Acute Glomerulonephritis and the Nephrotic Syndrome
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Glomerulonephritis Management in General Practice
Renal disease • THEME Glomerulonephritis Management in general practice Nicole M Isbel MBBS, FRACP, is Consultant Nephrologist, Princess Alexandra lomerular disease remains an important cause Hospital, Brisbane, BACKGROUND Glomerulonephritis (GN) is an G and Senior Lecturer in important cause of both acute and chronic kidney of renal impairment (and is the commonest cause Medicine, University disease, however the diagnosis can be difficult of end stage kidney disease [ESKD] in Australia).1 of Queensland. nikky_ due to the variability of presenting features. Early diagnosis is essential as intervention can make [email protected] a significant impact on improving patient outcomes. OBJECTIVE This article aims to develop However, presentation can be variable – from indolent a structured approach to the investigation of patients with markers of kidney disease, and and asymptomatic to explosive with rapid loss of kidney promote the recognition of patients who need function. Pathology may be localised to the kidney or further assessment. Consideration is given to the part of a systemic illness. Therefore diagnosis involves importance of general measures required in the a systematic approach using a combination of clinical care of patients with GN. features, directed laboratory and radiological testing, DISCUSSION Glomerulonephritis is not an and in many (but not all) cases, a kidney biopsy to everyday presentation, however recognition establish the histological diagnosis. Management of and appropriate management is important to glomerulonephritis (GN) involves specific therapies prevent loss of kidney function. Disease specific directed at the underlying, often immunological cause treatment of GN may require specialist care, of the disease and more general strategies aimed at however much of the management involves delaying progression of kidney impairment. -

Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis
Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis MATTHEW D. GRIFFIN,* JOHANNES BJORNSSON,t and STEPHEN B. ERICKSON* *Department of Internal Medicine, Division of Nephrology, and tDepartment of Pathology, Mayo Clinic and Mayo Foundation, Rochester, Minnesota. Abstract. A 72-year-old man developed acute renal failure after peated surgical debridement. Spontaneous recovery of renal coronary bypass surgery that had been complicated by sternal function occurred after eradication of infection and final sur- osteomyelitis caused by the Staphylococcus aureus bacterium. gical wound repair. The relationship between acute bacterial Bacteremia and sepsis were not present. Renal biopsy demon- infections and glomerulonephritis and, in particular, the causal strated a florid, diffuse, proliferative glomerulonephritis with role of staphylococcal antigens in the pathogenesis of such glomerular immune complex deposition. Management in- lesions is discussed. (J Am Soc Nephrol 8: 1633-1639, 1997) cluded hemodialysis, prolonged antibiotic therapy, and re- Coagulase-positive staphylococcus (Staphylococcus aureus) is mg/dl]) and in the immediate postoperative period. Over the the most common causative organism in acute osteomyelitis following days, the patient’s serum creatinine concentration (1). Along with coagulase-negative staphylococcal species, it increased progressively, and hemodialysis was instituted on has also been implicated in the pathogenesis of immune com- day 23 after CABG. There was no past or family history of plex (IC)-mediated diffuse proliferative glomerulonephritis renal disease and no known drug allergies. Prior medical (DPGN) in a variety of infections. These include bacterial history had included degenerative disc disease, stable abdom- endocarditis, ventriculoatrial shunt infections, pneumonia, and inal aortic aneurysm, stable benign prostatic hyperplasia, and visceral abscesses with or without septicemia (2-6). -

Urinary System Diseases and Disorders
URINARY SYSTEM DISEASES AND DISORDERS BERRYHILL & CASHION HS1 2017-2018 - CYSTITIS INFLAMMATION OF THE BLADDER CAUSE=PATHOGENS ENTERING THE URINARY MEATUS CYSTITIS • MORE COMMON IN FEMALES DUE TO SHORT URETHRA • SYMPTOMS=FREQUENT URINATION, HEMATURIA, LOWER BACK PAIN, BLADDER SPASM, FEVER • TREATMENT=ANTIBIOTICS, INCREASE FLUID INTAKE GLOMERULONEPHRITIS • AKA NEPHRITIS • INFLAMMATION OF THE GLOMERULUS • CAN BE ACUTE OR CHRONIC ACUTE GLOMERULONEPHRITIS • USUALLY FOLLOWS A STREPTOCOCCAL INFECTION LIKE STREP THROAT, SCARLET FEVER, RHEUMATIC FEVER • SYMPTOMS=CHILLS, FEVER, FATIGUE, EDEMA, OLIGURIA, HEMATURIA, ALBUMINURIA ACUTE GLOMERULONEPHRITIS • TREATMENT=REST, SALT RESTRICTION, MAINTAIN FLUID & ELECTROLYTE BALANCE, ANTIPYRETICS, DIURETICS, ANTIBIOTICS • WITH TREATMENT, KIDNEY FUNCTION IS USUALLY RESTORED, & PROGNOSIS IS GOOD CHRONIC GLOMERULONEPHRITIS • REPEATED CASES OF ACUTE NEPHRITIS CAN CAUSE CHRONIC NEPHRITIS • PROGRESSIVE, CAUSES SCARRING & SCLEROSING OF GLOMERULI • EARLY SYMPTOMS=HEMATURIA, ALBUMINURIA, HTN • WITH DISEASE PROGRESSION MORE GLOMERULI ARE DESTROYED CHRONIC GLOMERULONEPHRITIS • LATER SYMPTOMS=EDEMA, FATIGUE, ANEMIA, HTN, ANOREXIA, WEIGHT LOSS, CHF, PYURIA, RENAL FAILURE, DEATH • TREATMENT=LOW NA DIET, ANTIHYPERTENSIVE MEDS, MAINTAIN FLUIDS & ELECTROLYTES, HEMODIALYSIS, KIDNEY TRANSPLANT WHEN BOTH KIDNEYS ARE SEVERELY DAMAGED PYELONEPHRITIS • INFLAMMATION OF THE KIDNEY & RENAL PELVIS • CAUSE=PYOGENIC (PUS-FORMING) BACTERIA • SYMPTOMS=CHILLS, FEVER, BACK PAIN, FATIGUE, DYSURIA, HEMATURIA, PYURIA • TREATMENT=ANTIBIOTICS, -

Role of Urinalysis in the Diagnosis of Chronic Kidney Disease (CKD)
Research and Reviews Role of Urinalysis in the Diagnosis of Chronic Kidney Disease (CKD) JMAJ 54(1): 27–30, 2011 Kunitoshi ISEKI*1 Abstract As of the end of Year 2008, 1 out of 450 people was a dialysis patient in Japan, and patients with chronic kidney disease (CKD) at stages 3 and 4 accounted for nearly 10% of the total population. An epidemiological study in Okinawa that used the introduction of dialysis treatment as the outcome revealed that the 10-year cumulative incident rate of end-stage renal disease (ESRD) was about 3% of the participants who were positive (Ն 1ϩ) for both proteinuria and hematuria, while there was hardly any difference between those who were positive for hematuria alone and those who were negative for both proteinuria and hematuria. When the incidence of ESRD (dialysis introduction) was examined in relation to the severity of proteinuria (5 grades ranging from [Ϫ] to [Ն 3ϩ]) as determined by dipstick, the cumulative incidence rate during the 17-year observation period was 16% for proteinuria (Ն 3ϩ) and about 7% for proteinuria (2ϩ). In contrast, among participants who were negative for proteinuria, the rate of dialysis introduction in 10 years is about 1 out of 1 million. The CKD Practice Guide of the Japanese Society of Nephrology recommends referral to a nephrologist when a case meets any of the following 3 criteria: 1) 0.5g/g creatinine or higher, or proteinuria (Ն 2ϩ), 2) an estimated glomerular filtration rate of less than 50ml/min/1.73m2, or 3) positive results (Ն 1ϩ) for both proteinuria and hematuria tests. -

Hematuria in the Child
Hematuria and Proteinuria in the Pediatric Patient Laurie Fouser, MD Pediatric Nephrology Swedish Pediatric Specialty Care Hematuria in the Child • Definition • ³ 1+ on dipstick on three urines over three weeks • 5 RBCs/hpf on three fresh urines over three weeks • Prevalence • 4-6% for microscopic hematuria on a single specimen in school age children • 0.3-0.5% on repeated specimens Sources of Hematuria • Glomerular or “Upper Tract” – Dysmorphic RBCs and RBC casts – Tea or cola colored urine – Proteinuria, WBC casts, renal tubular cells • Non-Glomerular or “Lower Tract” – RBCs have normal morphology – Clots/ Bright red or pink urine The Glomerular Capillary Wall The Glomerular Capillary Wall Glomerular Causes of Hematuria • Benign or self-limiting – Benign Familial Hematuria – Exercise-Induced Hematuria – Fever-Induced Hematuria Glomerular Causes of Hematuria • Acute Glomerular Disease – Poststreptococcal/ Postinfectious – Henoch-Schönlein Purpura – Sickle Cell Disease – Hemolytic Uremic Syndrome Glomerular Causes of Hematuria • Chronic Glomerular Disease – IgA Nephropathy – Henoch-Schönlein Purpura or other Vasculitis – Alport Syndrome – SLE or other Collagen Vascular Disease – Proliferative Glomerulonephritis Non-Glomerular Hematuria • Extra-Renal • UTI • Benign urethralgia +/- meatal stenosis • Calculus • Vesicoureteral Reflux, Hydronephrosis • Foreign body • Rhabdomyosarcoma • AV M • Coagulation disorder Non-Glomerular Hematuria • Intra-Renal • Hypercalciuria • Polycystic Kidney Disease • Reflux Nephropathy with Renal Dysplasia • -

Hematuria Is a Risk Factor Towards End-Stage Renal
Nephrology and Renal Diseases Research Article Hematuria is a risk factor towards end-stage renal disease - A propensity score analysis Tomoko Shima* Department of Internal Medicine, Teikyo University School of Medicine, Tokyo, Japan Abstract Background: It remains unclear whether microscopic hematuria accelerates the progression of chronic kidney disease (CKD). Since the risk of microscopic hematuria was expected very weak, we employed a propensity score analysis. Methods: A retrospective CKD cohort of 803 participants in a single institution was analyzed. The degree of microscopic hematuria was scaled as 0, 0.5, 1, 2, 3 for negative, ±, 1+, 2+, 3+ in the urinary qualitative analysis by dipstick, respectively. Time-averaged microscopic hematuria (TA-MH) was calculated by trapezoidal rule. The propensity score was estimated using 23 baseline covariates by multivariate binary logistic regression for the threshold of TA-MH at ≥ 0.5 or ≥ 1.0. Kaplan-Meier analysis after propensity score matching was also examined. Results: The incidence rate of end-stage renal disease (ESRD) was 33.9 per 1,000 person-years over median follow-up of 4.3 years. A Cox regression analysis stratified by quintile on the propensity scores showed that TA-MH ≥ 0.5 was a risk for ESRD (HR 1.72, 95% CI 1.08-2.75, p = 0.023) but not TA-MH ≥ 1.0 (HR 1.34, 95% CI 0.76-2.40, p = 0.315). Kaplan-Meier analysis after propensity score matching reproduced the similar results (TA-MH ≥ 0.5, HR 1.80, 95% CI 1.03-3.12, p = 0.046; TA-MH ≥ 1.0, HR 1.73, 95% CI 0.84-3.54, p = 0.145). -

Blood Or Protein in the Urine: How Much of a Work up Is Needed?
Blood or Protein in the Urine: How much of a work up is needed? Diego H. Aviles, M.D. Disclosure • In the past 12 months, I have not had a significant financial interest or other relationship with the manufacturers of the products or providers of the services discussed in my presentation • This presentation will not include discussion of pharmaceuticals or devices that have not been approved by the FDA Screening Urinalysis • Since 2007, the AAP no longer recommends to perform screening urine dipstick • Testing based on risk factors might be a more effective strategy • Many practices continue to order screening urine dipsticks Outline • Hematuria – Definition – Causes – Evaluation • Proteinuria – Definition – Causes – Evaluation • Cases You are about to leave when… • 10 year old female seen for 3 day history URI symptoms and fever. Urine dipstick showed 2+ for blood and no protein. Questions? • What is the etiology for the hematuria? • What kind of evaluation should be pursued? • Is this an indication of a serious renal condition? • When to refer to a Pediatric Nephrologist? Hematuria: Definition • Dipstick > 1+ (large variability) – RBC vs. free Hgb – RBC lysis common • > 5 RBC/hpf in centrifuged urine • Can be – Microscopic – Macroscopic Hematuria: Epidemiology • Microscopic hematuria occurs 4-6% with single urine evaluation • 0.1-0.5% of school children with repeated testing • Gross hematuria occurs in 1/1300 Localization of Hematuria • Kidney – Brown or coke-colored urine – Cellular casts • Lower tract – Terminal gross hematuria – (Blood -

Glomerulonephritis
Adolesc Med 16 (2005) 67–85 Glomerulonephritis Keith K. Lau, MDa,b, Robert J. Wyatt, MD, MSa,b,* aDivision of Pediatric Nephrology, Department of Pediatrics, University of Tennessee Health Sciences Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA bChildren’s Foundation Research Center at the Le Bonheur Children’s Medical Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA Early diagnosis of glomerulonephritis (GN) in the adolescent is important in initiating appropriate treatment and controlling chronic glomerular injury that may eventually lead to end-stage renal disease (ESRD). The spectrum of GN in adolescents is more similar to that seen in young and middle-aged adults than to that observed in prepubertal children. In this article, the authors discuss the clinical features associated with GN and the diagnostic evaluation required to determine the specific type of GN. With the exception of hereditary nephritis (Alport’s disease), virtually all types of GN are immunologically mediated with glomerular deposition of immunoglobulins and complement proteins. The inflammatory events leading to GN may be triggered by a number of factors. Most commonly, immune complexes deposit in the glomeruli or are formed in situ with the antigen as a structural component of the glomerulus. The immune complexes then initiate the production of proinflammatory mediators, such as complement proteins and cytokines. Subsequently, the processes of sclerosis within the glomeruli and fibrosis in the tubulointerstitial cells lead to chronic or even irreversible renal injury [1]. Less commonly, these processes occur without involvement of immune complexes—so-called ‘‘pauci-immune GN.’’ * Corresponding author. -

An Unusual Cause of Glomerular Hematuria and Acute Kidney Injury in a Chronic Kidney Disease Patient During Warfarin Therapy Clara Santos, Ana M
11617 14/5/13 12:11 Página 400 http://www.revistanefrologia.com casos clínicos © 2013 Revista Nefrología. Órgano Oficial de la Sociedad Española de Nefrología An unusual cause of glomerular hematuria and acute kidney injury in a chronic kidney disease patient during warfarin therapy Clara Santos, Ana M. Gomes, Ana Ventura, Clara Almeida, Joaquim Seabra Department of Nephrology. Centro Hospitalar Vila Nova de Gaia. Vila Nova de Gaia (Portugal) Nefrologia 2013;33(3):400-3 doi:10.3265/Nefrologia.pre2012.Oct.11617 ABSTRACT Un caso inusual de hematuria glomerular y fracaso renal agudo en un paciente con enfermedad renal crónica Warfarin is a well-established cause of gross hematuria. durante terapia con warfarina However, impaired kidney function does not occur RESUMEN except in the rare instance of severe blood loss or clot La warfarina es una causa muy conocida de hematuria ma- formation that obstructs the urinary tract. It has been croscópica. Sin embargo, el deterioro de la función renal no ocurre salvo en el caso inusual de gran pérdida de sangre o recently described an entity called warfarin-related formación de coágulos que obstruyen el tracto urinario. Re- nephropathy, in which acute kidney injury is caused by cientemente se ha descrito una entidad denominada nefro- glomerular hemorrhage and renal tubular obstruction patía relacionada con la warfarina en la que el fracaso renal by red blood cell casts. We report a patient under agudo es provocado por hemorragia glomerular y obstruc- warfarin treatment with chronic kidney disease, ción tubular renal por cilindros de glóbulos rojos. Exponemos macroscopic hematuria and acute kidney injury. -

Hematuria: Blood in the Urine
Hematuria: Blood in the Urine National Kidney and Urologic Diseases Information Clearinghouse What is hematuria? Hematuria is blood in the urine. Two types of blood in the urine exist. Blood that can be seen in the urine is called gross hematu- U.S. Department of Health and ria. Blood that cannot be seen in the urine, Human Services except when examined with a microscope, is called microscopic hematuria. NATIONAL INSTITUTES OF HEALTH What are the symptoms of Kidneys hematuria? Most people with microscopic hematuria do not have symptoms. People with gross hematuria have urine that is pink, red, or cola-colored due to the presence of red blood cells (RBCs). Even a small amount of Bladder blood in the urine can cause urine to change Ureters color. In most cases, people with gross hematuria do not have other symptoms. However, people with gross hematuria that Urethra includes blood clots in the urine may have pain. The urinary tract What is the urinary tract? the two kidneys process about 200 quarts The urinary tract is the body’s drainage of blood to produce about 1 to 2 quarts of system for removing wastes and extra water. urine, composed of wastes and extra water. The urinary tract includes two kidneys, two The urine flows from the kidneys to the ureters, a bladder, and a urethra. The kid- bladder through tubes called ureters. The neys are two bean-shaped organs, each about bladder stores urine until releasing it through the size of a fist. They are located near the urination. When the bladder empties, urine middle of the back, just below the rib cage, flows out of the body through a tube called one on each side of the spine. -
Nephritis Fact Sheet
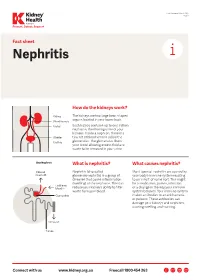
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine. -

Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy
PATHOPHYSIOLOGY of the RENAL BIOPSY www.jasn.org Fibrillary Glomerulonephritis and Immunotactoid Glomerulopathy Charles E. Alpers and Jolanta Kowalewska Department of Pathology, University of Washington, Seattle, Washington ABSTRACT extracellular accumulation of haphaz- Fibrillary glomerulonephritis is a now widely recognized diagnostic entity, occur- ardly arranged fibrils measuring ap- ring in approximately 1% of native kidney biopsies in several large biopsy series proximately 16 nm in thickness. Podo- obtained from Western countries. The distinctive features are infiltration of glo- cyte foot processes were diffusely merular structures by randomly arranged fibrils similar in appearance but larger effaced. There was no evidence of than amyloid fibrils and the lack of staining with histochemical dyes typically fibrillary deposits in the tubular base- reactive with amyloid. It is widely but not universally recognized to be distinct from ment membranes or interstitium. The immunotactoid glomerulopathy, an entity characterized by glomerular deposits of diagnosis of fibrillary glomerulone- immunoglobulin with substructural organization as microtubules and with clinical phritis was established on the basis of associations with lymphoplasmacytic disorders. The pathophysiologic basis for the ultrastructural findings in conjunc- organization of the glomerular deposits as fibrils or microtubules in these entities tion with the negative Congo Red stain remains obscure. and typical histologic and immunohis- J Am Soc Nephrol 19: 34–37, 2008. doi: