Use of 90% Ethanol to Decontaminate Stethoscopes in Resource Limited
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chemical Disinfectant and Cleaning Agent Safety – Frequently Asked Questions
Caribbean Public Health Agency Technical Guidance: COVID-19 Series No 33 Chemical Disinfectant and Cleaning Agent Safety – Frequently Asked Questions Suggested Citation: CARPHA. (2020). Chemical disinfectant and cleaning agent safety – frequently asked questions. Caribbean Public Health Agency Technical Guidance: COVID-19 Series, no. 33. CARPHA 2020 Chemical Disinfectant and Cleaning Agent Safety – Frequently Asked Questions 9 July 2020 Why are we concerned about cleaning agents and disinfectants? Selecting the correct chemical agent for cleaning and disinfecting and safely handling and using that agent is essential to health and wellbeing. Recently, with the increased focus on cleaning to reduce the risk of exposure to coronavirus disease, there have been an associated increase in media stories warning the public of the dangerous chemicals used for disinfectants. All chemical cleaning agents can be harmful to the health of the person using the product if it is not used as directed on the label by the manufacturer. Chemical agents can cause burns, breathing difficulties or damage to the lungs, or possibly result in poisoning. Persons should carefully read instructions for use, safety data sheets, and any health warnings to ensure they have selected the correct chemical agents, have the appropriate personal protection, and use and store the chemicals in a safe way. What are the properties of effective chemical cleaning agents and disinfectants? A wide variety of chemical agents can be used for cleaning, sanitising, and disinfecting. There are 4 categories of cleaners: detergents, degreasers, abrasives, and acids. Each is effective for cleaning different surfaces depending on the type of soiling. Different chemical agents are effective for killing different bacteria and viruses.1 Molds and fungus will require a sporicidal agent2. -

VOLUME 2 Cleaning Agents, Sanitisers and Disinfectants in Food Businesses: Detection of Traces and Human Risk Assessment Processes
Chemicals in Food Hygiene VOLUME 2 Cleaning agents, sanitisers and disinfectants in food businesses: detection of traces and human risk assessment processes Chemicals in Food Hygiene – Volume 2 Foreword The Global Food Safety Initiative (GFSI) is a considering carry-over risks of traces in non-profit industry association tasked with foods; promoting continuous improvement of food ➢ Reviewed and identified gaps in the safety management systems to ensure suitability of existing methods for confidence in the delivery of safe food to detection of traces at relevant points in consumers worldwide. GFSI provides a the food production process; platform for collaboration between some of ➢ Developed the GFSI position on the use of the world’s leading food safety experts from cleaning agents, sanitisers and retailer, producers and food service disinfectants and the relationship with companies, service providers associated with microbial resistance. the food supply chain, international organisations, academia and government. The TWG produced 2 volumes within one document: Since GFSI’s inception in 2000, experts from all over the world have been collaborating in ➢ Volume one of this document provides a numerous Technical Working Groups (TWG) high-level overview of the considerations to tackle current food safety issues defined that a food business operator needs to by GFSI stakeholders. In 2017 a TWG was consider in relation to ensuring established to determine best practices in appropriate hygienic practices. This relation to biocides (defined as the residues volume is aimed at a variety of readers from cleaning agents, sanitisers and from the food truck operator or farmer disinfectants) in the food supply chain. -

Knolltextiles Cleaning Information
Cleaning Information Regular Maintenance It is important to vacuum upholstery regularly to remove the surface dust that builds up and slowly contributes to a greying effect that diminishes the clarity of the original color. Please note that vacuuming should be done with the proper attachments to avoid breaking down the fibers and contributing to “pilling.” In addition to regular vacuuming, a professional cleaner should come in at least once or twice a year to thoroughly clean the fabrics and remove the soiling that a normal vacuum cleaner cannot reach. The expense of this service is small compared to the reward of seating that looks good as new after a lot of use. Cleaning Codes W: Water-based cleaning agents or foam may be used for cleaning this fabric. S: Only mild, pure water-free dry cleaning solvents may be used for cleaning this fabric. W-S: Water-based cleaning agents and foam or mild, waterfree solvents may be used for cleaning this fabric. W Bleach: Water-based or foam cleaning agents or diluted household bleach may be used for cleaning this fabric. W-S Bleach: Clean with water or solvent-based cleaning agents or diluted household bleach. X: This fabric should be vacuumed or brushed lightly to remove soil. Warning: Do not use water-based foam or liquid cleaning agents of any type on this fabric. Cleaning vs Sanitizing vs Disinfecting Cleaning, disinfecting and sanitizing are often used synonymously, but they are not the same thing. Cleaning removes the visible foreign matter from a surface. Disinfecting, when done according to the instructions of a suitable cleaner, kills all bacteria and viruses present, while sanitizing reduces the level of bacteria and viruses present. -
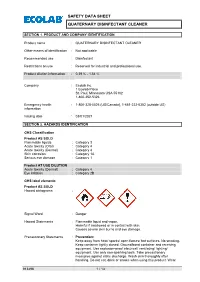
Safety Data Sheet Quaternary Disinfectant Cleaner
SAFETY DATA SHEET QUATERNARY DISINFECTANT CLEANER SECTION 1. PRODUCT AND COMPANY IDENTIFICATION Product name : QUATERNARY DISINFECTANT CLEANER Other means of identification : Not applicable Recommended use : Disinfectant Restrictions on use : Reserved for industrial and professional use. Product dilution information : 0.39 % - 1.54 % Company : Ecolab Inc. 1 Ecolab Place St. Paul, Minnesota USA 55102 1-800-352-5326 Emergency health : 1-800-328-0026 (US/Canada), 1-651-222-5352 (outside US) information Issuing date : 03/01/2021 SECTION 2. HAZARDS IDENTIFICATION GHS Classification Product AS SOLD Flammable liquids : Category 3 Acute toxicity (Oral) : Category 4 Acute toxicity (Dermal) : Category 4 Skin corrosion : Category 1A Serious eye damage : Category 1 Product AT USE DILUTION Acute toxicity (Dermal) : Category 4 Eye irritation : Category 2B GHS label elements Product AS SOLD Hazard pictograms : Signal Word : Danger Hazard Statements : Flammable liquid and vapor. Harmful if swallowed or in contact with skin. Causes severe skin burns and eye damage. Precautionary Statements : Prevention: Keep away from heat/ sparks/ open flames/ hot surfaces. No smoking. Keep container tightly closed. Ground/bond container and receiving equipment. Use explosion-proof electrical/ ventilating/ lighting/ equipment. Use only non-sparking tools. Take precautionary measures against static discharge. Wash skin thoroughly after handling. Do not eat, drink or smoke when using this product. Wear 913496 1 / 13 SAFETY DATA SHEET QUATERNARY DISINFECTANT CLEANER protective gloves/ protective clothing/ eye protection/ face protection. Response: IF SWALLOWED: Call a POISON CENTER/ doctor if you feel unwell. Rinse mouth. IF SWALLOWED: Rinse mouth. Do NOT induce vomiting. IF ON SKIN (or hair): Take off immediately all contaminated clothing. -

Apple Cider Vinegar Snakes Cage Cleaning
Apple cider vinegar snakes cage cleaning Apple cider vinegar snakes cage cleaning >>> Look Here <<< Wipe down cleaning: Using this method of tank cleaning you will be wiping the 10 Easy Steps to Reduce Odor Problems (or twice as often as changing litter that is in the whole bottom of the cage). Clean Apple cider vinegar can help never be used on a tank where an animal lives. Instead, try white vinegar. Control Fleas Naturally With Common Be sure and empty your vacuum after each cleaning or the pests Also put 1-3 tablespoons of apple cider vinegar in 05/12/2016 · Here's how to keep their cage clean, the way they » Rats; How to Keep Your Rat Cage Smelling Lovely. vinegar but not apple cider vinegar.fumes!Cider Vinegar Truth - Comments for My miracle snake oil "ACV" How? Simply click here to return to Apple Cider Vinegar and Weight Loss Stories. Home; The Vinegar Vinegar Cleaning 11 Comments on “Mel’s Top Bird Cleaning Tips For Even The Messiest of Species we wipe down the railes of the cages with solution of apple cider vinegar 16/09/2008 · Uses for Vinegar: Pet and Animal Care. with apple cider vinegar. Another ear-cleaning remedy is to the entire cage with vinegar on a because you Apple Cider Vinegar Then I let the vinegar cool down and use it for cleaning the coffee and we put her back into her cage and add one tablespoon of white different species in the tank, as some species are more susceptible than others to your normal wash load to remove bacterial residue and fresh them 01/11/2012 · The most complex liquid I use is hot water. -

Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008
Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 William A. Rutala, Ph.D., M.P.H.1,2, David J. Weber, M.D., M.P.H.1,2, and the Healthcare Infection Control Practices Advisory Committee (HICPAC)3 1Hospital Epidemiology University of North Carolina Health Care System Chapel Hill, NC 27514 2Division of Infectious Diseases University of North Carolina School of Medicine Chapel Hill, NC 27599-7030 1 Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 3HICPAC Members Robert A. Weinstein, MD (Chair) Cook County Hospital Chicago, IL Jane D. Siegel, MD (Co-Chair) University of Texas Southwestern Medical Center Dallas, TX Michele L. Pearson, MD (Executive Secretary) Centers for Disease Control and Prevention Atlanta, GA Raymond Y.W. Chinn, MD Sharp Memorial Hospital San Diego, CA Alfred DeMaria, Jr, MD Massachusetts Department of Public Health Jamaica Plain, MA James T. Lee, MD, PhD University of Minnesota Minneapolis, MN William A. Rutala, PhD, MPH University of North Carolina Health Care System Chapel Hill, NC William E. Scheckler, MD University of Wisconsin Madison, WI Beth H. Stover, RN Kosair Children’s Hospital Louisville, KY Marjorie A. Underwood, RN, BSN CIC Mt. Diablo Medical Center Concord, CA This guideline discusses use of products by healthcare personnel in healthcare settings such as hospitals, ambulatory care and home care; the recommendations are not intended for consumer use of the products discussed. 2 -
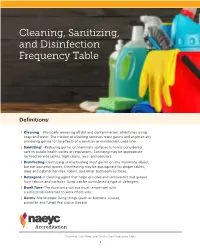
NAEYC Standard 5 (Health), Especially Topic C: Maintaining a Healthful Environment
Cleaning, Sanitizing, and Disinfection Frequency Table Definitions1 › Cleaning2 –Physically removing all dirt and contamination, oftentimes using soap and water. The friction of cleaning removes most germs and exposes any remaining germs to the effects of a sanitizer or disinfectant used later. › Sanitizing3 –Reducing germs on inanimate surfaces to levels considered safe by public health codes or regulations. Sanitizing may be appropriate for food service tables, high chairs, toys, and pacifiers. › Disinfecting–Destroying or inactivating most germs on any inanimate object, but not bacterial spores. Disinfecting may be appropriate for diaper tables, door and cabinet handles, toilets, and other bathroom surfaces. › Detergent–A cleaning agent that helps dissolve and remove dirt and grease from fabrics and surfaces. Soap can be considered a type of detergent. › Dwell Time–The duration a surface must remain wet with a sanitizer/disinfectant to work effectively. › Germs–Microscopic living things (such as bacteria, viruses, parasites and fungi) that cause disease. Cleaning, Sanitizing, and Disinfection Frequency Table 1 Cleaning, Sanitizing, and Disinfecting Frequency Table1 Relevant to NAEYC Standard 5 (Health), especially Topic C: Maintaining a Healthful Environment Before After Daily Areas each each (End of Weekly Monthly Comments4 Use Use the Day) Food Areas Clean, Clean, Food preparation Use a sanitizer safe for and then and then surfaces food contact Sanitize Sanitize If washing the dishes and utensils by hand, Clean, use a sanitizer safe -
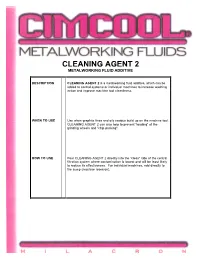
Cleaning Agent 2 Metalworking Fluid Additive
CLEANING AGENT 2 METALWORKING FLUID ADDITIVE DESCRIPTION CLEANING AGENT 2 is a metalworking fluid additive, which can be added to central systems or individual machines to increase washing action and improve machine tool cleanliness. WHEN TO USE Use when graphite fines and oily residue build up on the machine tool. CLEANING AGENT 2 can also help to prevent "loading" of the grinding wheels and "chip packing". HOW TO USE Pour CLEANING AGENT 2 directly into the "clean" side of the central filtration system where contamination is lowest and will be least likely to reduce its effectiveness. For individual machines, add directly to the sump (machine reservoir). RECOMMENDED FOR INDUSTRIAL USE ONLY STARTING Use dilution is 1:10,000 (0.01%) and 1:1,000 (0.1%). DILUTIONS CLEANING AGENT 2 is to be added to CIMCOOL® metalworking fluid mixes as described above. TYPICAL Physical state: Liquid PHYSICAL AND Appearance and odor: Clear, slight chemical CHEMICAL Colors available: Undyed PROPERTIES Solubility in water: 100% Miscible Weight, lb/gal, 60°F (15.6°C): 8.82 Specific gravity, (H2O = 1): 1.057 Boiling point, °F (°C): NA Flash point,COC,°F (°C): 477 (247.2) Fire point,COC, °F (°C): 540 (282.2) Extinguishing media: Chemical foam, carbon dioxide, water fog, dry chemical Unusual fire & explosion hazards: None Freezing point (or pour point), °F, (°C): 39 (3.9) If frozen, product separates. Thaw completely at room temperature and stir thoroughly. pH, concentrate: NA pH, 1.0% mix, typical operating conditions: 6.9 Total chlorine/chloride, wt%, calculated: 0.00/0.00 Total sulfur, wt%, calculated: 0.00 Silicones: None PACKAGING Available in 5-gallon pails and 55-gallon drums. -

Product Cleaning and Maintenance Care
Product Cleaning and Maintenance Care The best spaces manifest quality in proportion and material—from KnollTextiles colorful textiles, soft felts and leathers to wood, laminates and Knoll Office engineered polymers. Materials like these evoke simplicity and balance, KnollExtra coexisting with furniture to achieve Florence Knoll’s ideal—the spirit KnollStudio DatesWeiser of “total design.” Our extensive range of materials and dedication to SpinneyBeck | FilzFelt quality can complete your workspace, whether raw or refined. Muuto This product cleaning and maintenance care guide refers to the entire constellation of Knoll products. For additional Muuto cleaning guidance, please refer to Muuto’s Product Fact Sheets at: http://download.muuto.com/MediaLibrary/Product-Fact-Sheet Furniture that is comprised of multiple materials may require multiple cleaning and maintenance protocols. Refer to Knoll Price Lists to determine the component material and fabric options where applicable. Refer to this guide for how to clean and maintain each surface. Tested Disinfectant Formulas While Knoll cannot guarantee the efficacy of these products, when properly used in accordance with the manufacturers’ directions for use and dilution, they will not cause harm to the standard finishes below. These products have been tested on all standard Knoll Office veneers, laminates, paints, glass, aluminum and plated finishes. These products have been tested on all standard KnollStudio laminates, paints, glass, aluminum and plated finishes. These tested cleaners apply to these standard finishes only. (Additional testing is necessary for KnollStudio veneers as well as specialty finishes, DatesWeiser and Muuto.) + Envirox® H2Orange2 Concentrate 117 + Virox™ Accelerated™ Hydrogen Peroxide 5 + Envirox® EvolveO2™ ( GN×2 technology ) #1, Multi-Purpose Cleaner and Degreaser The Center for Disease Control (CDC) advises social distancing and handwashing to help prevent the spread of COVID-19. -

PP-CTD-US-0084-1 Bayer COVID Disinfectant Cleaning
Disinfecting Systems and Components A Bayer in Radiology COVID-19 Standards Guide Additional Information: Operations System or Specific Component For Reference, Excerpt of Cleaning/Disinfection View the most up-to-date Manual Bayer Recommendation (if applicable) Instructions from Product Operations Manual information on the EPA website: Reference https://www.epa.gov/pesticide-registration/ list-n-disinfectants-use-against-sars-cov-2 When cleaning after a suspected or confirmed COVID-19 patient, Bayer recommends throwing away any single use disposables component and transfer sets. For MEDRAD® Avanta Disposable Products Multi-Patient Sets and MEDRAD® Intego Source Administration Sets, an evaluation should be made to determine the best course. For MEDRAD® Intego SAS, the potential for excessive radiation exposure exists and should be considered prior to removing the set. When cleaning and disinfecting a Certegra Workstation, do not spray cleaning agent directly onto the Workstation display. Doing so could cause damage to the system, including the Certegra® Workstation touchscreen. Rather, follow the guidelines outlined below and be sure to refer to your Operation Manual for more specific instruction. ANGIOGRAPHY Bayer recommends following instructions published recently in the Bayer recommends that the MEDRAD® Avanta Fluid Avanta has specific warnings and cautions about Journal of the American College of Radiology, JACR. The authors user decontaminate with 70% Management Injection System 86480808 Rev. B cleaning that should be followed: (1) Warning: Do not recommend for systems like Avanta, to either wash with soap and > Fluid Control Module (FCM), isopropyl alcohol only for spray industrial cleaning solvents such as acetone to water or decontaminate using a low-level or intermediate-level decontamination for COVID-19. -

( 12 ) United States Patent ( 10 ) Patent No .: US 10,893,673 B2 Silvernail Et Al
US010893673B2 ( 12 ) United States Patent ( 10 ) Patent No .: US 10,893,673 B2 Silvernail et al . ( 45 ) Date of Patent : Jan. 19 , 2021 ( 54 ) QUATERNARY DISINFECTANT ( 52 ) U.S. CI . COMPOSITION WITH ANIONIC SCALE CPC AOIN 25/22 ( 2013.01 ) ; AOIN 25/02 INHIBITING AGENT ( 2013.01 ) ; A01N 33/04 ( 2013.01 ) ; AOIN 33/12 ( 2013.01 ) ; AOIN 57/20 ( 2013.01 ) ( 71 ) Applicant: ECOLAB USA INC , Saint Paul, MN ( 58 ) Field of Classification Search ( US ) CPC A01N 25/22 ; AOIN 25/02 ; A01N 57/20 ; AOIN 33/04 ; AO1N 33/12 ( 72 ) Inventors: Carter M. Silvernail, Saint Paul , MN See application file for complete search history . ( US ) ; Stefan Jaeger , Saint Paul , MN ( US ) ; Erin J. Dahlquist Howlett , Saint ( 56 ) References Cited Paul , MN ( US ); Michael Decker , Saint Paul , MN ( US ) U.S. PATENT DOCUMENTS 6,395,698 B1 5/2002 Daun et al . ( 73 ) Assignee : Ecolab USA Inc. , Saint Paul, MN (US ) 2011/0086791 A1 4/2011 Notte et al . 2016/0015030 A1 1/2016 Vanlaer ( * ) Notice : Subject to any disclaimer , the term of this patent is extended or adjusted under 35 FOREIGN PATENT DOCUMENTS U.S.C. 154 ( b ) by 0 days. EP 0343605 A1 11/1989 EP 1277403 B1 9/2005 ( 21 ) Appl. No .: 16 / 163,417 WO 2009080498 A1 7/2009 WO 2012121964 Al 9/2012 ( 22 ) Filed : Oct. 17 , 2018 WO 2015078496 Al 6/2015 Primary Examiner Robert S Cabral ( 65 ) Prior Publication Data ( 74 ) Attorney , Agent, or Firm — McKee , Voorhees & US 2019/0183117 A1 Jun . 20 , 2019 Sease , PLC ( 57 ) ABSTRACT Related U.S. -

Cleaning and Care Guide for Stainless Steel, Enviro-Glaze, Corterra, Plastic, Resin & Laminate/Melamine Surfaces
Cleaning and Care Guide For Stainless Steel, Enviro-Glaze, Corterra, Plastic, Resin & Laminate/Melamine Surfaces ACORN ENGINEERING P.O. Box 3527 City of Industry, CA 91744 U.S.A. Phone 800-591-9372 626-855-4804 Member of www.acorneng.com 9900-008-001 INSTALLATION, OPERATIONS & MAINTENANCE MANUAL Please visit www.acorneng.com for most current specifications. To Remove Smudges and Fingerprints: STAINLESS STEEL Wipe surfaces with a quality Stainless Steel cleaner/polish. Apply using a soft, non-abrasive cloth. Warning Always follow cleaner/polish product instructions and admonishments. F Do not mix different cleaning solutions. F Always read cleaning products label for proper To Remove Dirt and Debris: use and admonishments. Wash surfaces with a mild liquid soap using a soft cloth. Rinse surfaces thoroughly with clean water Normal Cleaning: followed by wiping dry with a soft non-abasive cloth Clean weekly or more often as needed (especially and stainless steel cleaner/polish. high polish or mirror finished surfaces). For best results always rinse well with fresh water and wipe dry with clean soft cloth. To Remove Rust Stains: Wipe surfaces with CRES Clean™ or equivalent cleaner or recommended solutions listed above. Recommended Cleaning Materials: Apply using a soft non-abrasive sponge. Rinse l Sponge - natural or artificial surfaces thoroughly with clean water followed by l Nylon or other soft bristle brush wiping dry with a soft non-abasive cloth and stainless l Micro-fiber Cloth steel cleaner/polish. Recommended Cleaning Solutions: For