Abdominal Wall CT Angiography: HOWIDOIT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
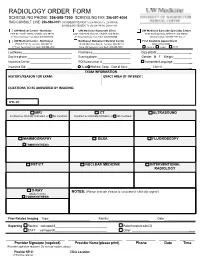
Radiology Order Form
RADIOLOGY ORDER FORM SCHEDULING PHONE: 206-598-7200 SCHEDULING FAX: 206-597-4004 RAD CONSULT LINE: 206-598-0101 UW RADIOLOGY RECORDS: Tel: 206-598-6206 Fax: 206-598-7690 NW RADIOLOGY RECORDS: Tel: 206-668-1748 Fax: 206-688-1398 UW Medical Center - Montlake UW Medicine Roosevelt Clinic UW Medicine Eastside Specialty Center 1959 NE Pacific Street, Seattle, WA 98195 4245 Roosevelt Way NE, Seattle, WA 98105 3100 Northup Way, Bellevue, WA 98004 2nd Floor Radiology Front Desk: 206-598-6200 2nd Floor Radiology Front Desk: 206-598-6868 ESC Front Desk: 425-646-7777 Opt. 2 UW Medical Center - Northwest Northwest Outpatient Medical Center First Available Appointment 1550 N 115th St, Seattle, WA 98133 10330 Meridian Ave N, Seattle, WA 98133 (ANY LOCATION) 2nd Floor Radiology Front Desk: 206-668-1302 Suite 130 Radiology Front Desk: 206-668-6050 Routine Urgent STAT Last Name: First Name: Date of Birth: _ Daytime phone: Evening phone: Gender: M F Weight:___________ Insurance Carrier: RQI/Authorization #: Interpreter/Language: __ Insurance ID#: Auto Workers’ Comp Date of Injury: ______ Claim # __ EXAM INFORMATION HISTORY/REASON FOR EXAM: EXACT AREA OF INTEREST: EXAM INFORMATION QUESTIONS TO BE ANSWERED BY IMAGING: ICD-10: MRI CT ULTRASOUND Contrast as clinically indicated, or No Contrast Contrast as clinically indicated, or No Contrast MAMMOGRAPHY DEXA FLUOROSCOPY TOMOSYNTHESIS PET/CT NUCLEAR MEDICINE INTERVENTIONAL RADIOLOGY X-RAY NOTES: (Please indicate if exam is considered “clinically urgent”) (Walk-In Only) TOMOSYNTHESIS Prior Related Imaging Type:_________________________ Facility:_________________________ Date:___________________ Reporting Routine call report # Patient to return with CD STAT call report # Other: __________ ________________________ ______________________ ____________ _______ ______ Provider Signature (required) Provider Name (please print) Phone Date Time (Provider signature required. -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Acr–Nasci–Sir–Spr Practice Parameter for the Performance and Interpretation of Body Computed Tomography Angiography (Cta)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2021 (Resolution 47)* ACR–NASCI–SIR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE AND INTERPRETATION OF BODY COMPUTED TOMOGRAPHY ANGIOGRAPHY (CTA) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Equilibrium Radionuclide Angiography/ Multigated Acquisition
EQUILIBRIUM RADIONUCLIDE ANGIOGRAPHY/ MULTIGATED ACQUISITION Equilibrium Radionuclide Angiography/ Multigated Acquisition S van Eeckhoudt, Bravis ziekenhuis, Roosendaal VJR Schelfhout, Rijnstate, Arnhem 1. Introduction Equilibrium radionuclide angiography (ERNA), also known as radionuclide ventriculography (ERNV), gated synchronized angiography (GSA), blood pool scintigraphy or multi gated acquisition (MUGA), is a well-validated technique to accurately determine cardiac function. In oncology its high reproducibility and low inter observer variability allow for surveillance of cardiac function in patients receiving potentially cardiotoxic anti-cancer treatment. In cardiology it is mostly used for diagnosis and prognosis of patients with heart failure and other heart diseases. 2. Methodology This guideline is based on available scientifi c literature on the subject, the previous guideline (Aanbevelingen Nucleaire Geneeskunde 2007), international guidelines from EANM and/or SNMMI if available and applicable to the Dutch situation. 3. Indications Several Class I (conditions for which there is evidence and/or general agreement that a given procedure or treatment is useful and effective) indications exist: • Evaluation of left ventricular function in cardiac disease: - Coronary artery disease - Valvular heart disease - Congenital heart disease - Congestive heart failure • Evaluation of left ventricular function in non-cardiac disease: - Monitoring potential cardiotoxic side effects of (chemo)therapy - Pre-operative risk stratifi cation in high risk surgery • Evaluation of right ventricular function: - Congenital heart disease - Mitral valve insuffi ciency - Heart-lung transplantation 4. Contraindications None 5. Medical information necessary for planning • Clear description of the indication (left and/or right ventricle) • Previous history of cardiac disease • Previous or current use of cardiotoxic medication PART I - 211 Deel I_C.indd 211 27-12-16 14:15 EQUILIBRIUM RADIONUCLIDE ANGIOGRAPHY/ MULTIGATED ACQUISITION 6. -

2019 Radiology Cpt Codes
2019 RADIOLOGY CPT CODES BONE DENSITOMETRY 1 Bone Density/DEXA 77080 CT 1 CT Abd & Pelvis W/ Contrast 74177 1 CT Enterography W/ Contrast 74177 1 CT Max/Facial W/O Contrast 70486 # CT Sinus Complete W/O Contrast 70486 1 CT Abd & Pelvis W W/O Contrast 74178 1 CT Extremity Lower W/ Contrast 73701 1 CT Neck W/ Contrast 70491 # CT Sinus Limited W/O Contrast 76380 1 CT Abd & Pelvis W/O Contrast 74176 1 CT Extremity Lower W/O Contrast 73700 1 CT Neck W/O Contrast 70490 # CT Spine Cervical W/ Contrast 72126 1 CT Abd W/ Contrast 74160 1 CT Extremity Upper W/ Contrast 73201 1 CT Orbit/ IAC W/ Contrast 70481 # CT Spine Cervical W/O Contrast 72125 1 CT Abd W/O Contrast 74150 1 CT Extremity Upper W/O Contrast 73200 1 CT Orbit/ IAC W/O Contrast 70480 # CT Spine Lumbar W/ Contrast 72132 1 CT Abd W W/O Contrast 74170 1 CT Head W/ Contrast 70460 1 CT Orbit/ IAC W W/O Contrast 70482 # CT Spine Lumbar W/O Contrast 72131 1 CT Chest W/ Contrast 71260 1 CT Head W/O Contrast 70450 1 CT Pelvis W/ Contrast 72193 # CT Spine Thoracic W/ Contrast 72129 1 CT Chest W/O Contrast 71250 1 CT Head W W/O Contrast 70470 1 CT Pelvis W/O Contrast 72192 # CT Spine Thoracic W/O Contrast 72128 1 CT Chest W W/O Contrast 71270 1 CT Max/Facial W/ Contrast 70487 1 CT Pelvis W W/O Contrast 72194 # CT Stone Protocol W/O Contrast 74176 CTA 1 Cardiac Calcium Score only 75571 1 CT Angiogram Abd & Pelvis W W/O Contrast 74174 1 CT Angiogram Head W W/O Contrast 70496 # CT / CTA Heart W Contrast 75574 1 CT Angiogram Abdomen W W/O Contrast 74175 1 CT Angiogram Chest W W/O Contrast 71275 -

Comparison of Echocardiography and Angiography in Determining the Cause of Severe Aortic Regurgitation
Br Heart J: first published as 10.1136/hrt.51.1.36 on 1 January 1984. Downloaded from Br Heart J 1984; 51: 36-45 Comparison of echocardiography and angiography in determining the cause of severe aortic regurgitation NICHOLAS L DEPACE, PASQUALE F NESTICO, MORRIS N KOTLER, GARY S MINTZ, DEMETRIOS KIMBIRIS, INDER P GOEL, E ELAINE GLAZIER-LASKEY, JOHN ROSS From the LikoffCardiovascular Institute, Hahnemann University, Philadelphia, Pennsylvania, USA SUMMARY To assess the accuracy of echocardiography in determining the cause of aortic regurgita- tion M mode and cross sectional echocardiography were compared with angiography in 43 patients with predominant aortic regurgitation. Each patient had all three investigations performed during the same admission to hospital. In each instance, the cause of aortic regurgitation was confirmed at surgery or necropsy. Seventeen patients had rheumatic aortic valve disease, 13 bacterial endocarditis with a perforated or partially destroyed cusp, five a biscuspid aortic valve (four with a history of endocarditis), and eight aortic regurgitation secondary to aortic root dilatation or aneurysm. Overall sensitivity of echocardiography and aortography was 84% in determining the cause of aortic regurgi- tation. Thus, rheumatic valve disease and endocarditis appear to be the most common causes of severe aortic regurgitation in this hospital based population. Furthermore, echocardiography is a sensitive non-invasive technique for determining the cause of aortic regurgitation and allows differentiation of valvular from root causes of aortic regurgitation. Aortic regurgitation may be caused by valvular dis- ment for predominant aortic regurgitation were http://heart.bmj.com/ ease, aortic root disease, or a combination of both. reviewed. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

X-Ray (Radiography) - Bone Bone X-Ray Uses a Very Small Dose of Ionizing Radiation to Produce Pictures of Any Bone in the Body
X-ray (Radiography) - Bone Bone x-ray uses a very small dose of ionizing radiation to produce pictures of any bone in the body. It is commonly used to diagnose fractured bones or joint dislocation. Bone x-rays are the fastest and easiest way for your doctor to view and assess bone fractures, injuries and joint abnormalities. This exam requires little to no special preparation. Tell your doctor and the technologist if there is any possibility you are pregnant. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. What is Bone X-ray (Radiography)? An x-ray exam helps doctors diagnose and treat medical conditions. It exposes you to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most often used form of medical imaging. A bone x-ray makes images of any bone in the body, including the hand, wrist, arm, elbow, shoulder, spine, pelvis, hip, thigh, knee, leg (shin), ankle or foot. What are some common uses of the procedure? A bone x-ray is used to: diagnose fractured bones or joint dislocation. demonstrate proper alignment and stabilization of bony fragments following treatment of a fracture. guide orthopedic surgery, such as spine repair/fusion, joint replacement and fracture reductions. look for injury, infection, arthritis, abnormal bone growths and bony changes seen in metabolic conditions. assist in the detection and diagnosis of bone cancer. locate foreign objects in soft tissues around or in bones. How should I prepare? Most bone x-rays require no special preparation. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -

The Costs and Benefits of Moving to the ICD-10 Code Sets
CHILDREN AND ADOLESCENTS This PDF document was made available from www.rand.org as a public CIVIL JUSTICE service of the RAND Corporation. EDUCATION ENERGY AND ENVIRONMENT Jump down to document HEALTH AND HEALTH CARE 6 INTERNATIONAL AFFAIRS POPULATION AND AGING The RAND Corporation is a nonprofit research PUBLIC SAFETY SCIENCE AND TECHNOLOGY organization providing objective analysis and effective SUBSTANCE ABUSE solutions that address the challenges facing the public TERRORISM AND HOMELAND SECURITY and private sectors around the world. TRANSPORTATION AND INFRASTRUCTURE U.S. NATIONAL SECURITY Support RAND Purchase this document Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore RAND Science and Technology View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. This product is part of the RAND Corporation technical report series. Reports may include research findings on a specific topic that is limited in scope; present discus- sions of the methodology employed in research; provide literature reviews, survey instruments, modeling exercises, guidelines for practitioners and research profes- sionals, and supporting documentation; -

Diagnostic Radiology Physics Diagnostic This Publication Provides a Comprehensive Review of Topics Relevant to Diagnostic Radiology Physics
A Handbook for Teachers and Students A Handbook for Teachers Diagnostic Diagnostic This publication provides a comprehensive review of topics relevant to diagnostic radiology physics. It is intended to provide the basis for the education of medical physicists in the field of diagnostic radiology. Bringing together the work of 41 authors and reviewers from 12 countries, the handbook covers a broad range of topics including radiation physics, dosimetry and Radiology instrumentation, image quality and image perception, imaging modality specific topics, recent advances in digital techniques, and radiation biology and protection. It is not designed to replace the large number of textbooks available on many aspects of diagnostic radiology physics, but is expected Radiology Physics Physics to fill a gap in the teaching material for medical radiation physics in imaging, providing in a single manageable volume the broadest coverage of topics currently available. The handbook has been endorsed by several international professional bodies and will be of value to those preparing for their certification A Handbook for as medical physicists, radiologists and diagnostic radiographers. Teachers and Students D.R. Dance S. Christofides A.D.A. Maidment I.D. McLean K.H. Ng Technical Editors International Atomic Energy Agency Vienna ISBN 978–92–0–131010–1 1 @ DIAGNOSTIC RADIOLOGY PHYSICS: A HANDBOOK FOR TEACHERS AND STUDENTS The following States are Members of the International Atomic Energy Agency: AFGHANISTAN GHANA OMAN ALBANIA GREECE PAKISTAN ALGERIA GUATEMALA -

Measurement of Peak Rates of Left Ventricular Wall Movement in Man Comparison of Echocardiography with Angiography
British HeartJournal, I975, 37, 677-683. Br Heart J: first published as 10.1136/hrt.37.7.677 on 1 July 1975. Downloaded from Measurement of peak rates of left ventricular wall movement in man Comparison of echocardiography with angiography D. G. Gibson and D. J. Brown From the Cardiac Department, Brompton Hospital, London, and the Medical Computer Centre, Westminster Hospital, London Estimates ofpeak systolic and diastolic rates of left ventricular wall movement were made in 23 patients by echocardiography and angiocardiography. Echocardiographic measurements were calculated as the rate of change of the transverse left ventricular dimension, derived continuously throughout the cardiac cycle. These were compared with similar plots of transverse left ventricular diameter, in the same patients, derived from digitized cineangiograms taken within IO minutes of echocardiograms. The results indicate close correlation between the two methods, and suggest that either can be used to measure peak rates of left ventricular wall movements in patients with heart disease. Identification of echoes arising from the interven- Echocardiograms tricular septum and posterior wall of the left In order to reduce the time interval between the two ventricle has proved to be a significant advance in investigations, echocardiograms were performed at the study of cardiac function by allowing the trans- cardiac catheterization using techniques that have pre- verse diameter of the left ventricle to be measured viously been described (Gibson, 1973). Clear, con- http://heart.bmj.com/ at end-systole and end-diastole (Chapelle and tinuous echoes were obtained from the posterior surface Mensch, I969; Feigenbaum et al., I969). More of the septum and the endocardium ofthe posterior wall recently, it has been possible to derive this dimension of the left ventricle, which were distinguished from those originating from the mitral valve apparatus.