophysiologic basis of HSP nephritis as the variant of HSP accompanied by renal involvement and its pathogenetic commonality with IgA nephropathy. Key Words: Henoch-Schonlein purpura, IgA nephropathy, leukocytoclastic vasculitis Introduction Henoch-Schonlein purpura is an IgA-immune complex mediated leukocytoclastic small vessel vasculitis that predominantly affects children. -
Minimal Change Glomerulonephritis (GN)
Patient information – Minimal Change Glomerulonephritis Minimal Change Glomerulonephritis (GN) What is it? Your kidney biopsy has shown that your swelling and protein leak (nephrotic syndrome) is caused by a condition called ‘Minimal Change Glomerulonephritis’. This is an inflammation in the glomeruli (the network of blood capillaries) of the kidney, which shows very little change looking down the ordinary microscope. More specialised tests (such as electron microscopy) on the biopsy show characteristic changes to make this diagnosis. It is the commonest cause of nephrotic syndrome in children and causes about a quarter of those in adults. While the symptoms can be quite unpleasant, it does not cause long- term damage to the kidney function. While many types of nephrotic syndrome cannot be treated, Minimal Change GN will respond to steroid treatment. Initial treatment This stops the protein leak in 94 –100% of cases. The main treatment is high dose Prednisolone (steroids) tablets for up to 16 weeks (although usually less time). You will be seen every two weeks, and once the urine is clear of protein, the dose will be gradually reduced over the following six months. Prednisolone 1mg/kg of body weight (max 80mg) daily Lansoprazole 30mg daily Alendronate 70mg weekly Nystatin 1ml four times a day Septrin 480mg daily As steroids may have many side effects, you will also be given additional medication to protect you from some of the more serious ones. Some possible side effects of the steroids · Infection: Steroids make you more prone to ‘opportunist infection’ (so-called, because they only affect vulnerable people). You will be given antibiotics (Septrin and Fluconazole), to protect against thrush and pneumonia.