Types of Disinfectants Used in CDC LB Laboratories
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
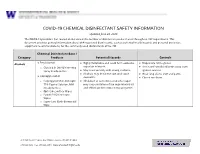
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -

European Contact Lens Society of Ophthalmologists ECLSO
European Contact Lens Society of Ophthalmologists ECLSO Course de Base en Contactologie I – IV Basiskurs in Kontaktologie I - IV Dr. med. Albert Franceschetti, Genève Michael Bärtschi, M.Sc.Optom. et M.Med.Educ.,Bern Optics and Contact Lenses What should I know about optics and physiological optics when I fit contact lenses ? Visual acuity = 1.0 • US notation 20/20 (20 feet) • Metric notation 6/6 (6 meters) • Decimal 10/10 (Monoyer) • Logarythmic Distance spectacles-eye • The position of the contact lens is different in relation to the eye. This is obviously the first criterion to take into consideration. • According to the power of the spectacles, the difference ǻ between the power of spectacle lenses and the contact lenses will be more or less important. Formula • DL power of the glasses (supposed perfect DL correction) DCL = -------------- 1 – d D • DCL power of the contact L lens (lens + tear meniscus) • d distance between the lens and the contact lens • ǻ difference between the power DCL and DL ǻ • ǻ = DCL –DL is always positive • ǻ = DCL –DL increases if the distance eye- glasses increases • The value d can be superior to 12mm if one uses trial lenses or refractor. Variation of powers between the two systems (contact lenses and spectacle) Distance eye- DL -20 -15 -10 -8 -5 +4 +10 glasses -16.13 -12.71 -8.93 -7.30 -4.72 +4.20 +11.36 DCL d=12m 3.87 2.29 1.07 0.70 0.28 0.20 1.36 m ǻ -15.38 -12.24 -8.70 -7.14 -4.65 +4.26 +11.76 DCL D=15 ǻ 4.62 2.76 1.30 0.86 0.35 0.26 1.76 mm Magnification • The distance eye-spectacles versus eye contact lens being different, the magnification of the retinal image will be different. -

(12) Patent Application Publication (10) Pub. No.: US 2014/0004156A1 Mellstedt Et Al
US 2014.0004156A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0004156A1 Mellstedt et al. (43) Pub. Date: Jan. 2, 2014 (54) BOLOGICAL INHIBITORS OF ROR1 Publication Classification CAPABLE OF INDUCING CELL, DEATH (51) Int. C. (76) Inventors: Hakan Mellstedt, Stockholm (SE): C07K 6/28 (2006.01) Hodjattallah Rabbani, Stockholm (SE); CI2N IS/II3 (2006.01) Ingrid Teige, Lund (SE) (52) U.S. C. CPC ............ C07K 16/28 (2013.01); CI2N 15/1138 (21) Appl. No.: 13/516,925 (2013.01) USPC ...... 424/400; 530/387.9; 536/24.5:536/23.1; (22) PCT Filed: Dec. 10, 2010 435/320.1; 435/325; 435/375; 424/139.1; (86). PCT No.: PCT/EP2010/007524 514/44. A:536/23.53; 435/331 S371 (c)(1), (57) ABSTRACT (2), (4) Date: Mar. 1, 2013 The invention relates to antibodies and siRNA molecules for (30) Foreign Application Priority Data inducing cell death by the specific binding of ROR1, domains thereof of nucleotide molecules encoding ROR1. There are Dec. 18, 2009 (GB) ................................... O922143.3 also provided methods involving and uses of the antibodies Jun. 3, 2010 (GB) ................................... 1OO93O7.8 and siRNA molecules of the invention. Patent Application Publication Jan. 2, 2014 Sheet 1 of 25 US 2014/0004156A1 L/S.*L/SdXL|-WLIXCRIO6] N Patent Application Publication Jan. 2, 2014 Sheet 2 of 25 US 2014/0004156A1 a bi-saw exit-8 ext: xx x: i. s: s x 8. : xxx xx . ex* x8. gri syst {{..} : twic s yxi-xxii. 33. 8 M. : : ised-east x 8. Patent Application Publication Jan. -

Hatchery Disinfection Policy and Procedures
MAINE DEPARTMENT OF INLAND FISHERIES & WILDLIFE Chapter 11 Disinfection Policy & Procedures Editors: David C. Rayner, Fish Culture Supervisor, Governor Hill State Fish Hatchery, Augusta, Maine (19XX- Present) & G. Russell Danner MS, DVM, Fish Pathologist, Fish Health Laboratory, Augusta, Maine (1998 – Present) Date: September 24, 1999. “Or if a person touches anything ceremonially unclean-whether the carcasses of unclean wild animals or of unclean livestock or of unclean creatures that move along the ground-even though he is unaware of it, he has become unclean and is guilty” Lev. 5:2 Several factors should be included in an evaluation of a disinfectant. A prerequisite for a disinfectant is its effectiveness against the expected spectrum of pathogens (Table 11- 1, 11-2, and 11-3). A general guideline for effective killing of pathogens by a disinfectant is a 5-log killing of bacteria and a 4-log killing of viruses. In addition to the activity of the disinfectant, its compatibility with devices should be reviewed in detail; this should include a review of data on devices that have been immersed for longer than recommended times. Instruments can be forgotten after immersion, and this mistake should not necessarily result in irreparable damage to the device. Other issues are toxicity, odor, compatibility with other compounds, and residual activity. Various and numerous organisms can cause diseases in fish. Viruses, bacteria, fungi, protozoan and many invertebrate animals are included in this list. No single disinfectant destroys them all. It is up to the applicant to decide what is the pathogen of most concern, and how it is to be reduced or eliminated. -

U.S. EPA, Pesticide Product Label, 776 DISINFECTANT VIRUCIDE
, 1-ls-lf9 UNITED ST ATES ENVIRONMENTAL PROTECTION AGENCY Carroll Company 2900 West Kingsley Road Garland, TX 75041 Subject: 776 Disinfectant, Virucide and Cleaner EPA Registration No. 4313-22 Amendment Dated November 9, 1998 Attn: Linda Kirk Kirby Director, Regulatory Compliance The amendment referred to above, submitted in connection with registration under the Federal Insecticide, Fungicide and Rodenticide Act, as amended, is acceptable. A stamped copy of the label is enclosed for your records. Submit one (I) copy ofthe finished printed label before this product is released for shipment. If you have any questions concerning the comments in this letter, you should contact Zenobia Jones at (703) 308-6198. Sincerely, ) JJ~lvJHdL Velma Noble Product Manager 31 Regulatory Management Branch I Antimicrobial Division (751 OW) COHCURRI!HCI!S ::::} ·m·I~ .Q........ ................ - ....................................... -................................ _............................. DATE ) . \-1i.-9l1... ....... ................... ................. .................................................................................... OFFICIAL FILE COpy Primed Oft R~cye/~d Paper ~' '....,-. " DISINFECTANT, UIRUCIDE* AND CLEANER FOR HOSPITAL INSTITUTIONAL ACTIVE INGREDIENT: AND iNDUSTRIAL USE Alkyl (C14 50%, C12 40%, C16 10%) dimelhyl • benzyl ammonium chloride........... 3.3 Yo ·Hum8n immunodeficiency virus, Type 1 (HIV-l) INERT INGR~DIENTS .................. 96.7% KEEP OUT OF REACH OF CHILDREN DANGER See back panel for additional precautionary -

Chemical Disinfectants | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC 3/19/20, 14:52
Chemical Disinfectants | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control | CDC 3/19/20, 14:52 Infection Control Chemical Disinfectants Guideline for Disinfection and Sterilization in Healthcare Facilities (2008) Alcohol Overview. In the healthcare setting, “alcohol” refers to two water-soluble chemical compounds—ethyl alcohol and isopropyl alcohol —that have generally underrated germicidal characteristics 482. FDA has not cleared any liquid chemical sterilant or high- level disinfectant with alcohol as the main active ingredient. These alcohols are rapidly bactericidal rather than bacteriostatic against vegetative forms of bacteria; they also are tuberculocidal, fungicidal, and virucidal but do not destroy bacterial spores. Their cidal activity drops sharply when diluted below 50% concentration, and the optimum bactericidal concentration is 60%–90% solutions in water (volume/volume) 483, 484. Mode of Action. The most feasible explanation for the antimicrobial action of alcohol is denaturation of proteins. This mechanism is supported by the observation that absolute ethyl alcohol, a dehydrating agent, is less bactericidal than mixtures of alcohol and water because proteins are denatured more quickly in the presence of water 484, 485. Protein denaturation also is consistent with observations that alcohol destroys the dehydrogenases of Escherichia coli 486, and that ethyl alcohol increases the lag phase of Enterobacter aerogenes 487 and that the lag phase e!ect could be reversed by adding certain amino acids. The bacteriostatic action was believed caused by inhibition of the production of metabolites essential for rapid cell division. Microbicidal Activity. Methyl alcohol (methanol) has the weakest bactericidal action of the alcohols and thus seldom is used in healthcare 488. The bactericidal activity of various concentrations of ethyl alcohol (ethanol) was examined against a variety of microorganisms in exposure periods ranging from 10 seconds to 1 hour 483. -

Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008
Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 William A. Rutala, Ph.D., M.P.H.1,2, David J. Weber, M.D., M.P.H.1,2, and the Healthcare Infection Control Practices Advisory Committee (HICPAC)3 1Hospital Epidemiology University of North Carolina Health Care System Chapel Hill, NC 27514 2Division of Infectious Diseases University of North Carolina School of Medicine Chapel Hill, NC 27599-7030 1 Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 3HICPAC Members Robert A. Weinstein, MD (Chair) Cook County Hospital Chicago, IL Jane D. Siegel, MD (Co-Chair) University of Texas Southwestern Medical Center Dallas, TX Michele L. Pearson, MD (Executive Secretary) Centers for Disease Control and Prevention Atlanta, GA Raymond Y.W. Chinn, MD Sharp Memorial Hospital San Diego, CA Alfred DeMaria, Jr, MD Massachusetts Department of Public Health Jamaica Plain, MA James T. Lee, MD, PhD University of Minnesota Minneapolis, MN William A. Rutala, PhD, MPH University of North Carolina Health Care System Chapel Hill, NC William E. Scheckler, MD University of Wisconsin Madison, WI Beth H. Stover, RN Kosair Children’s Hospital Louisville, KY Marjorie A. Underwood, RN, BSN CIC Mt. Diablo Medical Center Concord, CA This guideline discusses use of products by healthcare personnel in healthcare settings such as hospitals, ambulatory care and home care; the recommendations are not intended for consumer use of the products discussed. 2 -

Compatible Cleaning Solutions Chart*
Compatible Cleaning Solutions Chart* Reactive Chemicals Natural Rubber Polyurethane 316 Stainless Vinyl Nitrile FKM (Viton) Aluminum Neoprene Hypalon Silicone UHMW Hytrel Nitrile / SBR EPDM Nylon Brass XLPE Steel PTFE CPE Fluid PVC Notes: Alcohols +++++++–+–+– +++++ • Ingredient in Some (Methanol & Ethanol) Anti-Viral Cleansers Bleaching and Cleaning Bleach Solution + + • ••––– • + • – + • • – – – + – – Agent; Sodium (Sodium Hypochlorite) Hypochlorite Butyl Alcohol + + • + + + + + + + – + + + + + + + + + Potent virucidal agent Chlorine – – – – – – + + – – • • • Antiseptic; Anti-Viral – + + + + + ••– • + + • + + + + • + – – Insecticides and Citric Acid disinfectants; Antiviral Copper Chloride – + + + ••+++++++++++ +–– Copper Chloride Ethyl Alcohol + + + + + + + + • + • + + + + + + • + + + • + Ingredient in Some (Ethanol) Anti-Viral Cleansers Toilet, Tile and Porcelain Hydrochloric Acid +++–––––++–+++–––––– Cleaner; Anti-Viral (Polio) Hydrogen Peroxide + • – – – – – + • + – + • • – + • • ••–– Multipurpose Cleaner +++ –++–+––+ • ••–––– Antiseptic; Antiviral Iodine (Polio) + + + + ••+++–++++++++++++ Ingredient in Some Isopropyl Alcohol Anti-Viral Cleansers Phenol + • – – – – – – + – – + + + – – + + • + ••– Anti-Virus (Rhinovirus) (Carbolic Acid) (Adenovirus) Sodium Chloride ++++++++++++++++ • + – • Anti-Virus Sodium Hypochlorite ••+++––––++– • + + – – – ••–– Bleaching and Cleaning Agent (Bleach) Quaternary Ammonium + + + + + + + Common Anti-Viral; Salts (Lysol) Benzalkonium Chloride (Lysol) Lactic Acid – + • + – + + • + • • + + – + + + – -

US EPA, Pesticide Product Label, XHC-IA,06/07/2018
UNITED STATES ENVIRONMENTAL PROTECTION AGENCY WASHINGTON, DC 20460 OFFICE OF CHEMICAL SAFETY AND POLLUTION PREVENTION June 7, 2018 Bridget Middleton, M.S. Regulatory Specialist Ecolab Inc. 1 Ecolab Place St. Paul, MN 55102 Subject: PRIA Label Amendment – Adding Efficacy Claims and Emerging Viral Pathogens Language Product Name: XHC-IA EPA Registration Number: 1677-249 Application Date: January 16, 2018 Decision Number: 537595 Dear Ms. Middleton: The amended label referred to above, submitted in connection with registration under the Federal Insecticide, Fungicide and Rodenticide Act, as amended, is acceptable. This approval does not affect any conditions that were previously imposed on this registration. You continue to be subject to existing conditions on your registration and any deadlines connected with them. A stamped copy of your labeling is enclosed for your records. This labeling supersedes all previously accepted labeling. You must submit one copy of the final printed labeling before you release the product for shipment with the new labeling. In accordance with 40 CFR 152.130(c), you may distribute or sell this product under the previously approved labeling for 18 months from the date of this letter. After 18 months, you may only distribute or sell this product if it bears this new revised labeling or subsequently approved labeling. “To distribute or sell” is defined under FIFRA section 2(gg) and its implementing regulation at 40 CFR 152.3. Because you have opted to add statements pertaining to emerging viral pathogens to your label as described in the August 19, 2016, Guidance to Registrants: Process For Making Claims Against Emerging Viral Pathogens Not On EPA-Registered Disinfectant Labels (“Guidance”), https://www.epa.gov/sites/production/files/2016- 09/documents/emerging_viral_pathogen_program_guidance_final_8_19_16_001_0.pdf, you are subject to the following additional terms of registration: 1. -

FACT SHEET Chemical Disinfectants
FACT SHEET Chemical Disinfectants In the laboratory setting, chemical disinfection is the most common method employed to decontaminate surfaces and disinfect waste liquids. In most laboratories, dilutions of household bleach is the preferred method but there are many alternatives that may be considered and could be more appropriate for some agents or situations. There are numerous commercially available products that have been approved by the Environmental Protection Agency (EPA). EPA Registered Sterilizers, Tuberculocides, and Antimicrobial Products Against Certain Human Public Health Bacteria and Viruses can be found at https://www.epa.gov/pesticide- registration/selected-epa-registered-disinfectants Most EPA-registered disinfectants have a 10-minute label claim. However, OEHS Biosafety recommends a 15-20 minute contact time for disinfection/decontamination. General Considerations Prior to using a chemical disinfectant always consult the manufacturer’s instructions to determine the efficacy of the disinfectant against the biohazards in your lab and be sure to allow for sufficient contact time. In addition, consult the Safety Data Sheet for information regarding hazards, the appropriate protective equipment for handling the disinfectant and disposal of disinfected treated materials. Federal law requires all applicable label instructions on EPA-registered products to be followed (e.g., use-dilution, shelf life, storage, material compatibility, safe use, and disposal). Do not attempt to use a chemical disinfectant for a purpose it was not designed for. • When choosing a disinfectant consider the following: • The microorganisms present • The item to be disinfected or surface(s) • Corrosivity or hazards associated with the chemicals in the disinfectant • Ease of use 1. Organism Sensitivity and Resistant Organisms The innate characteristics of microorganisms often determine its sensitivity to chemical disinfection (Table 1). -

The Use of Povidone Iodine Nasal Spray and Mouthwash During the Current COVID-19 Pandemic May Protect Healthcare Workers and Reduce Cross Infection
March 27, 2020 The use of Povidone Iodine nasal spray and mouthwash during the current COVID-19 pandemic may protect healthcare workers and reduce cross infection. J Kirk-Bayley MRCP FRCA EDIC FFICM, Consultant Intensivist & Anaesthetist, Royal Surrey County Hospital S Challacombe, PhD, FRCPath, FDSRCS, FMedSci, DSc(h.c), FKC, Martin Rushton Professor of Oral Medicine, KCL VS Sunkaraneni LLM FRCS(2019), Consultant Rhinologist, Royal Surrey County Hospital J Combes FDS FRCS (OMFS), Lt Col RAMC, Consultant Advisor (ARMY) in OMFS, Defence Medical Services Abstract In late 2019 a novel coronavirus, SARS-CoV-2 causing Coronavirus disease 2019 (COVID-19) appeared in Wuhan China, and on 11th March 2020 the World Health Organisation declared it to have developed pandemic status. Povidone-iodine (PVP-I) has a better anti-viral activity than other antiseptics, and has already been proven to be an effective virucide in vitro against severe acute respiratory syndrome and Middle East respiratory syndrome coronaviruses (SARS-CoV and MERS- CoV). Povidone iodine has been shown to be a safe therapy when inhaled nasally or gargled. We propose that a protocolised nasal inhalation and oropharyngeal wash of PVP-I should be used in the current COVID-19 pandemic to limit the spread of SARS-CoV-2 from patients to healthcare workers (and vice versa) and thus reduce the incidence of COVID-19. There should be regular use in patients with COVID-19 to limit upper respiratory SARS-CoV-2 contamination, but also use by healthcare workers prior to treating COVID 19 patients or performing procedures in and around the mouth/ nose during the pandemic, regardless of the COVID 19 status of the patient.