Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
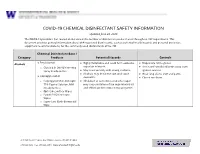
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

National Center for Toxicological Research
National Center for Toxicological Research Annual Report Research Accomplishments and Plans FY 2015 – FY 2016 Page 0 of 193 Table of Contents Preface – William Slikker, Jr., Ph.D. ................................................................................... 3 NCTR Vision ......................................................................................................................... 7 NCTR Mission ...................................................................................................................... 7 NCTR Strategic Plan ............................................................................................................ 7 NCTR Organizational Structure .......................................................................................... 8 NCTR Location and Facilities .............................................................................................. 9 NCTR Advances Research Through Outreach and Collaboration ................................... 10 NCTR Global Outreach and Training Activities ............................................................... 12 Global Summit on Regulatory Science .................................................................................................12 Training Activities .................................................................................................................................14 NCTR Scientists – Leaders in the Research Community .................................................. 15 Science Advisory Board ................................................................................................... -

Use of 90% Ethanol to Decontaminate Stethoscopes in Resource Limited
Raghubanshi et al. Antimicrobial Resistance and Infection Control (2017) 6:68 DOI 10.1186/s13756-017-0224-x RESEARCH Open Access Use of 90% ethanol to decontaminate stethoscopes in resource limited settings Bijendra Raj Raghubanshi, Supriya Sapkota, Arjab Adhikari*, Aman Dutta, Utsuk Bhattarai and Rastriyata Bhandari Abstract Background: In developing countries like Nepal, 90% ethanol is cheap and is available in most hospitals. The unavailability of isopropyl alcohol (IPA) in these settings led us to compare the efficacy between 90% ethanol and isopropyl alcohol pads in reducing the bacterial contamination of diaphragm of stethoscope. Methods: A randomized blinded experimental study was carried out to determine the difference between cleaning stethoscopes with 90% ethanol and IPA. Cultures of diaphragm were taken before and after cleaning with one of the cleaning agent. Colony forming units (CFU) count and organism identification was done by a blinded investigator. CFU before and after cleaning were compared using Wilcoxon signed–rank test. Mann Whitney U test was used to compare the decrease in CFU count between the cleaning agents. Results: About 30% of the stethoscopes harbored potential pathogens. Significant reduction in CFU was observed with both IPA (Wilcoxon signed–rank test, P value <0.001) and 90% ethanol (Wilcoxon signed–rank test, P value <0. 001). Comparing median decrease in CFU between cleaning with IPA and with 90% ethanol, no significant difference was found (Mann Whitney U test; U = 1357, P value >0.05). Conclusions: Both 90% ethanol and IPA are equally effective in decontaminating the diaphragm of stethoscope. Selection of agent should be done on the basis of cost and availability. -
Theory of Operation: How Parts Cleaning Works
Theory of Operation: How Parts Cleaning Works MART defines the term to clean as to overpower the soils. The MART Parts Washer is a high-impact pressure, high-temperature, industrial water-based cleaning system that uses a combination of the following factors to achieve cleaning results: Power x Temperature x Chemical x Time = Clean The relationship of these variables can be varied in an infinite number of ways to achieve the same level of cleanliness. Your own needs determine the relative value of each variable. Keep in mind that the MART Parts Washer provides one of the highest blasting powers in the cleaning industry, allowing you to reduce the wash-cycle times for your parts to a minimum. Additionally, the high blasting power allows you to operate the washer at lower cleaning temperatures, thus saving energy, and using less chemical than spray washers The exact combination of the factors must be determined for your application, based on the types of soils to be removed, the degree of cleanliness required, the cycle time required, the types of parts to be cleaned, and so on. How the Parts Washer Works The parts washer operates on a timed cycle. The operator places the parts to be cleaned in the washer on the turntable, closes and latches the door, and then starts the timed cleaning cycle. During the cleaning cycle, a high-temperature, high-pressure, water-and-detergent cleaning solution blasts soils from the parts. After the cycle has stopped and the steam has exhausted, the operator removes the cleaned parts. The parts washer utilizes closed loop, waste minimization technology, continuously reusing its cleaning solution and effectively reducing pollution potential. -

Toxicological Profile for Formaldehyde
TOXICOLOGICAL PROFILE FOR FORMALDEHYDE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Agency for Toxic Substances and Disease Registry July 1999 FORMALDEHYDE ii DISCLAIMER The use of company or product name(s) is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry. FORMALDEHYDE iii UPDATE STATEMENT Toxicological profiles are revised and republished as necessary, but no less than once every three years. For information regarding the update status of previously released profiles, contact ATSDR at: Agency for Toxic Substances and Disease Registry Division of Toxicology/Toxicology Information Branch 1600 Clifton Road NE, E-29 Atlanta, Georgia 30333 FORMALDEHYDE vii QUICK REFERENCE FOR HEALTH CARE PROVIDERS Toxicological Profiles are a unique compilation of toxicological information on a given hazardous substance. Each profile reflects a comprehensive and extensive evaluation, summary, and interpretation of available toxicologic and epidemiologic information on a substance. Health care providers treating patients potentially exposed to hazardous substances will find the following information helpful for fast answers to often-asked questions. Primary Chapters/Sections of Interest Chapter 1: Public Health Statement: The Public Health Statement can be a useful tool for educating patients about possible exposure to a hazardous substance. It explains a substance’s relevant toxicologic properties in a nontechnical, question-and-answer format, and it includes a review of the general health effects observed following exposure. Chapter 2: Health Effects: Specific health effects of a given hazardous compound are reported by route of exposure, by type of health effect (death, systemic, immunologic, reproductive), and by length of exposure (acute, intermediate, and chronic). -

U.S. EPA, Pesticide Product Label, WHITE CAP 15% PINE OIL
UNITED STATES ENVIRONMENTAL PROTECTION AGENCY /0 -c:JJ - cXJ{X).. EPA Reg. Date of Issuance: U.S . ENVIRONMENTAL PRCTECTION AGENCY Number: .,-«0 $7'.-, Office of ?esticide Programs ~. ~ ~ Antimicrob:a:s Division (7510C] 72138-E 1200 Penns:(:.vania Avenue N.W. OCT 2 1 201a {$1V:Z ~ Washir:g:on, D.C. 20460 <>.,J Term of IS~..lance: NOTICE OF PESTICIDE: Conditional _x_ Registration Reregistration --- Name of Pe~:icide Product: White (under fH'RA, as amended) Cap 15% Pine Oil Cleaner/Disinfectant Name and Address of Registrant (inc! ude lIP Code): White Cap, Inc. 625 Governor Printz Blvd. lC""'i.ngton, PA 19029 .0": Changes. in 1~1~ e~~t . :li1 silbstance from that accepted in connection witlt this registration must be _.-tted t:l'I!ondacd . -,,-~~~~~~_J..strat10n 01vbion prior to use of the label ia c01MIerce. In any correspondeQoe " : _ _ rater -to. the above EPA registration number. On the basis of information furnished by the registrant, the above named pesticide is hereby registered/reregistered under the Federal Insecticide, Fungicide and Rodenticide Act. Registration is in no way to be construed as an endorsement or recommendation of this product by the Agency. In order to protect health and the environment, the Administrator, on his motion, may at any time suspend or cancel the registration of a pesticide in accordance with the Act. The acceptance of any name in connection with the registration of a product under this Act is not to be construed as giving the registrant a right to exclusive use of the name or to its use if it has been covered by others. -

Chemical Disinfectant and Cleaning Agent Safety – Frequently Asked Questions
Caribbean Public Health Agency Technical Guidance: COVID-19 Series No 33 Chemical Disinfectant and Cleaning Agent Safety – Frequently Asked Questions Suggested Citation: CARPHA. (2020). Chemical disinfectant and cleaning agent safety – frequently asked questions. Caribbean Public Health Agency Technical Guidance: COVID-19 Series, no. 33. CARPHA 2020 Chemical Disinfectant and Cleaning Agent Safety – Frequently Asked Questions 9 July 2020 Why are we concerned about cleaning agents and disinfectants? Selecting the correct chemical agent for cleaning and disinfecting and safely handling and using that agent is essential to health and wellbeing. Recently, with the increased focus on cleaning to reduce the risk of exposure to coronavirus disease, there have been an associated increase in media stories warning the public of the dangerous chemicals used for disinfectants. All chemical cleaning agents can be harmful to the health of the person using the product if it is not used as directed on the label by the manufacturer. Chemical agents can cause burns, breathing difficulties or damage to the lungs, or possibly result in poisoning. Persons should carefully read instructions for use, safety data sheets, and any health warnings to ensure they have selected the correct chemical agents, have the appropriate personal protection, and use and store the chemicals in a safe way. What are the properties of effective chemical cleaning agents and disinfectants? A wide variety of chemical agents can be used for cleaning, sanitising, and disinfecting. There are 4 categories of cleaners: detergents, degreasers, abrasives, and acids. Each is effective for cleaning different surfaces depending on the type of soiling. Different chemical agents are effective for killing different bacteria and viruses.1 Molds and fungus will require a sporicidal agent2. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -
Laboratory Reagents Product List 2021
PRODUCT LIST Examples of our laboratory reagents Product list – selected products Artificial Urine Brooks and Keevil AMPQ44861.1000 Auramine-Rhodamine AMPQ55029.0500 Below is a selection of products. If you cannot find what you are look- Auric Chloride 0.1% AMPQ12450.0500 ing for, please contact us about your specific requests for laboratory reagents, volume and packaging, etc. Auric Chloride 1% AMPQ12452.0100 We mainly use chemicals by p.a. quality. If you want growth control on growing media, please contact us for an offer. B Balanced Salt Solution for Storage AMPQ46214.0100 Product name Cat. No. Balanced Salt Solution with Tris AMPQ40040.1000 Barium Chloride 0.5 M = 1.0 N AMPQ42099.1000 2,4-Dinitroflouro Benzen 1.3% v/v AMPQ44913.0100 Barium Chloride 1 M AMPQ43551.0500 2-Amino-2-Methyl-1,3-propanediol 2.1 % w/v AMPQ42009.0250 Barium Chloride 10% w/v AMPQ10513.1000 2-Propanol 35% AMPQ12900.5000 Barium Diphenylamine Sulfonate AMPQ40838.0500 Basophil Counting Solution AMPQ90492.0200 A Basophilic Colouring Solution AMPQ42037.0100 Acetate Buffer 0.1 M, pH 4.0 AMPQ10021.1000 Benzamidine 0.5 M in MilliQ H2O AMPQ10750.0100 Acetate Buffer 0.1 M, pH 4.8 AMPQ40728.1000 Benzoe I Colouring Solution AMPQ10779.0100 Acetate Buffer 0.1 M, pH 5.9 AMPQ43009.1000 Benzoe II Colouring Solution AMPQ10781.0100 Acetate Buffer 35%, pH 5.6 AMPQ10015.1000 Biebrich Scarlet Solution AMPQ46088.1000 Acetate Buffer Walpole pH 4.1 AMPQ55005.0500 Biebrich's Scarlet Acid Fuchsin AMPQ29082.0500 Acetic Acid 0.1 M Titrated AMPQ11590.5000 Bies Colouring Solution AMPQ10780.0050 Acetic Acid 1% AMPQ11515.1000 BiGGY Agar AMPQ02048.0015 Acetic Acid 10% P.A.