Interventional Fluoroscopy Reducing Radiation Risks for Patients and Staff
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
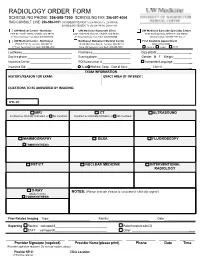
Radiology Order Form
RADIOLOGY ORDER FORM SCHEDULING PHONE: 206-598-7200 SCHEDULING FAX: 206-597-4004 RAD CONSULT LINE: 206-598-0101 UW RADIOLOGY RECORDS: Tel: 206-598-6206 Fax: 206-598-7690 NW RADIOLOGY RECORDS: Tel: 206-668-1748 Fax: 206-688-1398 UW Medical Center - Montlake UW Medicine Roosevelt Clinic UW Medicine Eastside Specialty Center 1959 NE Pacific Street, Seattle, WA 98195 4245 Roosevelt Way NE, Seattle, WA 98105 3100 Northup Way, Bellevue, WA 98004 2nd Floor Radiology Front Desk: 206-598-6200 2nd Floor Radiology Front Desk: 206-598-6868 ESC Front Desk: 425-646-7777 Opt. 2 UW Medical Center - Northwest Northwest Outpatient Medical Center First Available Appointment 1550 N 115th St, Seattle, WA 98133 10330 Meridian Ave N, Seattle, WA 98133 (ANY LOCATION) 2nd Floor Radiology Front Desk: 206-668-1302 Suite 130 Radiology Front Desk: 206-668-6050 Routine Urgent STAT Last Name: First Name: Date of Birth: _ Daytime phone: Evening phone: Gender: M F Weight:___________ Insurance Carrier: RQI/Authorization #: Interpreter/Language: __ Insurance ID#: Auto Workers’ Comp Date of Injury: ______ Claim # __ EXAM INFORMATION HISTORY/REASON FOR EXAM: EXACT AREA OF INTEREST: EXAM INFORMATION QUESTIONS TO BE ANSWERED BY IMAGING: ICD-10: MRI CT ULTRASOUND Contrast as clinically indicated, or No Contrast Contrast as clinically indicated, or No Contrast MAMMOGRAPHY DEXA FLUOROSCOPY TOMOSYNTHESIS PET/CT NUCLEAR MEDICINE INTERVENTIONAL RADIOLOGY X-RAY NOTES: (Please indicate if exam is considered “clinically urgent”) (Walk-In Only) TOMOSYNTHESIS Prior Related Imaging Type:_________________________ Facility:_________________________ Date:___________________ Reporting Routine call report # Patient to return with CD STAT call report # Other: __________ ________________________ ______________________ ____________ _______ ______ Provider Signature (required) Provider Name (please print) Phone Date Time (Provider signature required. -

THE FUTURE of INTERVENTIONAL RADIOLOGY Introduction
Volume 13 No 3 / Jun 2017 Quarterly publication of The Royal Australian and New Zealand College of Radiologists THE FUTURE OF INTERVENTIONAL RADIOLOGY Introduction A Day in the Life of a Modern Interventional Radiology Unit Interventional radiology (IR) has been It’s 7:30am on Wednesday morning and many of them with treatment histories a dynamic field since its inception the HCC meeting is about to start. The stretching back years. We have come over 50 years ago through the work room is filled with gastroenterologists, a a long way from an average life of early pioneers in the field. In hepatic surgeon, oncologists, diagnostic expectancy of seven months. 1964, Charles Dotter described and and interventional radiologists, IR By 8:30am, it’s time to get going on the performed the first angioplasty and and HCC nursing staff and keen first case of the day. He is a 54-year- in the years that followed, he and radiographers. It’s a relatively new old hypertensive vasculopath with other innovators brought about a meeting borne out of the UGI meeting calcified vessels and critical stenoses revolution in procedural medicine with that was at risk of stretching to several of his renal arteries. He was seen in the development of catheter directed hours by the prospect of an ever- the interventional clinic several weeks therapies and other minimally invasive increasing tide of chronic liver disease before for a pre-procedural assessment image guided techniques. (viral and NASH) predisposing to HCC. where he was fully worked up and Today, modern IR and the healthcare The first patient is a 65-year-old female paperwork completed so there are no system in which it operates is with cirrhosis, Child-Pugh A and ECOG hold ups getting him on the table. -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Acr–Nasci–Sir–Spr Practice Parameter for the Performance and Interpretation of Body Computed Tomography Angiography (Cta)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2021 (Resolution 47)* ACR–NASCI–SIR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE AND INTERPRETATION OF BODY COMPUTED TOMOGRAPHY ANGIOGRAPHY (CTA) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Interventional Radiology Curriculum for Medical Students
Interventional Radiology Curriculum for Medical Students Second Edition A brief overview of the most common clinical R conditions C SE handled by IRs May 2019 Editorial Board Editor in Chief Christoph Binkert Editors Roberto Cazzato Jan Jaap Janssen Gregory Makris Arash Najafi Fatemeh Sakhinia CIRSE Central Office Neutorgasse 9/6 1010 Vienna Austria Phone: +43 1 904 2003 Fax: +43 1 904 2003 30 E-mail: [email protected] www.cirse.org © All rights reserved by the Cardiovascular and Interventional Radiological Society of Europe / 2019 Table of Contents Introduction 2 1 Vascular IR 3 1.1 Peripheral Vascular Disease 3 1.2 Aneurysms 4 1.3 Venous Disease 5 1.3.1 Venous Thromboembolic Disease 5 1.3.2 Chronic Venous Obstruction 5 1.4 Embolisation for Benign Conditions 6 1.4.1 Uterine Fibroid Embolisation 6 1.4.2 Prostate Artery Embolisation 6 1.4.3 Gastrointestinal Bleeding 7 1.4.4 Gonadal Vein Embolisation 7 1.5 Access 8 1.5.1 Central Venous Access 8 1.5.2 Dialysis Shunt 8 2 Non-Vascular IR 9 2.1 Biopsies and Drainages 9 2.2 Biliary Procedures 9 2.3 Genitourinary Interventions 10 3 Interventional Oncology 11 3.1 Ablative Therapies 11 3.1.1 Liver Tumour Ablation 11 3.1.2 Renal Tumour Ablation 11 3.1.3 Lung Tumour Ablation 12 3.2 Liver Malignancy Embolisation 13 4 Musculoskeletal Interventions 14 4.1 Vertebral Compression Fractures and Vertebral Augmentation 14 4.2 Lower Back Pain 15 References 16 CIRSE and Interventional Radiology 18 Supporting IR’s Next Generation 19 Introduction In order to make medical students aware of the ever-increasing role of IR in hospital medicine and to provide guidance on the learning outcomes required to prepare medical students for their role during residency years, CIRSE published the first edition of the Interventional Radiology Curriculum for Medical Students in 2012. -

2019 Radiology Cpt Codes
2019 RADIOLOGY CPT CODES BONE DENSITOMETRY 1 Bone Density/DEXA 77080 CT 1 CT Abd & Pelvis W/ Contrast 74177 1 CT Enterography W/ Contrast 74177 1 CT Max/Facial W/O Contrast 70486 # CT Sinus Complete W/O Contrast 70486 1 CT Abd & Pelvis W W/O Contrast 74178 1 CT Extremity Lower W/ Contrast 73701 1 CT Neck W/ Contrast 70491 # CT Sinus Limited W/O Contrast 76380 1 CT Abd & Pelvis W/O Contrast 74176 1 CT Extremity Lower W/O Contrast 73700 1 CT Neck W/O Contrast 70490 # CT Spine Cervical W/ Contrast 72126 1 CT Abd W/ Contrast 74160 1 CT Extremity Upper W/ Contrast 73201 1 CT Orbit/ IAC W/ Contrast 70481 # CT Spine Cervical W/O Contrast 72125 1 CT Abd W/O Contrast 74150 1 CT Extremity Upper W/O Contrast 73200 1 CT Orbit/ IAC W/O Contrast 70480 # CT Spine Lumbar W/ Contrast 72132 1 CT Abd W W/O Contrast 74170 1 CT Head W/ Contrast 70460 1 CT Orbit/ IAC W W/O Contrast 70482 # CT Spine Lumbar W/O Contrast 72131 1 CT Chest W/ Contrast 71260 1 CT Head W/O Contrast 70450 1 CT Pelvis W/ Contrast 72193 # CT Spine Thoracic W/ Contrast 72129 1 CT Chest W/O Contrast 71250 1 CT Head W W/O Contrast 70470 1 CT Pelvis W/O Contrast 72192 # CT Spine Thoracic W/O Contrast 72128 1 CT Chest W W/O Contrast 71270 1 CT Max/Facial W/ Contrast 70487 1 CT Pelvis W W/O Contrast 72194 # CT Stone Protocol W/O Contrast 74176 CTA 1 Cardiac Calcium Score only 75571 1 CT Angiogram Abd & Pelvis W W/O Contrast 74174 1 CT Angiogram Head W W/O Contrast 70496 # CT / CTA Heart W Contrast 75574 1 CT Angiogram Abdomen W W/O Contrast 74175 1 CT Angiogram Chest W W/O Contrast 71275 -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Interventional Radiology in the Diagnosis and Treatment of Solid Tumors
THE ROLE OF INTERVENTIONAL RADIOLOGY IN THE DIAGNOSIS AND TREATMENT OF SOLID TUMORS Victoria L. Anderson, MSN, CRNP, FAANP OBJECTIVES •Using Case Studies and Imaging examples: 1) Discuss the role interventional (IR) procedures to aid in diagnosing malignancy 2) Current and emerging techniques employed in IR to cure and palliate solid tumor malignancies will be explored Within 1 and 2 will be a discussion of research in the field of IR Q+A NIH Center for Interventional Oncology WHAT IS INTERVENTIONAL RADIOLOGY? • Considered once a subspecialty of Diagnostic Radiology • Now its own discipline, it serves to offer minimally invasive procedures using state-of- the-art modern medical advances that often replace open surgery (Society of Interventional Radiology) NIH Center for Interventional Oncology CHARLES T. DOTTER M.D. (1920-1985) • Father of Interventional Radiologist • Pioneer in the Field of Minimally Invasive Procedures (Catheterization) • Developed Continuous X-Ray Angio- Cardiography • Performed First If a plumber can do it to pipes, we can do it to blood vessels.” Angioplasty (PTCA) Charles T. Dotter M.D. Procedure in 1964. • Treated the first THE ROOTS OF patient with catheter assisted vascular INTERVENTIONAL dilation RADIOLOGY NIH Center for Interventional Oncology THE “DO NOT FIX” CONSULT THE DO NOT FIX PATIENT SCALES MOUNT HOOD WITH DR. DOTTER 1965 NIH Center for Interventional Oncology •FIRST EMBOLIZATION FOR GI BLEEDING •ALLIANCE WITH •FIRST BALLOON BILL COOK •HIGH SPEED PERIPHERAL DEVELOPED RADIOGRAPHY ANGIOPLASTY-- NUMEROUS -

Fluoroscopy in Research Fact Sheet
Fluoroscopy in FactSheet Research luoroscopy is an imaging procedure that uses a continuous x-ray beam to create real-time images viewed on a monitor. It enables physicians to view internal organs and vessels in motion and can be used in both F diagnostic and therapeutic procedures. The long term risk associated with fluoroscopy is cancer, What I need to know... however, more immediate risks of skin injury due to high doses are possible. The typical fluoroscopic entrance Dose Reduction Techniques exposure rate for a medium-sized adult is approximately 30 mGy/min (3 rad/min), but is typically higher in image- • Use ultrasound imaging when possible. recording modes. Table 1 on the next page illustrates skin • Position the image intensifier as close to the injury per fluoroscopy dose and time of onset. patient as practicable. • Maximize the distance from the radiation For physicians/researchers, it is not often clear when the source. use of fluoroscopy is considered Standard of Care versus research. • Remove Grids. Grids improve the image quality, however, they increase the dose to the Standard of Care (SOC) is about clinical judgement, patient and staff by a factor of two or more. decision flexibility, whereas research needs to adhere • Use pulsed rather than continuous fluoroscopy strictly to protocols. The following assessments assist when possible, and with as low a pulse as the physician/researcher in determining whether use of possible. fluoroscopy is for research purposes: • Would the subject receive this care absent of the clinical trial? • Can you back yourself up in the literature? • Does local SOC differ from national standards/ guidelines? • Are protocol deviations documented? For any “NO” answer to the above, use of fluoroscopy may be for research purposes. -

Five-Year Results of a Merger Between Vascular Surgeons and Interventional Radiologists in a University Medical Center
From the Eastern Vascular Society Five-year results of a merger between vascular surgeons and interventional radiologists in a university medical center Richard M. Green, MD, and David Waldman, MD, PhD, for the Center for Vascular Disease* Rochester, NY Objectives: We examined economic and practice trends after 5 years of a merger between vascular surgeons and interventional radiologists. Methods: In 1998 a merger between the Division of Vascular Surgery and the Section of Interventional Radiology at the University of Rochester established the Center for Vascular Disease (CVD). Business activity was administered from the offices of the vascular surgeons. Results: In 1998 the CVD included five vascular surgeons and three interventional radiologists, who generated a total income of $5,789,311 (34% from vascular surgeons, 24% from interventional radiologists, 42% from vascular laborato- ries). Vascular surgeon participation in endoluminal therapy was limited to repair of abdominal aortic aneurysms (AAAs). Income was derived from 1011 major vascular procedures, 10,510 catheter-based procedures in 3286 patients, and 1 inpatient and 3 outpatient vascular laboratory tests. In 2002 there were six vascular surgeons (five, full-time equivalent) and four interventional radiologists, and total income was $6,550,463 despite significant reductions in unit value reimbursement over the 5 years, a 4% reduction in the number of major vascular procedures, and a 13% reduction in income from vascular laboratories. In 2002 the number of endoluminal procedures increased to 16,026 in 7131 patients, and contributions to CVD income increased from 24% in 1998 to 31% in 2002. Three of the six vascular surgeons performed endoluminal procedures in 634 patients in 2002, compared with none in 1998. -

X-Ray (Radiography) - Bone Bone X-Ray Uses a Very Small Dose of Ionizing Radiation to Produce Pictures of Any Bone in the Body
X-ray (Radiography) - Bone Bone x-ray uses a very small dose of ionizing radiation to produce pictures of any bone in the body. It is commonly used to diagnose fractured bones or joint dislocation. Bone x-rays are the fastest and easiest way for your doctor to view and assess bone fractures, injuries and joint abnormalities. This exam requires little to no special preparation. Tell your doctor and the technologist if there is any possibility you are pregnant. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. What is Bone X-ray (Radiography)? An x-ray exam helps doctors diagnose and treat medical conditions. It exposes you to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most often used form of medical imaging. A bone x-ray makes images of any bone in the body, including the hand, wrist, arm, elbow, shoulder, spine, pelvis, hip, thigh, knee, leg (shin), ankle or foot. What are some common uses of the procedure? A bone x-ray is used to: diagnose fractured bones or joint dislocation. demonstrate proper alignment and stabilization of bony fragments following treatment of a fracture. guide orthopedic surgery, such as spine repair/fusion, joint replacement and fracture reductions. look for injury, infection, arthritis, abnormal bone growths and bony changes seen in metabolic conditions. assist in the detection and diagnosis of bone cancer. locate foreign objects in soft tissues around or in bones. How should I prepare? Most bone x-rays require no special preparation. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions.