Oup Humupd Dmz004 1..25 ++
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 9,394,315 B2 Aicher Et Al
USOO93943 15B2 (12) United States Patent (10) Patent No.: US 9,394,315 B2 Aicher et al. (45) Date of Patent: Jul.19, 2016 (54) TETRAHYDROI18NAPHTHYRIDINE 6,605,634 B2 8, 2003 Zablocki et al. SULFONAMIDE AND RELATED 6,638,960 B2 10/2003 Assmann et al. 6,683,091 B2 1/2004 Asberomet al. COMPOUNDS FOR USEAS AGONSTS OF 6,828,344 B1 12/2004 Seehra et al. RORY AND THE TREATMENT OF DISEASE 7,084, 176 B2 8, 2006 Morie et al. 7,138.401 B2 11/2006 Kasibhatla et al. (71) Applicant: Lycera Corporation, Ann Arbor, MI 7,329,675 B2 2/2008 Cox et al. 7,420,059 B2 9, 2008 O'Connor et al. (US) 7,482.342 B2 1/2009 D’Orchymont et al. 7,569,571 B2 8/2009 Dong et al. (72) Inventors: Thomas D. Aicher, Ann Arbor, MI (US); 7,696,200 B2 4/2010 Ackermann et al. Peter L. Toogood, Ann Arbor, MI (US); 7,713.996 B2 5/2010 Ackermann et al. Xiao Hu, Northville, MI (US) 7,741,495 B2 6, 2010 Liou et al. 7,799,933 B2 9/2010 Ceccarelli et al. (73) Assignee: Lycera Corporation, Ann Arbor, MI 2006,0004000 A1 1/2006 D'Orchymont et al. 2006/010O230 A1 5, 2006 Bischoff et al. (US) 2007/0010537 A1 1/2007 Hamamura et al. 2007/OO 10670 A1 1/2007 Hirata et al. (*) Notice: Subject to any disclaimer, the term of this 2007/0049556 A1 3/2007 Zhang et al. patent is extended or adjusted under 35 2007/0060567 A1 3/2007 Ackermann et al. -
High-Throughput H295R Steroidogenesis Assay: Utility As an Alternative and a Statistical Approach to Characterize Effects on Steroidogenesis Derik E
High-throughput H295R steroidogenesis assay: utility as an alternative and a statistical approach to characterize effects on steroidogenesis Derik E. Haggard ORISE Postdoctoral Fellow National Center for Computational Toxicology Computational Toxicology Communities of Practice Dec. 14th, 2017 The views expressed in this presentation are those of the author and do not necessarily reflect the views or policies of the U.S. EPA Outline • Background • Objectives • Assay Background • Methods and Results 1. Evaluation of the HT-H295R assay 2. Development of a quantitative prioritization metric for the HT-H295R assay data • Summary and Conclusions 2 Steroid Hormone Biosynthesis & Metabolism • Proper steroidogenesis is essential: • In utero for fetal development • In adults for reproductive function • Disruption can result in congenital adrenal hyperplasia, sterility, prenatal virilization, salt wasting, etc. • >90% of steroidogenesis occurs in the gonads • Leydig cells (males) or follicular cells (females) • Adrenal gland (corticosteroids) 3 https://www.pharmacorama.com/en/Sections/Androgen_steroid_hormones.php US EPA Endocrine Disruptor Screening Program (EDSP) • EDSP mandated to screen chemicals for endocrine activity (estrogen, androgen, thyroid) • Initial tiered screen relied on low-throughput assays • Modernization of EDSP (EDSP21) to use high-throughput and computational methods • Prioritize the universe of EDSP chemicals for endocrine bioactivity • Altering hormone levels via disruption of biosynthesis or metabolism can also contribute -

Supplemental File 11
Supplemental File 11 Supplemental Table 11. OECD Reference Chemical Performance in HT H295R versus OECD inter-laboratory results and literature-reported results. Chemical identifiers (chemical name and casn) are provided for the 25 reference chemicals that overlapped between high-throughput (HT) H295R screening and the OECD inter-laboratory validation study (Hecker et al., 2011). Trilostane, glyphosate, and human chorionic gonadotrophin were not screened in the HT H295R assay. The adjusted maxmMd value, quadrants of the steroid synthesis pathway affected (progestagens (P), glucocorticoids (G), androgens (A), and/or estrogens (E)), and the number of steroid hormones affected using the ANOVA-based logic described in the main text are also provided. The OECD inter-laboratory results for estradiol (E2) and testosterone (T) are summarized along with a brief overview of additional information from the reported literature for activity in the H295R assay (if other in vitro assay data are referenced, the assay type is provided). Only 2 of the 25 chemicals with overlapping data were reported as negative for effects on both E2 and T: ethylene dimethanesulfonate and benomyl. NA indicates that no concentration-response screening data were available (only single concentration screening available). # Chemical identifiers Results from HT H295R assay OECD Inter-laboratory and literature-reported Chemical name casn Adjusted maxmMd Quadrants # Steroid results of steroid hormones biosynthesis affected pathway affected 1 Mifepristone 84371-65-3 27 P 2 Used pharmacologically as an abortifacient with antiprogestagen, antiglucocorticoid, and antiandrogen properties. Moderate induction of E2 (2 to 4-fold induction) and T (equivocal) synthesis (Hecker, et al., 2011). Strong modulation of glucocorticoid pathway in H295R cells as a GR antagonist (Asser et al., 2014). -
Hormonal Side Effects in Patients Using Levetiracetam
Reproductive endocrine side effects of antiepileptic drugs Student Thesis Student: Marte Wendel Gustavsen Class V-03 University of Oslo, Norway Supervisor: Professor Erik Taubøll Department of Neurology, Rikshospitalet University Hospital, Oslo, Norway Contents Contents ...................................................................................................................................... 2 Acknowledgements .................................................................................................................... 3 Abstract ...................................................................................................................................... 4 Introduction ................................................................................................................................ 5 Reproductive endocrine effects of epilepsy ............................................................................... 5 Reproductive hormones can affect epilepsy ............................................................................... 7 Reproductive hormones can influence on AEDs ....................................................................... 9 Reproductive endocrine effects of AEDs ................................................................................... 9 Reproductive endocrine effects of valproate ........................................................................ 11 Women ............................................................................................................................ -

Residue Dynamics and Risk Assessment of Prochloraz and Its Metabolite 2,4,6-Trichlorophenol in Apple
Article Residue Dynamics and Risk Assessment of Prochloraz and Its Metabolite 2,4,6-Trichlorophenol in Apple Qingkui Fang 1, Gengyou Yao 2, Yanhong Shi 2, Chenchun Ding 1, Yi Wang 2, Xiangwei Wu 2, Rimao Hua 2 and Haiqun Cao 1,* 1 School of Plant Protection, Provincial Key Laboratory for Agri-Food Safety, Anhui Agricultural University, Hefei 230036, China; [email protected] (Q.F.); [email protected] (C.D.) 2 School of Resource & Environment, Provincial Key Laboratory for Agri-Food Safety, Anhui Agricultural University, Hefei 230036, China; [email protected] (G.Y.); [email protected] (Y.S.); [email protected] (Y.W.); [email protected] (X.W.); [email protected] (R.H.) * Correspondence: [email protected] Received: 22 September 2017; Accepted: 19 October 2017; Published: 20 October 2017 Abstract: The residue dynamics and risk assessment of prochloraz and its metabolite 2,4,6- trichlorophenol (2,4,6-TCP) in apple under different treatment concentrations were investigated using a GC-ECD method. The derivatization percent of prochloraz to 2,4,6-TCP was stable and complete. The recoveries of prochloraz and 2,4,6-TCP were 82.9%–114.4%, and the coefficients of variation (CV) were 0.7%–8.6% for the whole fruit, apple pulp, and apple peel samples. Under the application of 2 °C 2.0 g/L, 2 °C 1.0 g/L, 20 °C 2.0 g/L, and 20 °C 1.0 g/L treatment, the half-life for the degradation of prochloraz was 57.8–86.6 d in the whole fruit and apple peel, and the prochloraz concentration in the apple pulp increased gradually until a peak (0.72 mg·kg−1) was reached. -

A Cell-Free Testing Platform to Screen Chemicals of Potential Neurotoxic Concern Across Twenty Vertebrate Species
Environmental Toxicology and Chemistry, Vol. 36, No. 11, pp. 3081–3090, 2017 # 2017 SETAC Printed in the USA A CELL-FREE TESTING PLATFORM TO SCREEN CHEMICALS OF POTENTIAL NEUROTOXIC CONCERN ACROSS TWENTY VERTEBRATE SPECIES a,b a,b a,c,d a a,e ADELINE ARINI, KRITTIKA MITTAL, PETER DORNBOS, JESSICA HEAD, JENNIFER RUTKIEWICZ, a,b, and NILADRI BASU * aDepartment of Environmental Health Sciences, University of Michigan, Ann Arbor, Michigan, USA bFaculty of Agricultural and Environmental Sciences, McGill University, Montreal, Quebec, Canada cDepartment of Biochemistry and Molecular Biology, Michigan State University, East Lansing, Michigan, USA dInstitute for Integrative Toxicology, Michigan State University, East Lansing, Michigan, USA eToxServices, Ann Arbor, Michigan, USA (Submitted 8 February 2017; Returned for Revision 9 March 2017; Accepted 5 June 2017) Abstract: There is global demand for new in vitro testing tools for ecological risk assessment. The objective of the present study was to apply a set of cell-free neurochemical assays to screen many chemicals across many species in a relatively high-throughput manner. The platform assessed 7 receptors and enzymes that mediate neurotransmission of g-aminobutyric acid, dopamine, glutamate, and acetylcholine. Each assay was optimized to work across 20 vertebrate species (5 fish, 5 birds, 7 mammalian wildlife, 3 biomedical species including humans). We tested the screening assay platform against 80 chemicals (23 pharmaceuticals and personal care products, 20 metal[loid]s, 22 polycyclic aromatic hydrocarbons and halogenated organic compounds, 15 pesticides). In total, 10 800 species–chemical–assay combinations were tested, and significant differences were found in 4041 cases. All 7 assays were significantly affected by at least one chemical in each species tested. -

QSAR Model for Androgen Receptor Antagonism
s & H oid orm er o t n S f a l o S l c a Journal of i n e Jensen et al., J Steroids Horm Sci 2012, S:2 r n u c o e DOI: 10.4172/2157-7536.S2-006 J ISSN: 2157-7536 Steroids & Hormonal Science Research Article Open Access QSAR Model for Androgen Receptor Antagonism - Data from CHO Cell Reporter Gene Assays Gunde Egeskov Jensen*, Nikolai Georgiev Nikolov, Karin Dreisig, Anne Marie Vinggaard and Jay Russel Niemelä National Food Institute, Technical University of Denmark, Department of Toxicology and Risk Assessment, Mørkhøj Bygade 19, 2860 Søborg, Denmark Abstract For the development of QSAR models for Androgen Receptor (AR) antagonism, a training set based on reporter gene data from Chinese hamster ovary (CHO) cells was constructed. The training set is composed of data from the literature as well as new data for 51 cardiovascular drugs screened for AR antagonism in our laboratory. The data set represents a wide range of chemical structures and various functions. Twelve percent of the screened drugs were AR antagonisms; three out of six statins showed AR antagonism, two showed cytotoxicity and one was negative. The newly identified AR antagonisms are: Lovastatin, Simvastatin, Mevastatin, Amiodaron, Docosahexaenoic acid and Dilazep. A total of 874 (231 positive, 643 negative) chemicals constitute the training set for the model. The Case Ultra expert system was used to construct the QSAR model. The model was cross-validated (leave-groups-out) with a concordance of 78.4%, a specificity of 86.1% and a sensitivity of 57.9%. -

Chronic Hazard Advisory Panel on Phthalates and Phthalate Alternatives
Report to the U.S. Consumer Product Safety Commission by the CHRONIC HAZARD ADVISORY PANEL ON PHTHALATES AND PHTHALATE ALTERNATIVES July 2014 U.S. Consumer Product Safety Commission Directorate for Health Sciences Bethesda, MD 20814 Chronic Hazard Advisory Panel on Phthalates and Phthalate Alternatives Chris Gennings, Ph.D. Virginia Commonwealth University Richmond, VA Russ Hauser, M.D., Sc.D., M.P.H. Harvard School of Public Health Boston, MA Holger M. Koch, Ph.D. Ruhr University Bochum, Germany Andreas Kortenkamp, Ph.D. Brunel University London, United Kingdom Paul J. Lioy, Ph.D. Robert Wood Johnson Medical School Piscataway, NJ Philip E. Mirkes, Ph.D. University of Washington (retired) Seattle, WA Bernard A. Schwetz, D.V.M., Ph.D. Department of Health and Human Services (retired) Washington, DC TABLE OF CONTENTS LIST OF TABLES ....................................................................................................................... iv LIST OF FIGURES ..................................................................................................................... vi ABBREVIATIONS ..................................................................................................................... vii 1 Executive Summary .............................................................................................................. 1 2 Background and Strategy................................................................................................... 11 2.1 Introduction and Strategy Definition ........................................................................... -

Temporal Records of Organic Contaminants in Lake Sediments, Their Bioconcentration and Effect on Daphnia Resting Eggs
Eawag_08974 Diss. ETH No. 21354 Temporal records of organic contaminants in lake sediments, their bioconcentration and effect on Daphnia resting eggs A dissertation submitted to the ETH ZURICH for the degree of Doctor of Sciences presented by AUREA CECILIA HERNANDEZ RAMIREZ OTHER FORMATS: AUREA CECILIA CHIAIA-HERNANDEZ MSc. In Chemistry, Oregon State University born 7 August 1980 citizen of Mexico accepted on the recommendation of Prof. Dr. Juliane Hollender, examiner Prof. Dr. Bernhard Wehrli, co-examiner Prof. Dr. Lee Ferguson, co-examiner PD. Dr. Piet Spaak, co-examiner 2014 ii Contents Summary vii Zusammenfassung xi 1 Introduction 1 1.1 Eutrophication and Anthropogenic Induced Environmental Changes . 2 1.2 Organic Pollutants in Sediments . 2 1.3 Analytical Procedures for the Detection and Identification of Parent Com- pounds and Transformation Products . 4 1.4 Daphnia as a Model Organism . 5 1.5 Bioaccumulation and Effects of Organic Contaminants . 6 1.6 Objectives and Contents of the Thesis . 7 2 Screening of Lake Sediments for Emerging Contaminants by Liquid Chro- matography Atmospheric Pressure Photoionization and Electrospray Ion- ization Coupled to High Resolution Mass Spectrometry 15 2.1 Introduction . 16 2.2ExperimentalSection............................. 18 2.2.1 Standards and Reagents . 18 2.2.2 Sample Collection and Preservation . 18 2.2.3ExtractionofSediments........................ 19 2.2.4 Clean-up and Enrichment of Sediment Extracts . 19 iii 2.2.5 Liquid Chromatography Tandem High Resolution Mass Spectro- metricDetection............................ 20 2.2.6AccuracyandPrecision........................ 21 2.2.7 Limits of Detection and Quantification . 21 2.2.8 Suspect Screening of Further Contaminants and Transformation Products . 21 2.2.9ProtonAffinityData......................... -

NEWS 02 2020 ENG.Qxp Layout 1
Polymers and fluorescence Balance of power 360° drinking water analysis trilogy Fluorescence spectroscopy LCMS-8060NX: performance of industrial base polymers and robustness without Automatic, simultaneous and compromising sensitivity rapid analysis of pesticides and speed CONTENT APPLICATION »Plug und Play« disease screening solution? – The MALDI-8020 in screening for Sickle Cell Disease 4 Customized software solutions for any measurement – Macro programming for Shimadzu UV-Vis and FTIR 8 Ensuring steroid-free food supplements – Identification of steroids in pharmaceuticals and food supplements with LCMS-8045 11 MSn analysis of nonderivatized and Mtpp-derivatized peptides – Two recent studies applying LCMS-IT-TOF instruments 18 Polymers and fluorescence – Part 2: How much fluorescence does a polymer show during quality control? 26 PRODUCTS The balance of power – LCMS-8060NX balances enhanced performance and robustness 7 360° drinking water analysis: Episode 2 – Automatic, simul- taneous and rapid analysis of pesticides in drinking water by online SPE and UHPLC-MS/MS 14 Versatile testing tool for the automotive industry – Enrico Davoli with the PESI-MS system (research-use only [RUO] instrument) New HMV-G3 Series 17 No more headaches! A guide to choosing the perfect C18 column 22 Validated method for monoclonal antibody drugs – Assessment of the nSMOL methodology in Global solution through the validation of bevacizumab in human serum 24 global collaboration LATEST NEWS Global solution through global collaboration – Shimadzu Cancer diagnosis: -
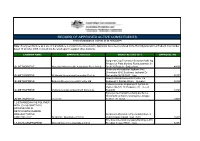
RECORD of APPROVED ACTIVE CONSTITUENTS This Information Is Current As at 19/02/2014
RECORD OF APPROVED ACTIVE CONSTITUENTS This information is current as at 19/02/2014 Note: Evergreen Nurture as a site of manufacture is known to be non-existent. Approvals have been restored to the Record pursuant to a Federal Court Order dated 13 October 2008. It should not be relied upon to support other products. COMMON NAME APPROVAL HOLDER MANUFACTURE SITE APPROVAL NO. Syngenta Crop Protection Schweizerhalle Ag Production Plant Muttenz Rothausstrasse 61 (S)-METHOPRENE Novartis Animal Health Australasia Pty. Limited Ch-4133 Pratteln Switzerland 44095 Wellmark International Jayhawk Fine Chemicals 8545 Southeast Jayhawk Dr (S)-METHOPRENE Wellmark International (australia) Pty Ltd Galena Ks 66739-0247 Usa 55179 Babolna Bioenvironmental Centre Ltd (S)-METHOPRENE Babolna Bioenvironmental Centre Ltd Budapest X Szallas Utca 6 Hungary 58495 Vyzkumny Ustav Organickych Syntez As Rybitvi 296 532 18 Pardubice 20 Czech (S)-METHOPRENE Vyzkumny Ustav Organickych Zyntez As Republic 59145 Synergetica-changzhou Gang Qu Bei Lu Weitang New District Changzhou Jiangsu (S)-METHOPRENE Zocor Inc 213033 Pr China 59428 1,2-ETHANEDIAMINE POLYMER WITH (CHLOROMETHYL) OXIRANE AND N- METHYLMETHANAMINE MANUFACTURING Buckman Laboratories Pty Ltd East Bomen CONCENTRATE Buckman Laboratories Pty Ltd Road Wagga Wagga Nsw 2650 56821 The Dow Chemical Company Building A-915 1,3-DICHLOROPROPENE Dow Agrosciences Australia Limited Freeport Texas 77541 Usa 52481 COMMON NAME APPROVAL HOLDER MANUFACTURE SITE APPROVAL NO. Dow Chemical G.m.b.h. Werk Stade D-2160 1,3-DICHLOROPROPENE Dow Agrosciences Australia Limited Stade Germany 52747 Agroquimicos De Levante (dalian) Company Limited 223-1 Jindong Road Jinzhou District 1,3-DICHLOROPROPENE Agroquimicos De Levante, S.a. -

Poraz® an Emulsifiable Concentrate Containing 450 G/Litre Prochloraz
® MAPP 11701 An emulsifiable concentrate containing 450 g/litre (39.8% w/w) prochloraz. PorazA broad-spectrum fungicide for use on wheat, barley, winter rye and winter oilseed rape. The (COSHH) Control of Substances Hazardous to Health Regulations may apply to the use of this product at work. SAFETY PRECAUTIONS Environmental protection Do not contaminate surface waters or ditches with Operator protection Engineering control of operator exposure must be used chemical or used container. where reasonably practicable in addition to the following Storage and disposal personal protective equipment: DO NOT RE-USE CONTAINER for any purpose. WEAR SUITABLE PROTECTIVE GLOVES AND FACE KEEP AWAY FROM FOOD, DRINK AND ANIMAL PROTECTION (FACESHIELD) when handling the FEEDING STUFFS. concentrate. KEEP OUT OF REACH OF CHILDREN. However, engineering controls may replace personal KEEP IN ORIGINAL CONTAINER, tightly closed in a protective equipment if a COSHH assessment shows safe place. that they provide an equal or higher standard of WASH OUT CONTAINER THOROUGHLY, empty protection. washings into spray tank and dispose of safely. WHEN USING DO NOT EAT, DRINK OR SMOKE. Store in a safe, dry, frost-free place designated as an WASH CONCENTRATE from skin or eyes immediately. agrochemical store. WASH HANDS AND EXPOSED SKIN before meals PROTECT FROM FROST. and after work. IF YOU FEEL UNWELL, seek medical advice (show leaflet where possible). This label is compliant UN 3082 with the CPA Voluntary Packing Group III Initiative Guidance Environmentally hazardous substance, liquid, N.O.S. (contains solvent naphtha, prochloraz 40%) L Marine Pollutant 5Supplied by: BASF plc Crop Protection PO Box 4, Earl Road Cheadle Hulme, CHEADLE Cheshire SK8 6QG Tel: 0161 485 6222 Emergency Information: (24 hours freephone): 0049 180 2273112 Technical Enquiries: 0845 602 2553 (office hours) 81075028GB1033 ® = Registered trademark of BASF Poraz® An emulsifiable concentrate containing 450 g/litre prochloraz.