FACT SHEET Chemical Disinfectants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chemical Disinfectants for Biohazardous Materials (3/21)
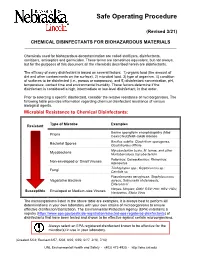
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -
EH&S COVID-19 Chemical Disinfectant Safety Information
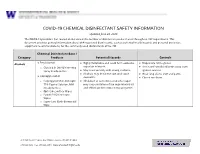
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -
For Peer Review Only - Page 1 of 27 BMJ Open
BMJ Open BMJ Open: first published as 10.1136/bmjopen-2015-010387 on 4 April 2016. Downloaded from FALSIFIED MEDICINES IN PERU: A Retrospective Review (1997-2014). ForJournal: peerBMJ Open review only Manuscript ID bmjopen-2015-010387 Article Type: Research Date Submitted by the Author: 27-Oct-2015 Complete List of Authors: Medina, Edwin; University of Barcelona - Faculty of Pharmacy, Department of Pharmacy and Pharmaceutical Technology Bel, Elvira; University of Barcelona - Faculty of Pharmacy, Department of Pharmacy and Pharmaceutical Technology Suñé, Josep María; University of Barcelona - Faculty of Pharmacy, Department of Pharmacy and Pharmaceutical Technology <b>Primary Subject Public health Heading</b>: Secondary Subject Heading: Global health, Epidemiology, Health policy, Health services research Keywords: Safety, Falsified, Medicines, Alerts, counterfeit, Drugs http://bmjopen.bmj.com/ on September 24, 2021 by guest. Protected copyright. For peer review only - http://bmjopen.bmj.com/site/about/guidelines.xhtml Page 1 of 27 BMJ Open BMJ Open: first published as 10.1136/bmjopen-2015-010387 on 4 April 2016. Downloaded from 1 2 3 FALSIFIED MEDICINES IN PERU: A Retrospective Review (1997-2014). 4 5 6 7 Authors: Edwin Medina1, Elvira Bel1, Josep María Suñé1 8 9 10 11 12 Affiliations: 13 14 15 1. DepartmentFor of peerPharmacy and review Pharmaceutical onlyTechnology, Faculty of 16 Pharmacy, University of Barcelona, Spain 17 18 19 20 Corresponding author: 21 22 Edwin Salvador Medina Vargas 23 24 Department of Pharmacy and Pharmaceutical Technology 25 Faculty of Pharmacy 26 University of Barcelona 27 Joan XXIII, s/n, 08028 Barcelona 28 29 Spain 30 Email: [email protected] 31 32 33 http://bmjopen.bmj.com/ 34 Keywords: Safety, Falsified, Medicines, Alerts, counterfeit, Drugs 35 36 37 38 39 Word Count 40 41 Abstract: 298 on September 24, 2021 by guest. -

Hydroxy- -Methylbutyrate (Hmb)
(19) *EP003373740B1* (11) EP 3 373 740 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A23K 10/10 (2016.01) A23L 33/10 (2016.01) 24.02.2021 Bulletin 2021/08 (86) International application number: (21) Application number: 16864978.8 PCT/US2016/061278 (22) Date of filing: 10.11.2016 (87) International publication number: WO 2017/083487 (18.05.2017 Gazette 2017/20) (54) COMPOSITIONS AND METHODS OF USE OF -HYDROXY- -METHYLBUTYRATE (HMB) AS AN ANIMAL FEED ADDITIVE ZUSAMMENSETZUNGEN UND VERFAHREN ZUR VERWENDUNG VON BETA-HYDROXY-BETA-METHYLBUTYRAT (HMB) ALS FUTTERZUSATZ COMPOSITIONS ET PROCÉDÉS D’UTILISATION DE -HYDROXY- -MÉTHYLBUTYRATE (HMB) COMME ADDITIF D’ALIMENT POUR ANIMAUX (84) Designated Contracting States: • BAIER, Shawn AL AT BE BG CH CY CZ DE DK EE ES FI FR GB Polk City, Iowa 50226 (US) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR (74) Representative: Evans, Jacqueline Gail Victoria Marches Intellectual Property Limited (30) Priority: 10.11.2015 US 201562253428 P Wyastone Business Park Wyastone Leys (43) Date of publication of application: Ganarew 19.09.2018 Bulletin 2018/38 Monmouth NP25 3SR (GB) (73) Proprietor: Metabolic Technologies, Inc. (56) References cited: Ames, IA 50010 (US) WO-A1-2004/037010 US-A- 5 028 440 US-A- 5 087 472 US-A- 5 087 472 (72) Inventors: US-A- 6 103 764 US-A1- 2014 249 223 • FULLER, John US-A1- 2015 025 145 Zearing, Iowa 50278 (US) • RATHMACHER, John Story City, Iowa 50248 (US) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -

Amoxicillin in Water: Insights Into Relative Reactivity, Byproduct Formation, and Toxicological Interactions During Chlorination
applied sciences Article Amoxicillin in Water: Insights into Relative Reactivity, Byproduct Formation, and Toxicological Interactions during Chlorination Antonietta Siciliano 1 , Marco Guida 1 , Giovanni Libralato 1 , Lorenzo Saviano 1, Giovanni Luongo 2 , Lucio Previtera 3, Giovanni Di Fabio 2 and Armando Zarrelli 2,* 1 Department of Biology, University of Naples Federico II, 80126 Naples, Italy; [email protected] (A.S.); [email protected] (M.G.); [email protected] (G.L.); [email protected] (L.S.) 2 Department of Chemical Sciences, University of Naples Federico II, 80126 Naples, Italy; [email protected] (G.L.); [email protected] (G.D.F.) 3 Associazione Italiana per la Promozione delle Ricerche su Ambiente e Salute umana, 82030 Dugenta, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-08-167-4472 Abstract: In recent years, many studies have highlighted the consistent finding of amoxicillin in waters destined for wastewater treatment plants, in addition to superficial waters of rivers and lakes in both Europe and North America. In this paper, the amoxicillin degradation pathway was investigated by simulating the chlorination process normally used in a wastewater treatment plant to reduce similar emerging pollutants at three different pH values. The structures of 16 isolated Citation: Siciliano, A.; Guida, M.; degradation byproducts (DPs), one of which was isolated for the first time, were separated on a Libralato, G.; Saviano, L.; Luongo, G.; C-18 column via a gradient HPLC method. Combining mass spectrometry and nuclear magnetic Previtera, L.; Di Fabio, G.; Zarrelli, A. resonance, we then compared commercial standards and justified a proposed formation mechanism Amoxicillin in Water: Insights into beginning from the parent drug. -

HIV-2 BLOT 1.2 Instructions for Use
HIV-2 BLOT 1.2 Instructions For Use FOR RESEARCH USE ONLY NOT FOR USE IN DIAGNOSTIC PROCEDURES REVISION DATE: 2017/05 Note Changes Highlighted MAC0012-ENG-1 (18 Tests): 11022-018 (36 Tests): 11022-036 NAME AND INTENDED USE The MP DIAGNOSTICS HIV-2 BLOT 1.2 is a qualitative enzyme immunoassay for in-vitro detection of specific antibodies to HIV-2 in human serum or plasma. This test kit is supplied for research purposes only. It is not intended for use in the diagnosis or prognosis of disease. In particular, this test cannot be used to evaluate blood specimens for the purposes of donor screening or as a confirmatory diagnostic. INTRODUCTION The MP Diagnostics HIV-2 BLOT 1.2 kit is intended as a supplemental antibody assay for Research Use Only. Human Immunodeficiency Virus Type 2 (HIV-2) infection was first described in 1985 in asymptomatic prostitutes from Senegal. The virus was subsequently isolated in 1986 from patients with AIDS-like symptoms in Guinea Bissau and Cape Verde. HIV-2 is related to, but distinct from HIV-1, the prototype AIDS virus. As such HIV-2 has many molecular, biological and serological similarities with HIV-1. Reports have shown that the infection is not limited to Africa and that HIV-2 seropositive individuals have been identified in Europe and the United States. DESCRIPTIONS OF SYMBOLS USED The following are graphical symbols used in or found on MP Diagnostics products and packaging. These symbols are the most common ones appearing on medical devices and their packaging. Some of the common symbols are explained in more detail in European Standard BS EN 980:2008 and International Standard ISO 15223-1:2007. -

Sodium Hypochlorite
SODIUM HYPOCHLORITE What is SODIUM HYPOCHLORITE? Sodium hypochlorite is a liquid with an odor of chlorine. Usually it is clear but some solutions are greenish to yellow in color. Other names for sodium hypochlorite include Clorox , bleach, liquid bleach, sodium oxychloride, Javex, antiformin, showchlon, Chlorox, B-K, Carrel-Dakin Solution, Chloros, Dakin’s Solution, hychlorite, Javelle Water, Mera Industries 2MOm≥B, Milton, modified Dakin’s Solution, Piochlor, and 13% active chlorine. Where can sodium hypochlorite be found and how is it used? Sodium hypochlorite is mainly used as a bleaching agent or disinfectant. A disinfectant kills bacteria that can carry diseases. It is found in consumer and commercial bleaches, cleaning solutions, and disinfectants for drinking water, wastewater and swimming pools. How can people be exposed to sodium hypochlorite? You could be exposed to sodium hypochlorite through: Breathing fumes while using products containing sodium hypochlorite. Drinking water from public drinking water supplies where these chemicals were added to kill bacteria. You could also be exposed by drinking sodium hypochlorite by accident. Touching sodium hypochlorite if gloves are not worn when using products containing it. Eye Contact by splashing sodium hypochlorite during use. People who work where sodium hypochlorite is used to bleach paper and textiles may have slightly higher levels of exposure in all of the above areas. How does sodium hypochlorite work and how can it affect my health? Sodium hypochlorite is a corrosive substance, meaning that it will eat away at materials it contacts. Accidental sodium hypochlorite poisoning can be deadly. Severe injuries can occur to the mouth, throat, esophagus and stomach. -

(12) Patent Application Publication (10) Pub. No.: US 2014/0004156A1 Mellstedt Et Al
US 2014.0004156A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0004156A1 Mellstedt et al. (43) Pub. Date: Jan. 2, 2014 (54) BOLOGICAL INHIBITORS OF ROR1 Publication Classification CAPABLE OF INDUCING CELL, DEATH (51) Int. C. (76) Inventors: Hakan Mellstedt, Stockholm (SE): C07K 6/28 (2006.01) Hodjattallah Rabbani, Stockholm (SE); CI2N IS/II3 (2006.01) Ingrid Teige, Lund (SE) (52) U.S. C. CPC ............ C07K 16/28 (2013.01); CI2N 15/1138 (21) Appl. No.: 13/516,925 (2013.01) USPC ...... 424/400; 530/387.9; 536/24.5:536/23.1; (22) PCT Filed: Dec. 10, 2010 435/320.1; 435/325; 435/375; 424/139.1; (86). PCT No.: PCT/EP2010/007524 514/44. A:536/23.53; 435/331 S371 (c)(1), (57) ABSTRACT (2), (4) Date: Mar. 1, 2013 The invention relates to antibodies and siRNA molecules for (30) Foreign Application Priority Data inducing cell death by the specific binding of ROR1, domains thereof of nucleotide molecules encoding ROR1. There are Dec. 18, 2009 (GB) ................................... O922143.3 also provided methods involving and uses of the antibodies Jun. 3, 2010 (GB) ................................... 1OO93O7.8 and siRNA molecules of the invention. Patent Application Publication Jan. 2, 2014 Sheet 1 of 25 US 2014/0004156A1 L/S.*L/SdXL|-WLIXCRIO6] N Patent Application Publication Jan. 2, 2014 Sheet 2 of 25 US 2014/0004156A1 a bi-saw exit-8 ext: xx x: i. s: s x 8. : xxx xx . ex* x8. gri syst {{..} : twic s yxi-xxii. 33. 8 M. : : ised-east x 8. Patent Application Publication Jan. -

Kinetic Studies on Oxidative Dissolution of Elemental Mercury in Aqueous Sodium Hypochlorite
International Journal of Environmental Science and Development, Vol. 7, No. 7, July 2016 Kinetic Studies on Oxidative Dissolution of Elemental Mercury in Aqueous Sodium Hypochlorite S. Bandyopadhyay, S. Chakraborty, D. B. Zaini, and S. Bhattacharjee mercury and second order reaction kinetics was observed Abstract—Aqueous sodium hypochlorite is often used to between elemental mercury and free chlorine. detoxify solid wastes containing elemental mercury and its Solid wastes are often treated with aqueous sodium compounds by oxidative dissolution of mercury in the form of a hypochlorite to remove mercury and its compounds. Brine soluble mercurochloro complex. Experiments were conducted to estimate global kinetics and interfacial mass transfer mud of a chlor-alkali industry containing elemental mercury parameters of the reaction between elemental mercury and and its salts is a solid waste and is usually dumped off-site in a aqueous sodium hypochlorite. The reaction did not conform to lined pond. Sometimes this brine mud is treated with aqueous either pure mass transfer or pure instantaneous reaction sodium hypochlorite to remove toxic mercury from the sludge. regimes. The order and activation energy of the reaction were This is a solid-liquid reaction and involves mass transfer of -1 estimated to be 1.168 and 13.48 kJ mol respectively. mercury from the solid matrix into a liquid phase. Sizeneva et Experimental data on reaction enhancement factors may be used al. [10] studied oxidative dissolution of Hg0 in NaOCl at pH for design of an industrial solid waste detoxification reactor. 0 0 5.9, 6.5, 6.9 and 8.5 at 25 C and 50 C. -

COVID-19 Environmental Cleaning and Disinfectants for Clinic
Coronavirus COVID-19 BC Centre for Disease Control | BC Ministry of Health Environmental Cleaning and Disinfectants for Health-Care and Clinic Settings Cleaning: the physical removal of visible soiling (e.g., dust, soil, blood, mucus). Cleaning removes, rather than kills, viruses and bacteria. It is done with water, detergents, and steady friction from cleaning cloth. Disinfection: the killing of viruses and bacteria. A disinfectant is only applied to objects; never on the human body. All visibly soiled surfaces should be cleaned before disinfection. Environmental cleaning for the COVID-19 virus is the same as for other common viruses. Cleaning products and disinfectants that are regularly used in hospitals and health-care settings are strong enough to deactivate coronaviruses and prevent their spread. Cleaning of visibly soiled surfaces followed by disinfection is recommended for the prevention of COVID-19 and other viral respiratory illnesses. Suggested cleaning and disinfecting frequencies for health-care and clinic settings: Type of surface Frequency 1. Shared equipment IN BETWEEN PATIENTS otoscopes, baby scales, tables and exam beds 2. Frequently-touched surfaces Examples: medical equipment, door knobs, light AT LEAST TWICE A DAY switches, telephones, keyboards, mice, pens, charts, cell phones, toys, bathrooms 3. General cleaning of procedure / exam rooms AT LEAST ONCE A DAY For electronic equipment please comply with manufacturer’s instructions in order to meet warranty requirements 06.02.21 Coronavirus COVID-19 BC Centre for Disease Control | BC Ministry of Health Environmental Cleaning and Disinfectants for Health-Care and Clinic Settings The list of common disinfectants below is provided as a guide to choosing products. -

Disinfection of Tonometers a Report by the American Academy of Ophthalmology
Ophthalmic Technology Assessment Disinfection of Tonometers A Report by the American Academy of Ophthalmology Anna K. Junk, MD,1 Philip P. Chen, MD,2 Shan C. Lin, MD,3 Kouros Nouri-Mahdavi, MD,4 Sunita Radhakrishnan, MD,5 Kuldev Singh, MD, MPH,6 Teresa C. Chen, MD7 Objective: To examine the efficacy of various disinfection methods for reusable tonometer prisms in eye care and to highlight how disinfectants can damage tonometer tips and cause subsequent patient harm. Methods: Literature searches were conducted last in October 2016 in the PubMed and the Cochrane Library databases for original research investigations. Reviews, non-English language articles, nonophthalmology articles, surveys, and case reports were excluded. Results: The searches initially yielded 64 unique citations. After exclusion criteria were applied, 10 labo- ratory studies remained for this review. Nine of the 10 studies used tonometer prisms and 1 used steel discs. The infectious agents covered in this assessment include adenovirus 8 and 19, herpes simplex virus (HSV) 1 and 2, human immunodeficiency virus 1, hepatitis C virus, enterovirus 70, and variant Creutzfeldt-Jakob disease. All 4 studies of adenovirus 8 concluded that after sodium hypochlorite (dilute bleach) disinfection, the virus was undetectable, but only 2 of the 4 studies found that 70% isopropyl alcohol (e.g., alcohol wipes or soaks) eradicated all viable virus. All 3 HSV studies concluded that both sodium hypochlorite and 70% isopropyl alcohol eliminated HSV. Ethanol, 70% isopropyl alcohol, dilute bleach, and mechanical cleaning all lack the ability to remove cellular debris completely, which is necessary to prevent prion transmission. Therefore, single-use tonometer tips or disposable tonometer covers should be considered when treating patients with suspected prion disease.