Toxicological Profile for Bisphenol A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Tebuconazole, Triclosan, Methylparaben and Ethylparaben According to the Danish Proposal for Criteria for Endocrine Disrupters
Downloaded from orbit.dtu.dk on: Sep 26, 2021 Evaluation of tebuconazole, triclosan, methylparaben and ethylparaben according to the Danish proposal for criteria for endocrine disrupters Hass, Ulla; Christiansen, Sofie; Petersen, Marta Axelstad; Boberg, Julie; Andersson, Anna-Maria ; Skakkebæk, Niels Erik ; Bay, Katrine ; Holbech, Henrik ; Lund Kinnberg, Karin ; Bjerregaard, Poul Publication date: 2012 Document Version Publisher's PDF, also known as Version of record Link back to DTU Orbit Citation (APA): Hass, U., Christiansen, S., Petersen, M. A., Boberg, J., Andersson, A-M., Skakkebæk, N. E., Bay, K., Holbech, H., Lund Kinnberg, K., & Bjerregaard, P. (2012). Evaluation of tebuconazole, triclosan, methylparaben and ethylparaben according to the Danish proposal for criteria for endocrine disrupters. Danish Centre on Endocrine Disrupters. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Users may download and print one copy of any publication from the public portal for the purpose of private study or research. You may not further distribute the material or use it for any profit-making activity or commercial gain You may freely distribute the URL identifying the publication in the public portal If you believe that this document breaches copyright please contact us providing details, and we will -

Effect of Vitamin C on Bisphenol a Induced Hepato& Nephrotoxicity in Albino Rats
Haroun et al. 57 EFFECT OF VITAMIN C ON BISPHENOL A INDUCED HEPATO& NEPHROTOXICITY IN ALBINO RATS Marcelle R. Haroun,M.D.*, Ibrahim S. Zamzam, M.D.*,Eslam S. Metwally, M.D.*, and Rabab Sh. EL-Shafey, M.S.C. * *Forensic Medicine & Clinical Toxicology Department, Faculty of Medicine, Benha University, Egypt [email protected] [email protected] [email protected] [email protected] ABSTRACT Bisphenol-A (BPA) is a worldwide used endocrine disruptor that is incorporated in many plastic industries. The exposure of humans to that substance starts early during the fetal life. Many agencies raised warnings against the excessive use of such substances. The present study aimed to evaluate the oxidative stress effect of BPA on liver and kidney of albino rats, and whether co-administration of vitamin C can ameliorate this oxidative damage. Albino rats were divided into six groups: -ve control group,+ve control group,vitamin C (60mglkg) treated group, BPA treated group, BPA+ high dose of vitamin C (60mglkg) treated group, and BPA+ low dose of vitamin C (5.5mglkg) treated group The oxidative stress arising from BPA was evaluated in liver and kidney tissues. In addition, serum creatinine, uric acid levels, (AST) and (ALT) activities as markers of kidney and liver function were measured. Biochemical analysis revealed significant reduction in activities of enzymatic antioxidants in BPA treated group and BPA + vitamin C treated groups in high & low doses as compared to control group. In addition, there were significant increase in AST, ALT, uric acid, and creatinine levels in BPA treated group and reduction in their concentrations BPA + vitamin C treated groups in high & low doses as compared to control group. -
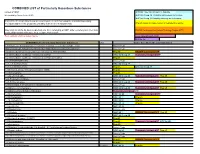
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -

Pesticides Reduce Symbiotic Efficiency of Nitrogen-Fixing Rhizobia and Host Plants
Pesticides reduce symbiotic efficiency of nitrogen-fixing rhizobia and host plants Jennifer E. Fox*†, Jay Gulledge‡, Erika Engelhaupt§, Matthew E. Burow†¶, and John A. McLachlan†ʈ *Center for Ecology and Evolutionary Biology, University of Oregon, 335 Pacific Hall, Eugene, OR 97403; †Center for Bioenvironmental Research, Environmental Endocrinology Laboratory, Tulane University, 1430 Tulane Avenue, New Orleans, LA 70112-2699; ‡Department of Biology, University of Louisville, Louisville, KY 40292 ; §University of Colorado, Boulder, CO 80309; and ¶Department of Medicine and Surgery, Hematology and Medical Oncology Section, Tulane University Medical School, 1430 Tulane Avenue, New Orleans, LA 70112-2699 Edited by Christopher B. Field, Carnegie Institution of Washington, Stanford, CA, and approved May 8, 2007 (received for review January 8, 2007) Unprecedented agricultural intensification and increased crop by plants, in rotation with non-N-fixing crops (8, 15). The yield will be necessary to feed the burgeoning world population, effectiveness of this strategy relies on maximizing symbiotic N whose global food demand is projected to double in the next 50 fixation (SNF) and plant yield to resupply organic and inorganic years. Although grain production has doubled in the past four N and nutrients to the soil. The vast majority of biologically fixed decades, largely because of the widespread use of synthetic N is attributable to symbioses between leguminous plants (soy- nitrogenous fertilizers, pesticides, and irrigation promoted by the bean, alfalfa, etc.) and species of Rhizobium bacteria; replacing ‘‘Green Revolution,’’ this rate of increased agricultural output is this natural fertilizer source with synthetic N fertilizer would cost unsustainable because of declining crop yields and environmental Ϸ$10 billion annually (16, 17). -
OECD Conceptual Framework for Testing and Assessment of Endocrine Disrupters As a Basis for Regulation of Substances with Endocrine Disrupting Properties
OECDOECD ConceptualConceptual FrameworkFramework for forTesting Testing and and Assessment Assessment of Endocrineof EndocrineDisrupters Disruptersas a basis asfor aregulation basis of forsubstances regulation with of substances endocrine disrupting with endocrineproperties disrupting properties Ulla Hass, Majken Dalgaard, Kirsten Jarfelt and Thuri S.A. Kledal Department of Toxicology and Risk Assessment, Danish Institute for Food and Veterinary Research, Denmark TemaNord 2004:555 OECD Conceptual Framework for Testing and Assessment of Endocrine Disrupters as a basis for regulation of substances with endocrine disrupting properties TemaNord 2004:555 © Nordic Council of Ministers, Copenhagen 2004 ISBN 92-893-1073-1 ISSN 0908-6692 Nordic Council of Ministers Nordic Council Store Strandstræde 18 Store Strandstræde 18 DK-1255 Copenhagen K DK-1255 Copenhagen K Phone (+45) 3396 0200 Phone (+45) 3396 0400 Fax (+45) 3396 0202 Fax (+45) 3311 1870 www.norden.org Nordic Environmental Co-operation Environmental co-operation is aimed at contributing to the improvement of the environment and forestall problems in the Nordic countries as well as on the international scene. The co- operation is conducted by the Nordic Committee of Senior Officials for Environmental Affairs. The co-operation endeavours to advance joint aims for Action Plans and joint projects, exchange of information and assistance, e.g. to Eastern Europe, through the Nordic Environmental Finance Corporation (NEFCO). The Nordic Council of Ministers was established in 1971. It submits proposals on co-operation between the governments of the five Nordic countries to the Nordic Council, implements the Council's recommendations and reports on results, while directing the work carried out in the targeted areas. The Prime Ministers of the five Nordic countries assume overall responsibility for the co-operation measures, which are co-ordinated by the ministers for co-operation and the Nordic Co-operation committee. -

In Vivo Exposure to Bisphenol-A Altered the Reproductive Functionality in Male Coturnix Coturnix Japonica
In Vivo Exposure to Bisphenol-A Altered the Reproductive Functionality in Male Coturnix Coturnix Japonica SUTHAN PERMUAL Central Avian Research Institute GAUTHAM KOLLURI ( [email protected] ) Central Avian Research Institute JAG MOHAN Central Avian Research Institute RAM SINGH Salim Ali Center for Ornithology and Natural History JAGBIR TYAGI Central Avian Research Institute Research Article Keywords: Bisphenol-A, quails, sperm quality, fertility Posted Date: December 21st, 2020 DOI: https://doi.org/10.21203/rs.3.rs-124102/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/21 Abstract Bisphenol-A, is one of the most characterized endocrine disruptors on the reproductive functions in humans and animals. We have previously reported in vitro and in vivo effects of bisphenol-A on functional role of sperm in chicken. Here, the effects of 1 and 5 mg/kg bisphenol-A daily administered by gavage for 3 wk to adult male Japanese quails on reproductive functionality was investigated. Cloacal index and foam frequency were greatly reduced at high dose. Sperm quality attributes were affected at both doses. Sperm quality attributes were affected at both doses. Alkaline phosphatase showed most signicant reduction among seminal enzymes. Dose dependent response (P < 0.01) of bisphenol-A was noticed with modulating testosterone concentrations at low and high doses. Disturbances regarding fertility and hatchability traits were prominent in high and low dose groups. The current study conrms the compromising actions of bisphenol-A on reproductive success in male Japanese quails at lower doses that are considered to be safe (50 mg/kg BW/d) under in vivo exposure module. -

Fighting Bisphenol A-Induced Male Infertility: the Power of Antioxidants
antioxidants Review Fighting Bisphenol A-Induced Male Infertility: The Power of Antioxidants Joana Santiago 1 , Joana V. Silva 1,2,3 , Manuel A. S. Santos 1 and Margarida Fardilha 1,* 1 Department of Medical Sciences, Institute of Biomedicine-iBiMED, University of Aveiro, 3810-193 Aveiro, Portugal; [email protected] (J.S.); [email protected] (J.V.S.); [email protected] (M.A.S.S.) 2 Institute for Innovation and Health Research (I3S), University of Porto, 4200-135 Porto, Portugal 3 Unit for Multidisciplinary Research in Biomedicine, Institute of Biomedical Sciences Abel Salazar, University of Porto, 4050-313 Porto, Portugal * Correspondence: [email protected]; Tel.: +351-234-247-240 Abstract: Bisphenol A (BPA), a well-known endocrine disruptor present in epoxy resins and poly- carbonate plastics, negatively disturbs the male reproductive system affecting male fertility. In vivo studies showed that BPA exposure has deleterious effects on spermatogenesis by disturbing the hypothalamic–pituitary–gonadal axis and inducing oxidative stress in testis. This compound seems to disrupt hormone signalling even at low concentrations, modifying the levels of inhibin B, oestra- diol, and testosterone. The adverse effects on seminal parameters are mainly supported by studies based on urinary BPA concentration, showing a negative association between BPA levels and sperm concentration, motility, and sperm DNA damage. Recent studies explored potential approaches to treat or prevent BPA-induced testicular toxicity and male infertility. Since the effect of BPA on testicular cells and spermatozoa is associated with an increased production of reactive oxygen species, most of the pharmacological approaches are based on the use of natural or synthetic antioxidants. -

Toxicological Evaluation of Bisphenol a and Its Analogues Bisfenol a Ve Analoglarının Toksikolojik Değerlendirilmesi
Turk J Pharm Sci 2020;17(4):457-462 DOI: 10.4274/tjps.galenos.2019.58219 REVIEW Toxicological Evaluation of Bisphenol A and Its Analogues Bisfenol A ve Analoglarının Toksikolojik Değerlendirilmesi İrem İYİGÜNDOĞDU1, Aylin ÜSTÜNDAĞ2*, Yalçın DUYDU2 1Gazi University Faculty of Pharmacy, Department of Toxicology, Ankara, Turkey 2Ankara University Faculty of Pharmacy, Department of Toxicology, Ankara, Turkey ABSTRACT Bisphenol A (BPA) is known as one of the oldest synthetic compounds with endocrine disrupting activity. It is commonly used in the production of epoxy resins, polycarbonates, dental fillings, food storage containers, baby bottles, and water containers. BPA is associated with various health problems such as obesity, diabetes, chronic respiratory diseases, cardiovascular diseases, renal diseases, behavior disorders, breast cancer, tooth development disorders, and reproductive disorders. Increasing health concerns have led the industry to seek alternatives to BPA. As BPA is now being excluded from several consumer products, the use of alternative compounds is increasing. However, the chemicals used to replace BPA are also BP analogues and may have similar or higher toxicological effects on organisms. The aim of this review is to focus on the toxicological profiles of different BP analogues (i.e. BPS and BPF) which are increasingly used today as alternative to BPA. Key words: Bisphenols, bisphenol A, endocrine disruptor, bisphenol S, bisphenol F ÖZ Bisfenol A (BPA) endokrin aktiviteye sahip bilinen en eski bileşiklerden biridir. BPA epoksi reçineler, polikarbonatlar, diş dolguları, yemek saklama kapları, bebek biberonları ve su bidonlarının üretiminde yaygın olarak kullanılmaktadır. BPA obezite, diyabet, kronik solunum hastalıkları, kardiyovasküler hastalıklar, renal hastalıklar, davranış bozuklukları, meme kanseri, diş gelişimi bozuklukları ve üreme bozuklukları gibi çeşitli sağlık sorunlarıyla ilişkilendirilmiştir. -

The Fates of Endocrine Disruptors in Consumer Products: Bisphenol A
The Fates of Endocrine Disruptors in Consumer Products: Bisphenol A Prepared by Dr. Matthew A. DeNardo for the One Health One Planet Conference on March 8, 2018 at Phipps Conservatory The Fates of Endocrine Disruptors in Consumer Products: Bisphenol A Prepared by Dr. Matthew A. DeNardo for the One Health One Planet Conference on March 8, 2017 at Phipps Conservatory The Fates of Endocrine Disruptors in Consumer Products: Bisphenol A Prepared by Dr. Matthew A. DeNardo for the One Health One Planet Conference on March 8, 2017 at Phipps Conservatory A multidisciplinary investigation of the technical and environmental performances of TAML/peroxide elimination of Bisphenol A compounds from water. Green Chemistry doi:10.1039/C7GC01415E The Fates of Endocrine Disruptors in Consumer Products: Bisphenol A Prepared by Dr. Matthew A. DeNardo for the One Health One Planet Conference on March 8, 2017 at Phipps Conservatory HO OH Bisphenol A HO OH Phenol Bisphenol A HO OH Phenol Phenol Bisphenol A A HO OH Phenol Phenol Bisphenol A A HO OH Phenol Phenol Bisphenol A + O H 1 + 2 + H2O HO Δ HO OH Acetone Phenol Bisphenol A Water A HO OH Phenol Phenol Bisphenol A + O H 1 + 2 + H2O HO Δ HO OH Acetone Phenol Bisphenol A Water + A HO OH Phenol Phenol Bisphenol A + O H 1 + 2 + H2O HO Δ HO OH Acetone Phenol Bisphenol A Water + Bhandari 2015 HO OH Bisphenol A HO OH Bisphenol A HO OH Bisphenol A HO OH Bisphenol A O NaOH Cl Cl (Sodium (Phosgene) HO Hydroxide) o H2O, 25 C Bisphenol A OH O Cl O O Cl NaOH (Phosgene) O O O O (Sodium o C Hydroxide)O, 25 Bisphenol A Polycarbonate -

Toxicological and Health Aspects of Bisphenol A
Toxicological and Health Aspects of Bisphenol A Report of Joint FAO/WHO Expert Meeting 2–5 November 2010 and Report of Stakeholder Meeting on Bisphenol A 1 November 2010 Ottawa, Canada Food and Agriculture Organization of the United Nations WHO Library Cataloguing-in-Publication Data Joint FAO/WHO expert meeting to review toxicological and health aspects of bisphenol A: final report, including report of stakeholder meeting on bisphenol A, 1-5 November 2010, Ottawa, Canada. 1.Phenols - toxicity. 2.Food contamination. 3.Food packing. I.World Health Organization. II.Food and Agriculture Organization of the United Nations. ISBN 978 92 14 156427 4 (NLM classification: QV 223) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. -

California Proposition 65 (Prop65)
20 NOVEMBER 2018 To Whom It May Concern: Certificate of Compliance California Proposition 65 California’s Proposition 65 entitles California consumers to special warnings for products that contain chemicals known to the state of California to cause cancer and birth defects or other reproductive harm if those products expose consumers to such chemicals above certain threshold levels. This is to certify that Alliance Memory comply with Safe Drinking Water and Toxic Enforcement Act of 1986, commonly known as California Proposition 65, that are ‘known to the state to cause cancer or reproductive toxicity’ as of December 29, 2017, by following the labelling guidelines set out therein. Alliance Memory labelling system clearly states a ‘Prop65 warning’ as and when necessary, on product packaging that is destined for the state of California, USA. This document certifies that to the best of our current knowledge and belief and under normal usage, Alliance Memory’s IC products are in compliance with California Proposition 65 – The Safe Drinking Water and Toxic Enforcement Act, 1986) and do not contain chemical elements of those listed within the California Proposition 65 chemical listing as shown below. Signature : Date: 20 November 2018 Name : Kim Bagby Title : Director QRA Department/Alliance Memory California Proposition 65 list of chemicals. The following is a list of chemicals published as a requirement of Safe Drinking Water and Toxic Enforcement Act of 1986, commonly known as California Proposition 65, that are ‘known to the state to cause -
STATE of the ART ASSESSMENT of ENDOCRINE DISRUPTERS Final Report
STATE OF THE ART ASSESSMENT OF ENDOCRINE DISRUPTERS Final Report Project Contract Number 070307/2009/550687/SER/D3 Authors: Andreas Kortenkamp, Olwenn Martin, Michael Faust, Richard Evans, Rebecca McKinlay, Frances Orton and Erika Rosivatz 23.12.2011 TABLE OF CONTENTS TABLE OF CONTENTS 0 EXECUTIVE SUMMARY ......................................................................................................................... 7 1 INTRODUCTION .................................................................................................................................... 9 1.1 TERMS OF REFERENCE, SCOPE OF THE REPORT ........................................................................... 9 1.2 STRUCTURE OF THE REPORT ....................................................................................................... 11 2 DEFINITION OF ENDOCRINE DISRUPTING CHEMICALS ...................................................................... 13 2.1 THE ENDOCRINE SYSTEM ............................................................................................................ 13 2.2 ADVERSITY ................................................................................................................................... 15 2.2.1 DEFINITION........................................................................................................................... 15 2.2.2 ASSAY REQUIREMENTS ........................................................................................................ 16 2.2.3 ECOTOXICOLOGICAL EFFECTS .............................................................................................