Appendix B Androgen 07/03 13 DRAFT -- DO NOT CITE OR QUOTE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Investigating Non-Targeted Screening and Accurate Quantitation of Trace Surface Water Contaminants Using High-Resolution Mass Spectrometry
Western University Scholarship@Western Electronic Thesis and Dissertation Repository 8-8-2018 3:00 PM Investigating non-targeted screening and accurate quantitation of trace surface water contaminants using high-resolution mass spectrometry Lucas M. Morrison The University of Western Ontario Supervisor Sumarah, Mark W. The University of Western Ontario Co-Supervisor Yeung, Ken K-C. The University of Western Ontario Graduate Program in Chemistry A thesis submitted in partial fulfillment of the equirr ements for the degree in Master of Science © Lucas M. Morrison 2018 Follow this and additional works at: https://ir.lib.uwo.ca/etd Part of the Analytical Chemistry Commons, and the Environmental Chemistry Commons Recommended Citation Morrison, Lucas M., "Investigating non-targeted screening and accurate quantitation of trace surface water contaminants using high-resolution mass spectrometry" (2018). Electronic Thesis and Dissertation Repository. 5612. https://ir.lib.uwo.ca/etd/5612 This Dissertation/Thesis is brought to you for free and open access by Scholarship@Western. It has been accepted for inclusion in Electronic Thesis and Dissertation Repository by an authorized administrator of Scholarship@Western. For more information, please contact [email protected]. Abstract The human impact on surface water is a growing concern and the chemical surveying of contaminants including pharmaceuticals and pesticides is currently lacking. Neonicotinoids in particular, are among the most widely used insecticides that have prompted environmental concern and require monitoring. Chemical contaminants in environmental water samples are commonly analyzed by targeted tandem mass spectrometry. However, this requires a prior knowledge of the contaminants in the area of interest. Here, surface water samples were screened by utilizing optimized data-independent acquisition (DIA) methods and the spectra were databased for future retrospective analysis. -

Evaluation of Tebuconazole, Triclosan, Methylparaben and Ethylparaben According to the Danish Proposal for Criteria for Endocrine Disrupters
Downloaded from orbit.dtu.dk on: Sep 26, 2021 Evaluation of tebuconazole, triclosan, methylparaben and ethylparaben according to the Danish proposal for criteria for endocrine disrupters Hass, Ulla; Christiansen, Sofie; Petersen, Marta Axelstad; Boberg, Julie; Andersson, Anna-Maria ; Skakkebæk, Niels Erik ; Bay, Katrine ; Holbech, Henrik ; Lund Kinnberg, Karin ; Bjerregaard, Poul Publication date: 2012 Document Version Publisher's PDF, also known as Version of record Link back to DTU Orbit Citation (APA): Hass, U., Christiansen, S., Petersen, M. A., Boberg, J., Andersson, A-M., Skakkebæk, N. E., Bay, K., Holbech, H., Lund Kinnberg, K., & Bjerregaard, P. (2012). Evaluation of tebuconazole, triclosan, methylparaben and ethylparaben according to the Danish proposal for criteria for endocrine disrupters. Danish Centre on Endocrine Disrupters. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Users may download and print one copy of any publication from the public portal for the purpose of private study or research. You may not further distribute the material or use it for any profit-making activity or commercial gain You may freely distribute the URL identifying the publication in the public portal If you believe that this document breaches copyright please contact us providing details, and we will -
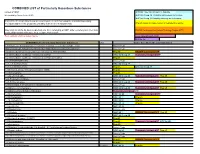
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -
OECD Environment Health and Safety Publications Series on Testing and Assessment No
OECD Environment Health and Safety Publications Series on Testing and Assessment No. 21 Detailed Review Paper Appraisal of Test Methods for Sex Hormone Disrupting Chemicals Environment Directorate ORGANISATION FOR ECONOMIC CO-OPERATION AND DEVELOPMENT Paris May 2001 1 Also Published in the Series Testing and Assessment: No. 1, Guidance Document for the Development of OECD Guidelines for Testing of Chemicals (1993; reformatted 1995) No. 2, Detailed Review Paper on Biodegradability Testing (1995) No. 3, Guidance Document for Aquatic Effects Assessment (1995) No. 4, Report of the OECD Workshop on Environmental Hazard/Risk Assessment (1995) No. 5, Report of the SETAC/OECD Workshop on Avian Toxicity Testing (1996) No. 6, Report of the Final Ring-test of the Daphnia magna Reproduction Test (1997) No. 7, Guidance Document on Direct Phototransformation of Chemicals in Water (1997) No. 8, Report of the OECD Workshop on Sharing Information about New Industrial Chemicals Assessment (1997) No. 9 Guidance Document for the Conduct of Studies of Occupational Exposure to Pesticides During Agricultural Application (1997) No. 10, Report of the OECD Workshop on Statistical Analysis of Aquatic Toxicity Data (1998) No. 11, Detailed Review Paper on Aquatic Testing Methods for Pesticides and industrial Chemicals (1998) No. 12, Detailed Review Document on Classification Systems for Germ Cell Mutagenicity in OECD Member Countries (1998) No. 13, Detailed Review Document on Classification Systems for Sensitising Substances in OECD Member Countries 1998) No. 14, Detailed Review Document on Classification Systems for Eye Irritation/Corrosion in OECD Member Countries (1998) No. 15, Detailed Review Document on Classification Systems for Reproductive Toxicity in OECD Member Countries (1998) No. -

(12) United States Patent (10) Patent No.: US 9,394,315 B2 Aicher Et Al
USOO93943 15B2 (12) United States Patent (10) Patent No.: US 9,394,315 B2 Aicher et al. (45) Date of Patent: Jul.19, 2016 (54) TETRAHYDROI18NAPHTHYRIDINE 6,605,634 B2 8, 2003 Zablocki et al. SULFONAMIDE AND RELATED 6,638,960 B2 10/2003 Assmann et al. 6,683,091 B2 1/2004 Asberomet al. COMPOUNDS FOR USEAS AGONSTS OF 6,828,344 B1 12/2004 Seehra et al. RORY AND THE TREATMENT OF DISEASE 7,084, 176 B2 8, 2006 Morie et al. 7,138.401 B2 11/2006 Kasibhatla et al. (71) Applicant: Lycera Corporation, Ann Arbor, MI 7,329,675 B2 2/2008 Cox et al. 7,420,059 B2 9, 2008 O'Connor et al. (US) 7,482.342 B2 1/2009 D’Orchymont et al. 7,569,571 B2 8/2009 Dong et al. (72) Inventors: Thomas D. Aicher, Ann Arbor, MI (US); 7,696,200 B2 4/2010 Ackermann et al. Peter L. Toogood, Ann Arbor, MI (US); 7,713.996 B2 5/2010 Ackermann et al. Xiao Hu, Northville, MI (US) 7,741,495 B2 6, 2010 Liou et al. 7,799,933 B2 9/2010 Ceccarelli et al. (73) Assignee: Lycera Corporation, Ann Arbor, MI 2006,0004000 A1 1/2006 D'Orchymont et al. 2006/010O230 A1 5, 2006 Bischoff et al. (US) 2007/0010537 A1 1/2007 Hamamura et al. 2007/OO 10670 A1 1/2007 Hirata et al. (*) Notice: Subject to any disclaimer, the term of this 2007/0049556 A1 3/2007 Zhang et al. patent is extended or adjusted under 35 2007/0060567 A1 3/2007 Ackermann et al. -
OECD Conceptual Framework for Testing and Assessment of Endocrine Disrupters As a Basis for Regulation of Substances with Endocrine Disrupting Properties
OECDOECD ConceptualConceptual FrameworkFramework for forTesting Testing and and Assessment Assessment of Endocrineof EndocrineDisrupters Disruptersas a basis asfor aregulation basis of forsubstances regulation with of substances endocrine disrupting with endocrineproperties disrupting properties Ulla Hass, Majken Dalgaard, Kirsten Jarfelt and Thuri S.A. Kledal Department of Toxicology and Risk Assessment, Danish Institute for Food and Veterinary Research, Denmark TemaNord 2004:555 OECD Conceptual Framework for Testing and Assessment of Endocrine Disrupters as a basis for regulation of substances with endocrine disrupting properties TemaNord 2004:555 © Nordic Council of Ministers, Copenhagen 2004 ISBN 92-893-1073-1 ISSN 0908-6692 Nordic Council of Ministers Nordic Council Store Strandstræde 18 Store Strandstræde 18 DK-1255 Copenhagen K DK-1255 Copenhagen K Phone (+45) 3396 0200 Phone (+45) 3396 0400 Fax (+45) 3396 0202 Fax (+45) 3311 1870 www.norden.org Nordic Environmental Co-operation Environmental co-operation is aimed at contributing to the improvement of the environment and forestall problems in the Nordic countries as well as on the international scene. The co- operation is conducted by the Nordic Committee of Senior Officials for Environmental Affairs. The co-operation endeavours to advance joint aims for Action Plans and joint projects, exchange of information and assistance, e.g. to Eastern Europe, through the Nordic Environmental Finance Corporation (NEFCO). The Nordic Council of Ministers was established in 1971. It submits proposals on co-operation between the governments of the five Nordic countries to the Nordic Council, implements the Council's recommendations and reports on results, while directing the work carried out in the targeted areas. The Prime Ministers of the five Nordic countries assume overall responsibility for the co-operation measures, which are co-ordinated by the ministers for co-operation and the Nordic Co-operation committee. -

Fighting Bisphenol A-Induced Male Infertility: the Power of Antioxidants
antioxidants Review Fighting Bisphenol A-Induced Male Infertility: The Power of Antioxidants Joana Santiago 1 , Joana V. Silva 1,2,3 , Manuel A. S. Santos 1 and Margarida Fardilha 1,* 1 Department of Medical Sciences, Institute of Biomedicine-iBiMED, University of Aveiro, 3810-193 Aveiro, Portugal; [email protected] (J.S.); [email protected] (J.V.S.); [email protected] (M.A.S.S.) 2 Institute for Innovation and Health Research (I3S), University of Porto, 4200-135 Porto, Portugal 3 Unit for Multidisciplinary Research in Biomedicine, Institute of Biomedical Sciences Abel Salazar, University of Porto, 4050-313 Porto, Portugal * Correspondence: [email protected]; Tel.: +351-234-247-240 Abstract: Bisphenol A (BPA), a well-known endocrine disruptor present in epoxy resins and poly- carbonate plastics, negatively disturbs the male reproductive system affecting male fertility. In vivo studies showed that BPA exposure has deleterious effects on spermatogenesis by disturbing the hypothalamic–pituitary–gonadal axis and inducing oxidative stress in testis. This compound seems to disrupt hormone signalling even at low concentrations, modifying the levels of inhibin B, oestra- diol, and testosterone. The adverse effects on seminal parameters are mainly supported by studies based on urinary BPA concentration, showing a negative association between BPA levels and sperm concentration, motility, and sperm DNA damage. Recent studies explored potential approaches to treat or prevent BPA-induced testicular toxicity and male infertility. Since the effect of BPA on testicular cells and spermatozoa is associated with an increased production of reactive oxygen species, most of the pharmacological approaches are based on the use of natural or synthetic antioxidants. -
Toxicological Profile for Bisphenol A
TT TOXICOLOGICAL PROFILE FOR BISPHENOL A September 2009 Integrated Risk Assessment Branch Office of Environmental Health Hazard Assessment California Environmental Protection Agency Toxicological Profile for Bisphenol A September 2009 Prepared by Office of Environmental Health Hazard Assessment Prepared for Ocean Protection Council Under an Interagency Agreement, Number 07-055, with the State Coastal Conservancy LIST OF CONTRIBUTORS Authors Jim Carlisle, D.V.M., Ph.D., Senior Toxicologist, Integrated Risk Assessment Branch Dave Chan, D. Env., Staff Toxicologist, Integrated Risk Assessment Branch Mari Golub, Ph.D., Staff Toxicologist, Reproductive and Cancer Hazard Assessment Branch Sarah Henkel, Ph.D., California Sea Grant Fellow, California Ocean Science Trust Page Painter, M.D., Ph.D., Senior Toxicologist, Integrated Risk Assessment Branch K. Lily Wu, Ph.D., Associate Toxicologist, Reproductive and Cancer Hazard Assessment Branch Reviewers David Siegel, Ph.D., Chief, Integrated Risk Assessment Branch i Table of Contents Executive Summary ................................................................................................................................ iv Use and Exposure ............................................................................................................................... iv Environmental Occurrence ................................................................................................................. iv Effects on Aquatic Life ...................................................................................................................... -

Detection of Estrogen Receptor Endocrine Disruptor Potency of Commonly Used Organochlorine Pesticides Using the LUMI-CELL ER Bioassay
DEVELOPMENTAL AND REPRODUCTIVE TOXICITY Detection of Estrogen Receptor Endocrine Disruptor Potency of Commonly Used Organochlorine Pesticides Using The LUMI-CELL ER Bioassay John D. Gordon1, Andrew C: Chu1, Michael D. Chu2, Michael S. Denison3, George C. Clark1 1Xenobiotic Detection Systems, Inc., 1601 E. Geer St., Suite S, Durham, NC 27704, USA 2Alta Analytical Perspectives, 2714 Exchange Drive, Wilmington, NC 28405, USA 3Dept. of Environmental Toxicology, Meyer Hall, Univ. of California, Davis; Davis, CA 95616 USA Introduction Organochlorine pesticides are found in many ecosystems worldwide as result of agricultural and industrial activities and exist as complex mixtures. The use of these organochlorine pesticides has resulted in the contamination of lakes and streams, and eventually the animal and human food chain. Many of these pesticides, such as pp ’-DDT, pp ’-DDE, Kepone, Vinclozolin, and Methoxychlor (a substitute for the banned DDT), have been described as putative estrogenic endocrine disruptors, and act by mimicking endogenous estrogen 1-3 . Estrogenic compounds can have a significant detrimental effect on the endocrine and reproductive systems of both human and other animal populations 4 . Previous studies have shown a strong association between several EDCs (17p-Estradiol, DES, Zeralanol, Zeralenone, Coumestrol, Genistein, Biochanin A, Diadzein, Naringenin, Tamoxifin) and estrogenic activity via uterotropic assay, cell height, gland number, increased lactoferrin, and a transcriptional activity assay using BG1Luc4E2 cells4 . Some other examples of the effects of these EDCs are: decreased reproductive success and feminization of males in several wildlife species; increased hypospadias along with reductions in sperm counts in men; increase in the incidence of human breast and prostate cancers; and endometriosis 3-5 . -
High-Throughput H295R Steroidogenesis Assay: Utility As an Alternative and a Statistical Approach to Characterize Effects on Steroidogenesis Derik E
High-throughput H295R steroidogenesis assay: utility as an alternative and a statistical approach to characterize effects on steroidogenesis Derik E. Haggard ORISE Postdoctoral Fellow National Center for Computational Toxicology Computational Toxicology Communities of Practice Dec. 14th, 2017 The views expressed in this presentation are those of the author and do not necessarily reflect the views or policies of the U.S. EPA Outline • Background • Objectives • Assay Background • Methods and Results 1. Evaluation of the HT-H295R assay 2. Development of a quantitative prioritization metric for the HT-H295R assay data • Summary and Conclusions 2 Steroid Hormone Biosynthesis & Metabolism • Proper steroidogenesis is essential: • In utero for fetal development • In adults for reproductive function • Disruption can result in congenital adrenal hyperplasia, sterility, prenatal virilization, salt wasting, etc. • >90% of steroidogenesis occurs in the gonads • Leydig cells (males) or follicular cells (females) • Adrenal gland (corticosteroids) 3 https://www.pharmacorama.com/en/Sections/Androgen_steroid_hormones.php US EPA Endocrine Disruptor Screening Program (EDSP) • EDSP mandated to screen chemicals for endocrine activity (estrogen, androgen, thyroid) • Initial tiered screen relied on low-throughput assays • Modernization of EDSP (EDSP21) to use high-throughput and computational methods • Prioritize the universe of EDSP chemicals for endocrine bioactivity • Altering hormone levels via disruption of biosynthesis or metabolism can also contribute -

WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/107 (2006.01) A61K 9/00 (2006.01) kind of national protection available): AE, AG, AL, AM, A 61 47/10 (2006.0V) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, PCT/US2012/034361 HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, (22) International Filing Date: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 20 April 2012 (20.04.2012) MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/480,259 28 April 201 1 (28.04.201 1) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (71) Applicant (for all designated States except US): BOARD UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, OF REGENTS, THE UNIVERSITY OF TEXAS SYS¬ TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, TEM [US/US]; 201 West 7th St., Austin, TX 78701 (US). -

Supplemental File 11
Supplemental File 11 Supplemental Table 11. OECD Reference Chemical Performance in HT H295R versus OECD inter-laboratory results and literature-reported results. Chemical identifiers (chemical name and casn) are provided for the 25 reference chemicals that overlapped between high-throughput (HT) H295R screening and the OECD inter-laboratory validation study (Hecker et al., 2011). Trilostane, glyphosate, and human chorionic gonadotrophin were not screened in the HT H295R assay. The adjusted maxmMd value, quadrants of the steroid synthesis pathway affected (progestagens (P), glucocorticoids (G), androgens (A), and/or estrogens (E)), and the number of steroid hormones affected using the ANOVA-based logic described in the main text are also provided. The OECD inter-laboratory results for estradiol (E2) and testosterone (T) are summarized along with a brief overview of additional information from the reported literature for activity in the H295R assay (if other in vitro assay data are referenced, the assay type is provided). Only 2 of the 25 chemicals with overlapping data were reported as negative for effects on both E2 and T: ethylene dimethanesulfonate and benomyl. NA indicates that no concentration-response screening data were available (only single concentration screening available). # Chemical identifiers Results from HT H295R assay OECD Inter-laboratory and literature-reported Chemical name casn Adjusted maxmMd Quadrants # Steroid results of steroid hormones biosynthesis affected pathway affected 1 Mifepristone 84371-65-3 27 P 2 Used pharmacologically as an abortifacient with antiprogestagen, antiglucocorticoid, and antiandrogen properties. Moderate induction of E2 (2 to 4-fold induction) and T (equivocal) synthesis (Hecker, et al., 2011). Strong modulation of glucocorticoid pathway in H295R cells as a GR antagonist (Asser et al., 2014).