Australian Bat Lyssavirus (ABLV) Belongs to the Same Family As (But Is Antigenically Distinct To) the Rabies Virus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bat Calls of New South Wales
Bat calls of New South Wales Region based guide to the echolocation calls of microchiropteran bats Michael Pennay1 , Brad Law2 & Linda Reinhold3 1 New South Wales Department of Environment and Conservation 2 State Forests of New South Wales 3 Queensland Department of Natural Resources and Mines Bat calls of New South Wales Bat calls of New South Wales Published by the NSW Department of Environment and Conservation May 2004 Copyright © NSW Department of Environment and Conservation ISBN 0 7313 6786 3 This guide is the result of a co-operative project between NSW National Parks and Wildlife Service, now the NSW Department of Environment and Conservation (DEC) and State Forests of NSW (SFNSW). DEC provided project funding, management, staff, reference calls, preparation and printing. SFNSW provided part funding and granted support of staff time and expertise, reference calls and editing. Research was conducted under NPWS scientific licence number A2753 and SFNSW special purpose permit for research number 05466. Material presented in this publication may be copied for personal use or republished for non-commercial purposes provided that NSW Department of Environment and Conservation is fully acknowledged as the copyright owner. Apart from these purposes or for private study, research, criticism or review, as permitted under the Australian Copyright Act, no part of this publication may be reproduced by any process without written permission from NSW Department of Environment and Conservation. Inquiries should be addressed to the NSW Department of Environment and Conservation. This publication should be cited as follows: Pennay, M., Law, B., Reinhold, L. (2004). Bat calls of New South Wales: Region based guide to the echolocation calls of Microchiropteran bats. -

Bat Conservation 2021
Bat Conservation Global evidence for the effects of interventions 2021 Edition Anna Berthinussen, Olivia C. Richardson & John D. Altringham Conservation Evidence Series Synopses 2 © 2021 William J. Sutherland This document should be cited as: Berthinussen, A., Richardson O.C. and Altringham J.D. (2021) Bat Conservation: Global Evidence for the Effects of Interventions. Conservation Evidence Series Synopses. University of Cambridge, Cambridge, UK. Cover image: Leucistic lesser horseshoe bat Rhinolophus hipposideros hibernating in a former water mill, Wales, UK. Credit: Thomas Kitching Digital material and resources associated with this synopsis are available at https://www.conservationevidence.com/ 3 Contents Advisory Board.................................................................................... 11 About the authors ............................................................................... 12 Acknowledgements ............................................................................. 13 1. About this book ........................................................... 14 1.1 The Conservation Evidence project ................................................................................. 14 1.2 The purpose of Conservation Evidence synopses ............................................................ 14 1.3 Who this synopsis is for ................................................................................................... 15 1.4 Background ..................................................................................................................... -

Pacific Sheath-Tailed Bat American Samoa Emballonura Semicaudata Semicaudata Species Report April 2020
Pacific Sheath-tailed Bat American Samoa Emballonura semicaudata semicaudata Species Report April 2020 U.S. Fish and Wildlife Service Pacific Islands Fish and Wildlife Office Honolulu, HI Cover Photo Credits Shawn Thomas, Bat Conservation International. Suggested Citation USFWS. 2020. Species Status Assessment for the Pacific Sheath Tailed Bat (Emballonura semicaudata semicaudata). April 2020 (Version 1.1). U.S. Fish and Wildlife Service, Pacific Islands Fish and Wildlife Office, Honolulu, HI. 57 pp. Primary Authors Version 1.1 of this document was prepared by Mari Reeves, Fred Amidon, and James Kwon of the Pacific Islands Fish and Wildlife Office, Honolulu, Hawaii. Preparation and review was conducted by Gregory Koob, Megan Laut, and Stephen E. Miller of the Pacific Islands Fish and Wildlife Office. Acknowledgements We thank the following individuals for their contribution to this work: Marcos Gorresen, Adam Miles, Jorge Palmeirim, Dave Waldien, Dick Watling, and Gary Wiles. ii Executive Summary This Species Report uses the best available scientific and commercial information to assess the status of the semicaudata subspecies of the Pacific sheath-tailed bat, Emballonura semicaudata semicaudata. This subspecies is found in southern Polynesia, eastern Melanesia, and Micronesia. Three additional subspecies of E. semicaudata (E.s. rotensis, E.s. palauensis, and E.s. sulcata) are not discussed here unless they are used to support assumptions about E.s. semicaudata, or to fill in data gaps in this analysis. The Pacific sheath-tailed bat is an Old-World bat in the family Emballonuridae, and is found in parts of Polynesia, eastern Melanesia, and Micronesia. It is the only insectivorous bat recorded from much of this area. -

Insights Into Australian Bat Lyssavirus in Insectivorous Bats of Western Australia
Tropical Medicine and Infectious Disease Article Insights into Australian Bat Lyssavirus in Insectivorous Bats of Western Australia Diana Prada 1,*, Victoria Boyd 2, Michelle Baker 2, Bethany Jackson 1,† and Mark O’Dea 1,† 1 School of Veterinary Medicine, Murdoch University, Perth, WA 6150, Australia; [email protected] (B.J.); [email protected] (M.O.) 2 Australian Animal Health Laboratory, CSIRO, Geelong, VIC 3220, Australia; [email protected] (V.B.); [email protected] (M.B.) * Correspondence: [email protected]; Tel.: +61-893607418 † These authors contributed equally. Received: 21 February 2019; Accepted: 7 March 2019; Published: 11 March 2019 Abstract: Australian bat lyssavirus (ABLV) is a known causative agent of neurological disease in bats, humans and horses. It has been isolated from four species of pteropid bats and a single microbat species (Saccolaimus flaviventris). To date, ABLV surveillance has primarily been passive, with active surveillance concentrating on eastern and northern Australian bat populations. As a result, there is scant regional ABLV information for large areas of the country. To better inform the local public health risks associated with human-bat interactions, this study describes the lyssavirus prevalence in microbat communities in the South West Botanical Province of Western Australia. We used targeted real-time PCR assays to detect viral RNA shedding in 839 oral swabs representing 12 species of microbats, which were sampled over two consecutive summers spanning 2016–2018. Additionally, we tested 649 serum samples via Luminex® assay for reactivity to lyssavirus antigens. Active lyssavirus infection was not detected in any of the samples. -

2020 Taxonomic Update for Phylum Negarnaviricota (Riboviria: Orthornavirae), Including the Large Orders Bunyavirales and Mononegavirales
Archives of Virology https://doi.org/10.1007/s00705-020-04731-2 VIROLOGY DIVISION NEWS 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales Jens H. Kuhn1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Gaya K. Amarasinghe5 · Simon J. Anthony6,7 · Tatjana Avšič‑Županc8 · María A. Ayllón9,10 · Justin Bahl11 · Anne Balkema‑Buschmann12 · Matthew J. Ballinger13 · Tomáš Bartonička14 · Christopher Basler15 · Sina Bavari16 · Martin Beer17 · Dennis A. Bente18 · Éric Bergeron19 · Brian H. Bird20 · Carol Blair21 · Kim R. Blasdell22 · Steven B. Bradfute23 · Rachel Breyta24 · Thomas Briese25 · Paul A. Brown26 · Ursula J. Buchholz27 · Michael J. Buchmeier28 · Alexander Bukreyev18,29 · Felicity Burt30 · Nihal Buzkan31 · Charles H. Calisher32 · Mengji Cao33,34 · Inmaculada Casas35 · John Chamberlain36 · Kartik Chandran37 · Rémi N. Charrel38 · Biao Chen39 · Michela Chiumenti40 · Il‑Ryong Choi41 · J. Christopher S. Clegg42 · Ian Crozier43 · John V. da Graça44 · Elena Dal Bó45 · Alberto M. R. Dávila46 · Juan Carlos de la Torre47 · Xavier de Lamballerie38 · Rik L. de Swart48 · Patrick L. Di Bello49 · Nicholas Di Paola50 · Francesco Di Serio40 · Ralf G. Dietzgen51 · Michele Digiaro52 · Valerian V. Dolja53 · Olga Dolnik54 · Michael A. Drebot55 · Jan Felix Drexler56 · Ralf Dürrwald57 · Lucie Dufkova58 · William G. Dundon59 · W. Paul Duprex60 · John M. Dye50 · Andrew J. Easton61 · Hideki Ebihara62 · Toufc Elbeaino63 · Koray Ergünay64 · Jorlan Fernandes195 · Anthony R. Fooks65 · Pierre B. H. Formenty66 · Leonie F. Forth17 · Ron A. M. Fouchier48 · Juliana Freitas‑Astúa67 · Selma Gago‑Zachert68,69 · George Fú Gāo70 · María Laura García71 · Adolfo García‑Sastre72 · Aura R. Garrison50 · Aiah Gbakima73 · Tracey Goldstein74 · Jean‑Paul J. Gonzalez75,76 · Anthony Grifths77 · Martin H. Groschup12 · Stephan Günther78 · Alexandro Guterres195 · Roy A. -

Characterizing and Evaluating the Zoonotic Potential of Novel Viruses Discovered in Vampire Bats
viruses Article Characterizing and Evaluating the Zoonotic Potential of Novel Viruses Discovered in Vampire Bats Laura M. Bergner 1,2,* , Nardus Mollentze 1,2 , Richard J. Orton 2 , Carlos Tello 3,4, Alice Broos 2, Roman Biek 1 and Daniel G. Streicker 1,2 1 Institute of Biodiversity, Animal Health and Comparative Medicine, College of Medical, Veterinary and Life Sciences, University of Glasgow, Glasgow G12 8QQ, UK; [email protected] (N.M.); [email protected] (R.B.); [email protected] (D.G.S.) 2 MRC–University of Glasgow Centre for Virus Research, Glasgow G61 1QH, UK; [email protected] (R.J.O.); [email protected] (A.B.) 3 Association for the Conservation and Development of Natural Resources, Lima 15037, Peru; [email protected] 4 Yunkawasi, Lima 15049, Peru * Correspondence: [email protected] Abstract: The contemporary surge in metagenomic sequencing has transformed knowledge of viral diversity in wildlife. However, evaluating which newly discovered viruses pose sufficient risk of infecting humans to merit detailed laboratory characterization and surveillance remains largely speculative. Machine learning algorithms have been developed to address this imbalance by ranking the relative likelihood of human infection based on viral genome sequences, but are not yet routinely Citation: Bergner, L.M.; Mollentze, applied to viruses at the time of their discovery. Here, we characterized viral genomes detected N.; Orton, R.J.; Tello, C.; Broos, A.; through metagenomic sequencing of feces and saliva from common vampire bats (Desmodus rotundus) Biek, R.; Streicker, D.G. and used these data as a case study in evaluating zoonotic potential using molecular sequencing Characterizing and Evaluating the data. -

Is Bat Hair Morphology Exceptional?
Vespertilio 17: 171–183, 2014 ISSN 1213-6123 Is bat hair morphology exceptional? Britten D. SESSIONS1, Chanell E. Nielson2, John M. SOWA3, Wilford M. HESS4, Wesley “Skip” Skidmore5 & Bradley A. Carmack6 1 Patent Attorney, Zilka-Kotab, 1155 N. First Street Ste. 105, San Jose, CA 95112, U.S.A.; [email protected] 2 Department of English, Brigham Young University, Provo, UT 84602, U.S.A. 3 Department of Chemical Engineering, Brigham Young University, Provo, UT 84602, U.S.A. 4 Department of Plant and Wildlife Sciences, Brigham Young University, Provo, UT 84602, U.S.A. 5 Life Sciences Museum, Brigham Young University, Provo, UT 84602, U.S.A. 6 HR Professional, Sunnyvale, CA 94089, U.S.A. Abstract. Surface hair scale patterns from 19 bat species (families Vespertilionidae and Molossidae) from Utah were studied using scanning electron microscopy (SEM). Hair width, scale length, pattern, and position in relation to the long axis were used to characterize morphology within species, and fa- milies within the order Chiroptera. Previous studies indicate variations within families. Hair morphology results make it evident that large variations and similarities within the families can be seen visually and codified for the order. In the family Vespertilionidae, variations in hair morphology necessitated better terminology, including two new terms for morphology patterns. In the family Molossidae, distinctions between species, and possibly within the family, may be evident using SEM imaging to characterize morphology characteristics, although only two species were studied in this family. More precise morpho- logical measurements than used for this study may be necessary to construct useful keys for species within at least some families of bat. -

Viral Zoonotic Encephalitis: Australian Bat Lyssavirus and Hendra
Viral zoonotic encephalitis: Australian Bat Lyssavirus and Hendra Bev Paterson Hunter© by Medicalauthor Research Institute University of Newcastle Australia ESCMID OnlineEmail: [email protected] Library Encephalitis in Australia Causes substantial morbidity and mortality Herpes simplex virus is the most commonly identified causative pathogen 70% of adult encephalitis hospitalisations no pathogen identified 57% of deaths no pathogen identified (Reference: Huppatz et al. CDI,© 2009; by Huppatzauthor et al. EID, 2009) ESCMID Online Lecture Library Viral zoonotic encphalitis Several recently emerged or resurging pathogens are known to cause an encephalitis syndrome Vectorborne and transmitted flaviviruses – MVEV, WNEV-KUN and JEV © by author Bat-borne viruses – Australian Bat Lyssavirus (ABLV) and Hendra virus ESCMID Online Lecture Library Impact of climatic conditions © by author ESCMID Online Lecture Library Australian Bat Lyssavirus Australia has no endemic rabies ABLV is a member of the family Rhabdoviridae, genus Lyssavirus ABLV is very closely related to rabies (genotype 7 of the Lyssavirus genus) Reservoir is bats © by author Two deaths from ABLV ESCMID Online Lecture Library Human exposure © by author ESCMID Online Lecture Library Epidemiology of human disease Two fatal human cases – coastal Qld – encephalitis indistinguishable from classic rabies 1996 – 39yr female, a few weeks after scratches from bat 1998 – 37yr female, 27 months after bite from bat © by author References (Samaratunga -

BATS of the Golfo Dulce Region, Costa Rica
MURCIÉLAGOS de la región del Golfo Dulce, Puntarenas, Costa Rica BATS of the Golfo Dulce Region, Costa Rica 1 Elène Haave-Audet1,2, Gloriana Chaverri3,4, Doris Audet2, Manuel Sánchez1, Andrew Whitworth1 1Osa Conservation, 2University of Alberta, 3Universidad de Costa Rica, 4Smithsonian Tropical Research Institute Photos: Doris Audet (DA), Joxerra Aihartza (JA), Gloriana Chaverri (GC), Sébastien Puechmaille (SP), Manuel Sánchez (MS). Map: Hellen Solís, Universidad de Costa Rica © Elène Haave-Audet [[email protected]] and other authors. Thanks to: Osa Conservation and the Bobolink Foundation. [fieldguides.fieldmuseum.org] [1209] version 1 11/2019 The Golfo Dulce region is comprised of old and secondary growth seasonally wet tropical forest. This guide includes representative species from all families encountered in the lowlands (< 400 masl), where ca. 75 species possibly occur. Species checklist for the region was compiled based on bat captures by the authors and from: Lista y distribución de murciélagos de Costa Rica. Rodríguez & Wilson (1999); The mammals of Central America and Southeast Mexico. Reid (2012). Taxonomy according to Simmons (2005). La región del Golfo Dulce está compuesta de bosque estacionalmente húmedo primario y secundario. Esta guía incluye especies representativas de las familias presentes en las tierras bajas de la región (< de 400 m.s.n.m), donde se puede encontrar c. 75 especies. La lista de especies fue preparada con base en capturas de los autores y desde: Lista y distribución de murciélagos de Costa Rica. Rodríguez -

Morphometrics of the Family Emballonuridae
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DigitalCommons@University of Nebraska University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Papers in Natural Resources Natural Resources, School of September 1992 Morphometrics of the Family Emballonuridae Patricia W. Freeman University of Nebraska-Lincoln, [email protected] Cliff A. Lemen University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/natrespapers Part of the Natural Resources and Conservation Commons Freeman, Patricia W. and Lemen, Cliff A., "Morphometrics of the Family Emballonuridae" (1992). Papers in Natural Resources. 19. https://digitalcommons.unl.edu/natrespapers/19 This Article is brought to you for free and open access by the Natural Resources, School of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Papers in Natural Resources by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Published in Contributions to Mammalogy in honor of Karl F. Koopman (T.A. Griffiths and D. Klingener, Eds.), Bulletin of the American Museum of Natural History, No. 206, pp. 54–60. Copyright © 1992 American Museum of Natural History. Used by permission. American Museum of Natural History http://www.amnh.org/ Bulletin of the American Museum of Natural History http://library.amnh.org/pubs/bulletin.html R N\~)H, ISo. 206 : 5'4-*b lqq'L Morphometrics of the Family Emballonuridae PATRICIA W. FREEMAN1 AND CLIFF A. LEMEN2 ABSTRACT Morphometric analysis revealed three distinc- all other emballonurids. Phylogenetic studies also tive groups among the genera of emballonurids. separated Taphozous-Saccolaimus as distinctive Taphozous-Saccolaimus is a group distinctive in but included diclidurids among other New World size and shape, particularly cranially. -

Are Megabats Flying Primates? Contrary Evidence from a Mitochondrial DNA Sequence
Aust. J. Bioi. Sci., 1988, 41, 327-32 Are Megabats Flying Primates? Contrary Evidence from a Mitochondrial DNA Sequence S. Bennett,A L. J. Alexander,A R. H. CrozierB,c and A. G. MackinlayA,c A School of Biochemistry, University of New South Wales, P.O. Box 1, Kensington, N.S.W. 2033. B School of Biological Science, University of New South Wales, P.O. Box 1, Kensington, N.S.W. 2033. C To whom reprint requests should be addressed. Abstract Bats (Chiroptera) are divided into the suborders Megachiroptera (fruit bats, 'megabats') and Micro chiroptera (predominantly insectivores, 'microbats'). It had been found that megabats and primates share a connection system between the retina and the midbrain not seen in microbats or other eutherian mammals, and challenging but plausible hypotheses were made that (a) bats are diphyletic and (b) megabats are flying primates. We obtained two DNA sequences from the mitochondrion of the fruit bat Pteropus poliocephalus, and performed phylogenetic analyses using the bat sequences in conjunction with homologous Drosophila, mouse, cow and human sequences. Two trees stand out as significantly more likely than any other; neither of these links the bat and human as the closest sequences. These results cast considerable doubt on the hypothesis that megabats are particularly close to primates. Introduction Various phylogenetic schemes based on morphology have linked bats and primates, such as in McKenna's (1975) grandorder Archonta, which also includes the Dermoptera (flying lemurs) and Scandentia (tree shrews). Molecular systematists, using immunological comparisons and amino acid sequences, have found that bats are not placed particularly close to primates, and that they are not diphyletic (Cronin and Sarich 1980; Dene et al. -
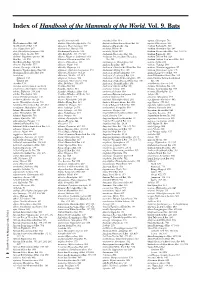
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A.