Diffuse Proliferative Lupus Nephritis: Identification of Specific Pathologic Features Affecting Renal Outcome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Case for Lupus Nephritis
Journal of Clinical Medicine Review Expanding the Role of Complement Therapies: The Case for Lupus Nephritis Nicholas L. Li * , Daniel J. Birmingham and Brad H. Rovin Department of Internal Medicine, Division of Nephrology, The Ohio State University, Columbus, OH 43210, USA; [email protected] (D.J.B.); [email protected] (B.H.R.) * Correspondence: [email protected]; Tel.: +1-614-293-4997; Fax: +1-614-293-3073 Abstract: The complement system is an innate immune surveillance network that provides defense against microorganisms and clearance of immune complexes and cellular debris and bridges innate and adaptive immunity. In the context of autoimmune disease, activation and dysregulation of complement can lead to uncontrolled inflammation and organ damage, especially to the kidney. Systemic lupus erythematosus (SLE) is characterized by loss of tolerance, autoantibody production, and immune complex deposition in tissues including the kidney, with inflammatory consequences. Effective clearance of immune complexes and cellular waste by early complement components protects against the development of lupus nephritis, while uncontrolled activation of complement, especially the alternative pathway, promotes kidney damage in SLE. Therefore, complement plays a dual role in the pathogenesis of lupus nephritis. Improved understanding of the contribution of the various complement pathways to the development of kidney disease in SLE has created an opportunity to target the complement system with novel therapies to improve outcomes in lupus nephritis. In this review, we explore the interactions between complement and the kidney in SLE and their implications for the treatment of lupus nephritis. Keywords: lupus nephritis; complement; systemic lupus erythematosus; glomerulonephritis Citation: Li, N.L.; Birmingham, D.J.; Rovin, B.H. -

Glomerulonephritis Management in General Practice
Renal disease • THEME Glomerulonephritis Management in general practice Nicole M Isbel MBBS, FRACP, is Consultant Nephrologist, Princess Alexandra lomerular disease remains an important cause Hospital, Brisbane, BACKGROUND Glomerulonephritis (GN) is an G and Senior Lecturer in important cause of both acute and chronic kidney of renal impairment (and is the commonest cause Medicine, University disease, however the diagnosis can be difficult of end stage kidney disease [ESKD] in Australia).1 of Queensland. nikky_ due to the variability of presenting features. Early diagnosis is essential as intervention can make [email protected] a significant impact on improving patient outcomes. OBJECTIVE This article aims to develop However, presentation can be variable – from indolent a structured approach to the investigation of patients with markers of kidney disease, and and asymptomatic to explosive with rapid loss of kidney promote the recognition of patients who need function. Pathology may be localised to the kidney or further assessment. Consideration is given to the part of a systemic illness. Therefore diagnosis involves importance of general measures required in the a systematic approach using a combination of clinical care of patients with GN. features, directed laboratory and radiological testing, DISCUSSION Glomerulonephritis is not an and in many (but not all) cases, a kidney biopsy to everyday presentation, however recognition establish the histological diagnosis. Management of and appropriate management is important to glomerulonephritis (GN) involves specific therapies prevent loss of kidney function. Disease specific directed at the underlying, often immunological cause treatment of GN may require specialist care, of the disease and more general strategies aimed at however much of the management involves delaying progression of kidney impairment. -
What Is Lupus Nephritis
What is lupus nephritis (LN)? Lupus nephritis (LN) is inflammation of the kidney that occurs as a common symptom of systemic lupus erythematosus (SLE), also known as lupus. Proteins in the immune system called antibodies damage important structures in the kidney. ⅱ Why are the kidneys important? To understand how lupus nephritis damages the kidney, it is important to understand how the kidneys work. The kidneys’ main function is to filter out excess waste and water from the blood through the urine. Kidneys also balance the salts and minerals circulating in the blood, help control blood pressure and make red blood cells. So, when the kidneys are damaged or fail, they can’t do their job as well. As a result, the kidneys are not able to filter out waste and water into the urine causing it to stay in the blood. What are the signs and symptoms of LN? Signs to ask the doctor about include blood in the urine or foamy urine which can mean that there is excess protein. Other signs to notice are swelling of legs, ankles, hands or tissue around the eyes as well as weight gain that can be caused by fluid the body isn’t getting rid of. ⅲ Symptoms of lupus nephritis also include high blood pressure, joint/muscle pain, high levels of waste (creatinine) in the blood, or impaired/failing kidney. ⅳ How common is LN? Lupus nephritis is the most common complication of lupus. Five out of 10 adults with lupus will have lupus nephritis, while eight out of 10 children with lupus will have kidney damage, which usually stems from lupus nephritis. -

Management of Lupus Nephritis
Journal of Clinical Medicine Review Management of Lupus Nephritis Farah Tamirou * and Frédéric A. Houssiau Department of Rheumatology, Cliniques Universitaires Saint-Luc and Institut de Recherche Expérimentale et Clinique, UCLouvain, 1200 Bruxelles, Belgium; [email protected] * Correspondence: [email protected] Abstract: Lupus nephritis (LN) is a frequent and severe manifestation of systemic lupus erythemato- sus. The main goal of the management of LN is to avoid chronic kidney disease (CKD). Current treatment strategies remain unsatisfactory in terms of complete renal response, prevention of relapses, CKD, and progression to end-stage kidney disease. To improve the prognosis of LN, recent data suggest that we should (i) modify our treat-to-target approach by including, in addition to a clinical target, a pathological target and (ii) switch from conventional sequential therapy to combination therapy. Here, we also review the results of recent controlled randomized trials. Keywords: lupus nephritis; treat-to-target approach; repeat kidney biopsy; combination therapy 1. Introduction Lupus nephritis (LN) occurs in 12 to 69% of patients suffering from systemic lupus erythematosus (SLE), depending on case series [1]. Based on clinical and laboratory findings, it affects around 50% of SLE patients, while the rates of biopsy-proven LN are somewhat lower [2]. LN is more prevalent in Asian than in African or Hispanic and European patients [3]. 2. Pathophysiology of Lupus Nephritis Citation: Tamirou, F.; Houssiau, F.A. Management of Lupus Immune complexes (IC), produced in lymph nodes, spleen, or other lymphoid tissues Nephritis. J. Clin. Med. 2021, 10, 670. are deposited in the glomeruli of LN patients [4]. -

Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis
Diffuse Proliferative Glomerulonephritis and Acute Renal Failure Associated with Acute Staphylococcal Osteomyelitis MATTHEW D. GRIFFIN,* JOHANNES BJORNSSON,t and STEPHEN B. ERICKSON* *Department of Internal Medicine, Division of Nephrology, and tDepartment of Pathology, Mayo Clinic and Mayo Foundation, Rochester, Minnesota. Abstract. A 72-year-old man developed acute renal failure after peated surgical debridement. Spontaneous recovery of renal coronary bypass surgery that had been complicated by sternal function occurred after eradication of infection and final sur- osteomyelitis caused by the Staphylococcus aureus bacterium. gical wound repair. The relationship between acute bacterial Bacteremia and sepsis were not present. Renal biopsy demon- infections and glomerulonephritis and, in particular, the causal strated a florid, diffuse, proliferative glomerulonephritis with role of staphylococcal antigens in the pathogenesis of such glomerular immune complex deposition. Management in- lesions is discussed. (J Am Soc Nephrol 8: 1633-1639, 1997) cluded hemodialysis, prolonged antibiotic therapy, and re- Coagulase-positive staphylococcus (Staphylococcus aureus) is mg/dl]) and in the immediate postoperative period. Over the the most common causative organism in acute osteomyelitis following days, the patient’s serum creatinine concentration (1). Along with coagulase-negative staphylococcal species, it increased progressively, and hemodialysis was instituted on has also been implicated in the pathogenesis of immune com- day 23 after CABG. There was no past or family history of plex (IC)-mediated diffuse proliferative glomerulonephritis renal disease and no known drug allergies. Prior medical (DPGN) in a variety of infections. These include bacterial history had included degenerative disc disease, stable abdom- endocarditis, ventriculoatrial shunt infections, pneumonia, and inal aortic aneurysm, stable benign prostatic hyperplasia, and visceral abscesses with or without septicemia (2-6). -
Lupus Nephropathy
Rev. Colomb. Nefrol. 2014; 1(2): 101- 114. http//www.revistanefrologia.org Rev. Colomb.Review Nefrol. article2014; 1(2): 101-114 http//doi.org/10.22265/acnef.1.2.182 Lupus nephropathy Luis Fernando Pinto Peñaranda1 1Internal Medicine - Rheumatology, Medical Specialties - Research Unit, Hospital Pablo Tobón Uribe, Medellín – Colombia Abstract Lupus nephritis (LN) occurs between 30% and 70% of patients with systemic lupus erythematosus (SLE), depending on race and sex. LN appears early in the disease with prevalence of severe forms such as classes III, IV and mixed (V + III IV or V +). 50% of adults and 70% of children with lupus born in Colombia, suffer LN sometime in their lifetime; in this population 25% of children and 38% of adults have nephrotic syndrome. The remission rate at six months is low, the proteinuria in nephrotic range, and the incraease of baseline creatinine predict failure to achieve remission at 6 months. Key words: Lupus, Nephritis, Nephrotic Syndrome, Proliferative glomerulonephritis. Nefropatía lúpica Resumen La nefritis lúpica (NL) se presenta entre el 30 y 70% de los pacientes con lupus eritematoso sistémico (LES), dependiendo de la raza y el sexo, ocurre temprano en la enfermedad y predominan las formas gra- ves, clases III, IV y mixtas (V + III o V + IV). El 50% de los adultos y 70% de los niños colombianos con lupus sufren NL en algún momento de la vida; en esta población el 25% de los niños y el 38% de los adultos presentan síndrome nefrótico, la tasa de remisión a 6 meses es baja, la proteinuria en rango nefrótico y la elevación de creatinina basal, predicen falla en el logro de remisión a 6 meses. -

Pathogenesis of Human Systemic Lupus Erythematosus: a Cellular Perspective Vaishali R
Feature Review Pathogenesis of Human Systemic Lupus Erythematosus: A Cellular Perspective Vaishali R. Moulton,1,* Abel Suarez-Fueyo,1 Esra Meidan,1,2 Hao Li,1 Masayuki Mizui,3 and George C. Tsokos1,* Systemic lupus erythematosus (SLE) is a chronic autoimmune disease affecting Trends multiple organs. A complex interaction of genetics, environment, and hormones Recent work has identified patterns of leads to immune dysregulation and breakdown of tolerance to self-antigens, altered gene expression denoting resulting in autoantibody production, inflammation, and destruction of end- molecular pathways operating in organs. Emerging evidence on the role of these factors has increased our groups of SLE patients. knowledge of this complex disease, guiding therapeutic strategies and identi- Studies have identified local, organ- fying putative biomarkers. Recent findings include the characterization of specific factors enabling or ameliorat- ing SLE tissue damage, thereby dis- genetic/epigenetic factors linked to SLE, as well as cellular effectors. Novel sociating autoimmunity and end-organ observations have provided an improved understanding of the contribution of damage. tissue-specific factors and associated damage, T and B lymphocytes, as well Novel subsets of adaptive immune as innate immune cell subsets and their corresponding abnormalities. The effectors, and the contributions of intricate web of involved factors and pathways dictates the adoption of tailored innate immune cells including platelets therapeutic approaches to conquer this disease. and neutrophils, are being increasingly recognized in lupus pathogenesis. Studies have revealed metabolic cellu- SLE, a Devastating Disease for Young Women lar aberrations, which underwrite cell SLE afflicts mostly women [1] in which the autoimmune response is directed against practically and organ injury, as important contri- all organs, leading to protean clinical manifestations including arthritis, skin disease, blood cell butors to lupus disease. -

Glomerulonephritis Histopathological Pattern Change
AlYousef et al. BMC Nephrology (2020) 21:186 https://doi.org/10.1186/s12882-020-01836-3 RESEARCH ARTICLE Open Access Glomerulonephritis Histopathological Pattern Change Anas AlYousef1* , Ali AlSahow2, Bassam AlHelal3, Ahmed Alqallaf4, Emad Abdallah3, Mohammed Abdellatif1, Hani Nawar2 and Riham Elmahalawy4 Abstract Background: Glomerulonephritides (GN) are relatively rare kidney diseases with substantial morbidity and mortality. They are often difficult to treat, sometimes with no cure, and can lead to chronic kidney disease (CKD) and end stage kidney disease (ESKD). Kidney biopsy is the diagnostic procedure of choice with variable indications from center to center. It helps in identifying the exact specific diagnosis, assessing the level of disease activity and severity, and hence aids in proper therapy and helps predicting prognosis. There is a global change of pattern of glomerular disease over the last five decades. Methods: Retrospective analysis of all kidney biopsies (545 cases) that were done in patients over 12 year-old over last six years in four major hospitals in Kuwait. The indications for kidney biopsy were categorized into six clinical syndromes: nephrotic syndrome, sub-nephrotic proteinuria, nephrotic syndrome plus acute kidney injury (AKI), sub- nephrotic proteinuria plus AKI, isolated hematuria, and Unexplained renal impairment. We calculated the incidence of each type of kidney disease and indication of biopsy. Results: most common indication of kidney biopsy was sub-nephrotic proteinuria associated with AKI in 179 cases (32.8%). Primary Glomerulonephritis was the main diagnosis that was reported in 356 cases (65.3%). Immunoglobulin A Nephropathy (IgAN) was the commonest lesion in primary glomerulonephritis in 85 (23.9%) cases. -

Glomerulonephritis
Adolesc Med 16 (2005) 67–85 Glomerulonephritis Keith K. Lau, MDa,b, Robert J. Wyatt, MD, MSa,b,* aDivision of Pediatric Nephrology, Department of Pediatrics, University of Tennessee Health Sciences Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA bChildren’s Foundation Research Center at the Le Bonheur Children’s Medical Center, Room 301, WPT, 50 North Dunlap, Memphis, TN 38103, USA Early diagnosis of glomerulonephritis (GN) in the adolescent is important in initiating appropriate treatment and controlling chronic glomerular injury that may eventually lead to end-stage renal disease (ESRD). The spectrum of GN in adolescents is more similar to that seen in young and middle-aged adults than to that observed in prepubertal children. In this article, the authors discuss the clinical features associated with GN and the diagnostic evaluation required to determine the specific type of GN. With the exception of hereditary nephritis (Alport’s disease), virtually all types of GN are immunologically mediated with glomerular deposition of immunoglobulins and complement proteins. The inflammatory events leading to GN may be triggered by a number of factors. Most commonly, immune complexes deposit in the glomeruli or are formed in situ with the antigen as a structural component of the glomerulus. The immune complexes then initiate the production of proinflammatory mediators, such as complement proteins and cytokines. Subsequently, the processes of sclerosis within the glomeruli and fibrosis in the tubulointerstitial cells lead to chronic or even irreversible renal injury [1]. Less commonly, these processes occur without involvement of immune complexes—so-called ‘‘pauci-immune GN.’’ * Corresponding author. -

Iga Nephropathy in Systemic Lupus Erythematosus Patients
r e v b r a s r e u m a t o l . 2 0 1 6;5 6(3):270–273 REVISTA BRASILEIRA DE REUMATOLOGIA w ww.reumatologia.com.br Case report IgA nephropathy in systemic lupus erythematosus patients: case report and literature review Leonardo Sales da Silva, Bruna Laiza Fontes Almeida, Ana Karla Guedes de Melo, Danielle Christine Soares Egypto de Brito, Alessandra Sousa Braz, ∗ Eutília Andrade Medeiros Freire School of Medicine, Universidade Federal da Paraíba, João Pessoa, PB, Brazil a r t i c l e i n f o a b s t r a c t Article history: Systemic erythematosus lupus (SLE) is a multisystemic autoimmune disease which has Received 1 August 2014 nephritis as one of the most striking manifestations. Although it can coexist with other Accepted 19 October 2014 autoimmune diseases, and determine the predisposition to various infectious complica- Available online 16 February 2015 tions, SLE is rarely described in association with non-lupus nephropathies etiologies. We report the rare association of SLE and primary IgA nephropathy (IgAN), the most frequent Keywords: primary glomerulopathy in the world population. The patient was diagnosed with SLE due to the occurrence of malar rash, alopecia, pleural effusion, proteinuria, ANA 1: 1280, nuclear Systemic lupus erythematosus IgA nephropathy fine speckled pattern, and anticardiolipin IgM and 280 U/mL. Renal biopsy revealed mesan- Glomerulonephritis gial hypercellularity with isolated IgA deposits, consistent with primary IgAN. It was treated with antimalarial drug, prednisone and inhibitor of angiotensin converting enzyme, show- ing good progress. Since they are relatively common diseases, the coexistence of SLE and IgAN may in fact be an uncommon finding for unknown reasons or an underdiagnosed con- dition. -

Acute Poststreptococcal Glomerulonephritis: Immune Deposit Disease
Acute poststreptococcal glomerulonephritis: immune deposit disease. A F Michael Jr, … , R A Good, R L Vernier J Clin Invest. 1966;45(2):237-248. https://doi.org/10.1172/JCI105336. Research Article Find the latest version: https://jci.me/105336/pdf Journal of Clinical Investigation Vol. 45, No. 2, 1966 Acute Poststreptococcal Glomerulonephritis: Immune Deposit Disease * ALFRED F. MICHAEL, JR.,t KEITH N. DRUMMOND,t ROBERT A. GOOD,§ AND ROBERT L. VERNIER || WITH THE TECHNICAL ASSISTANCE OF AGNES M. OPSTAD AND JOYCE E. LOUNBERG (From the Pediatric Research Laboratories of the Variety Club Heart Hospital and the Department of Pediatrics, University of Minnesota, Minneapolis, Minn.) The possible role of immunologic mechanisms in the kidney in acute glomerulonephritis have also acute poststreptococcal glomerulonephritis was revealed the presence of discrete electron dense suggested in 1908 by Schick (2), who compared masses adjacent to the epithelial surface of the the delay in appearance of serum sickness after glomerular basement membrane (11-18). injection of heterologous serum to the latent pe- The purpose of this paper is to describe immuno- riod between scarlet fever and onset of acute glo- fluorescent and electron microscopic observations merulonephritis. Evidence in support of this con- of the kidney in 16 children with acute poststrepto- cept is the depression of serum complement during coccal glomerulonephritis. This study demon- the early stages of the disease (3) and glomerular strates 1) the presence of discrete deposits of yG- localization of immunoglobulin. Immunofluores- and fl3c-globulins along the glomerular basement cent studies have revealed either no glomerular membrane and its epithelial surface that are similar deposition of a-globulin (4) or a diffuse involve- in size and location to the dense masses seen by ment of the capillary wall (5-9). -
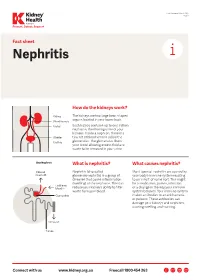
Nephritis Fact Sheet
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine.