Txnip and the Gapdh-Siah1 Signalling Pathway in Diabetic Nephropathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
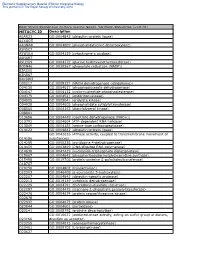
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Gene Symbol Gene Description ACVR1B Activin a Receptor, Type IB
Table S1. Kinase clones included in human kinase cDNA library for yeast two-hybrid screening Gene Symbol Gene Description ACVR1B activin A receptor, type IB ADCK2 aarF domain containing kinase 2 ADCK4 aarF domain containing kinase 4 AGK multiple substrate lipid kinase;MULK AK1 adenylate kinase 1 AK3 adenylate kinase 3 like 1 AK3L1 adenylate kinase 3 ALDH18A1 aldehyde dehydrogenase 18 family, member A1;ALDH18A1 ALK anaplastic lymphoma kinase (Ki-1) ALPK1 alpha-kinase 1 ALPK2 alpha-kinase 2 AMHR2 anti-Mullerian hormone receptor, type II ARAF v-raf murine sarcoma 3611 viral oncogene homolog 1 ARSG arylsulfatase G;ARSG AURKB aurora kinase B AURKC aurora kinase C BCKDK branched chain alpha-ketoacid dehydrogenase kinase BMPR1A bone morphogenetic protein receptor, type IA BMPR2 bone morphogenetic protein receptor, type II (serine/threonine kinase) BRAF v-raf murine sarcoma viral oncogene homolog B1 BRD3 bromodomain containing 3 BRD4 bromodomain containing 4 BTK Bruton agammaglobulinemia tyrosine kinase BUB1 BUB1 budding uninhibited by benzimidazoles 1 homolog (yeast) BUB1B BUB1 budding uninhibited by benzimidazoles 1 homolog beta (yeast) C9orf98 chromosome 9 open reading frame 98;C9orf98 CABC1 chaperone, ABC1 activity of bc1 complex like (S. pombe) CALM1 calmodulin 1 (phosphorylase kinase, delta) CALM2 calmodulin 2 (phosphorylase kinase, delta) CALM3 calmodulin 3 (phosphorylase kinase, delta) CAMK1 calcium/calmodulin-dependent protein kinase I CAMK2A calcium/calmodulin-dependent protein kinase (CaM kinase) II alpha CAMK2B calcium/calmodulin-dependent -

Synthesis and Evaluation of Chromone Derivatives As Inhibitors of Monoamine Oxidase
Synthesis and evaluation of chromone derivatives as inhibitors of monoamine oxidase AN Mpitimpiti 21253005 Dissertation submitted in fulfilment of the requirements for the degree Magister Scientiae in Pharmaceutical Chemistry at the Potchefstroom Campus of the North-West University Supervisor: Dr ACU Lourens Co-supervisors: Dr A Petzer Prof JP Petzer November 2014 The financial assistance of the National Research Foundation (NRF) and the Medical Research Council (MRC) towards this research is hereby acknowledged. Opinions expressed and conclusions arrived at are those of the author and are not necessarily to be attributed to the NRF or MRC. Acknowledgements • All glory be to God. • I am deeply indebted to the following for their immense support and contribution: o My supervisor - Dr A.C.U Lourens (your guidance is truly boundless). o My co-supervisors, Prof J.P Petzer and Dr A. Petzer. o Dr J.Jordaan. • My mother, Magret Chigeza (for your unconditional love and support). • My family and friends. • All those who knowingly and unknowingly supported me through out this journey. Psalm 115 verse 1: ‘Not to us, O Lord, not to us, but to Your Name be the glory, because of Your love and faithfulness’ i Table of Contents Abstract ...........................................................................................................................iv Opsomming ....................................................................................................................vii List of abbreviations .......................................................................................................xi -

Supplementary Materials
1 Supplementary Materials: Supplemental Figure 1. Gene expression profiles of kidneys in the Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice. (A) A heat map of microarray data show the genes that significantly changed up to 2 fold compared between Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice (N=4 mice per group; p<0.05). Data show in log2 (sample/wild-type). 2 Supplemental Figure 2. Sting signaling is essential for immuno-phenotypes of the Fcgr2b-/-lupus mice. (A-C) Flow cytometry analysis of splenocytes isolated from wild-type, Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice at the age of 6-7 months (N= 13-14 per group). Data shown in the percentage of (A) CD4+ ICOS+ cells, (B) B220+ I-Ab+ cells and (C) CD138+ cells. Data show as mean ± SEM (*p < 0.05, **p<0.01 and ***p<0.001). 3 Supplemental Figure 3. Phenotypes of Sting activated dendritic cells. (A) Representative of western blot analysis from immunoprecipitation with Sting of Fcgr2b-/- mice (N= 4). The band was shown in STING protein of activated BMDC with DMXAA at 0, 3 and 6 hr. and phosphorylation of STING at Ser357. (B) Mass spectra of phosphorylation of STING at Ser357 of activated BMDC from Fcgr2b-/- mice after stimulated with DMXAA for 3 hour and followed by immunoprecipitation with STING. (C) Sting-activated BMDC were co-cultured with LYN inhibitor PP2 and analyzed by flow cytometry, which showed the mean fluorescence intensity (MFI) of IAb expressing DC (N = 3 mice per group). 4 Supplemental Table 1. Lists of up and down of regulated proteins Accession No. -

Activation of Sphingosine Kinase 1 by ERK1/2Mediated Phosphorylation
The EMBO Journal Vol. 22 No. 20 pp. 5491±5500, 2003 Activation of sphingosine kinase 1 by ERK1/2-mediated phosphorylation Stuart M.Pitson1,2, Paul A.B.Moretti1, second messenger and a ligand for cell-surface receptors Julia R.Zebol1, Helen E.Lynn1, Pu Xia1,3, (Hla et al., 2001; Spiegel and Milstien, 2002). MathewA.Vadas 1,3 and The cellular levels of S1P are controlled by its Binks W.Wattenberg1,4 formation from sphingosine through the activity of sphingosine kinase, and by its degradation by S1P lyase 1Hanson Institute, Division of Human Immunology, Institute of (Van Veldhoven et al., 2000) and S1P phosphatases Medical and Veterinary Science, Frome Road, Adelaide, SA 5000 and (Mandala, 2001). In the basal state, this balance between 3Department of Medicine, Adelaide University, Frome Road, Adelaide, Australia S1P generation and degradation results in low cellular levels of S1P (Pyne and Pyne, 2000). However, when cells 4Present address: James Graham Brown Cancer Center, Dehlia Baxter Research Building, 580 S. Preston Avenue, Louisville, KY 40202, are exposed to speci®c growth factors and other agonists USA like tumour necrosis factor-a (TNFa) or phorbol esters the cellular levels of S1P can increase rapidly and transiently 2Corresponding author e-mail: [email protected] (Pitson et al., 2000b). This results in the triggering of various signalling pathways through as yet unidenti®ed Sphingosine kinase 1 is an agonist-activated signalling intracellular S1P targets, as well as through the engage- enzyme that catalyses the formation of sphingosine ment of cell surface S1P receptors following its release 1-phosphate, a lipid second messenger that has been from cells (Hobson et al., 2001). -

Bioenergetic Impairment in Congenital Muscular Dystrophy Type 1A And
www.nature.com/scientificreports OPEN Bioenergetic Impairment in Congenital Muscular Dystrophy Type 1A and Leigh Syndrome Received: 20 September 2016 Accepted: 23 February 2017 Muscle Cells Published: 03 April 2017 Cibely C. Fontes-Oliveira1, Maarten Steinz1, Peter Schneiderat2, Hindrik Mulder3 & Madeleine Durbeej1 Skeletal muscle has high energy requirement and alterations in metabolism are associated with pathological conditions causing muscle wasting and impaired regeneration. Congenital muscular dystrophy type 1A (MDC1A) is a severe muscle disorder caused by mutations in the LAMA2 gene. Leigh syndrome (LS) is a neurometabolic disease caused by mutations in genes related to mitochondrial function. Skeletal muscle is severely affected in both diseases and a common feature is muscle weakness that leads to hypotonia and respiratory problems. Here, we have investigated the bioenergetic profile in myogenic cells from MDC1A and LS patients. We found dysregulated expression of genes related to energy production, apoptosis and proteasome in myoblasts and myotubes. Moreover, impaired mitochondrial function and a compensatory upregulation of glycolysis were observed when monitored in real-time. Also, alterations in cell cycle populations in myoblasts and enhanced caspase-3 activity in myotubes were observed. Thus, we have for the first time demonstrated an impairment of the bioenergetic status in human MDC1A and LS muscle cells, which could contribute to cell cycle disturbance and increased apoptosis. Our findings suggest that skeletal muscle metabolism might be a promising pharmacological target in order to improve muscle function, energy efficiency and tissue maintenance of MDC1A and LS patients. Skeletal muscle is the largest organ in the human body and is used to respond to a broad range of functional demands in each animal species. -

Lipid Metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives
cancers Review Lipid metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives 1, 1, 1 2 1 Laurence Pellerin y, Lorry Carrié y , Carine Dufau , Laurence Nieto , Bruno Ségui , 1,3 1, , 1, , Thierry Levade , Joëlle Riond * z and Nathalie Andrieu-Abadie * z 1 Centre de Recherches en Cancérologie de Toulouse, Equipe Labellisée Fondation ARC, Université Fédérale de Toulouse Midi-Pyrénées, Université Toulouse III Paul-Sabatier, Inserm 1037, 2 avenue Hubert Curien, tgrCS 53717, 31037 Toulouse CEDEX 1, France; [email protected] (L.P.); [email protected] (L.C.); [email protected] (C.D.); [email protected] (B.S.); [email protected] (T.L.) 2 Institut de Pharmacologie et de Biologie Structurale, CNRS, Université Toulouse III Paul-Sabatier, UMR 5089, 205 Route de Narbonne, 31400 Toulouse, France; [email protected] 3 Laboratoire de Biochimie Métabolique, CHU Toulouse, 31059 Toulouse, France * Correspondence: [email protected] (J.R.); [email protected] (N.A.-A.); Tel.: +33-582-7416-20 (J.R.) These authors contributed equally to this work. y These authors jointly supervised this work. z Received: 15 September 2020; Accepted: 23 October 2020; Published: 27 October 2020 Simple Summary: Melanoma is a devastating skin cancer characterized by an impressive metabolic plasticity. Melanoma cells are able to adapt to the tumor microenvironment by using a variety of fuels that contribute to tumor growth and progression. In this review, the authors summarize the contribution of the lipid metabolic network in melanoma plasticity and aggressiveness, with a particular attention to specific lipid classes such as glycerophospholipids, sphingolipids, sterols and eicosanoids. -

Recent Research Developments in Parkinson's Disease
Page 12 to 30 Current Opinions in Neurological Science ISSN: 2575-5447 Review Article Volume 5 Issue 1 • 2020 Recent Research Developments in Parkinson’s Disease Alain L. Fymat Institute Professor, International Institute of Medicine & Science, California, U.S.A Received : February 09, 2020 Published : February 24, 2020 *Corresponding Author: Alain L. Fymat, Professor, International Institute of Medicine & Science, California, U.S.A Copyright © All rights are reserved by Alain L. Fymat. Abstract Important research developments have recently occurred in the understanding of Parkinson’s mechanisms and the symptomatic therapy of the disease. This article reviews such developments and their place in the disease’s therapeutic armamentarium. It also assesses their potential contribution(s) to our search for the root cause(s) of the disease. Improved symptomatic therapy has taken place for both motor and non-motor systems with the progressive development of several therapeutic drugs. This article also explores new research vistas including the role of gene therapy in the search for Parkinson’s disease-modifying therapy and neuroprotective treatments such as neural transplantation, stem cell transplantation, and transcranial magnetic stimulation. In this context, our two interacting brains (brain-in-the-skull, brain-in-the-gut) should underpin Braak’s hypothesis as to the origin of Parkinson’s. In the search for disease-modifying therapies, the article reviews the two therapeutic strategies currently followed, the correlation between a reduced occurrence or prevalence (or both) of PD and the consumption of compounds such as caffeine or nicotine. The three different principles of therapeutic action epidemiological findings and large clinical prospective trials reporting a are addressed: active and passive immunotherapy, modulation of alpha-synuclein aggregation, and enhancement of autophagy of alpha-synuclein. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
Building a Metabolic Bridge Between Glycolysis and Sphingolipid Biosynthesis : Implications in Cancer
University of Louisville ThinkIR: The University of Louisville's Institutional Repository Electronic Theses and Dissertations 8-2014 Building a metabolic bridge between glycolysis and sphingolipid biosynthesis : implications in cancer. Morgan L. Stathem University of Louisville Follow this and additional works at: https://ir.library.louisville.edu/etd Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Stathem, Morgan L., "Building a metabolic bridge between glycolysis and sphingolipid biosynthesis : implications in cancer." (2014). Electronic Theses and Dissertations. Paper 1374. https://doi.org/10.18297/etd/1374 This Master's Thesis is brought to you for free and open access by ThinkIR: The nivU ersity of Louisville's Institutional Repository. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of ThinkIR: The nivU ersity of Louisville's Institutional Repository. This title appears here courtesy of the author, who has retained all other copyrights. For more information, please contact [email protected]. BUILDING A METABOLIC BRIDGE BETWEEN GLYCOLYSIS AND SPHINGOLIPID BIOSYNTHESIS: IMPLICATIONS IN CANCER By Morgan L. Stathem B.S., University of Georgia, 2010 A Thesis Submitted to the Faculty of the School of Medicine of the University of Louisville In Partial Fulfillment of the Requirements for the Degree of Master of Science Department of Pharmacology and Toxicology University of Louisville Louisville, KY August 2014 BUILDING A METABOLIC BRIDGE BETWEEN GLYCOLYSIS AND SPHINGOLIPID BIOSYNTHESIS: IMPLICATIONS IN CANCER By Morgan L. Stathem B.S., University of Georgia, 2010 Thesis Approved on 08/07/2014 by the following Thesis Committee: __________________________________ Leah Siskind, Ph.D. __________________________________ Levi Beverly, Ph.D. -

Table of Contents
PI name: Carsten G. Bönnemann, MD Date: 01-Dec-2017 NIH Protocol number: 15-N-0018 NIH Version: 16 Santhera Protocol number: SNT-I-015 Santhera Version: 10 Congenital Muscular Dystrophy Ascending Multiple Dose Cohort Study anaLyzing Pharmacokinetics at three dose Levels In Children and Adolescents with Assessment of Safety and Tolerability of Omigapil (CALLISTO) Clinical Research Protocol Abbreviated Title: CALLISTO NIH Protocol Number: 15-N-0018 Santhera Protocol Number: SNT-I-015 Date of This Submission/Version (see header) IND Number: 113,370 Eudract Number: 2012-002700-40 Compound: Omigapil Hydrogen Maleate CRADA 2012-0097 (expiration 2020) Confidential Property of Santhera Pharmaceuticals (Switzerland) Ltd. 1 PI name: Carsten G. Bönnemann, MD Date: 01-Dec-2017 NIH Protocol number: 15-N-0018 NIH Version: 16 Santhera Protocol number: SNT-I-015 Santhera Version: 10 Synopsis Study Title Congenital Muscular Dystrophy Ascending Multiple Dose Cohort Study anaLyzing Pharmacokinetics at three dose Levels In Children and Adolescents with Assessment of Safety and Tolerability of Omigapil Study Number SNT-I-015 Study Phase 1 Study Acronym CALLISTO Planned Study Duration 84 weeks (16 weeks recruitment, 68 weeks study conduct). The above duration is assuming cohorts are dosed in staggered parallel. Patient participation will be up to 28 weeks (up to 4 weeks screening, 4 weeks run-in, 12 weeks treatment and a follow-up visit 8 weeks post last dose taken) Investigational Product Omigapil oral solution (0.1 and 0.25 mg/ml in Humco® Cherry Syrup) -

Targeting the Sphingosine Kinase/Sphingosine-1-Phosphate Signaling Axis in Drug Discovery for Cancer Therapy
cancers Review Targeting the Sphingosine Kinase/Sphingosine-1-Phosphate Signaling Axis in Drug Discovery for Cancer Therapy Preeti Gupta 1, Aaliya Taiyab 1 , Afzal Hussain 2, Mohamed F. Alajmi 2, Asimul Islam 1 and Md. Imtaiyaz Hassan 1,* 1 Centre for Interdisciplinary Research in Basic Sciences, Jamia Millia Islamia, Jamia Nagar, New Delhi 110025, India; [email protected] (P.G.); [email protected] (A.T.); [email protected] (A.I.) 2 Department of Pharmacognosy, College of Pharmacy, King Saud University, Riyadh 11451, Saudi Arabia; afi[email protected] (A.H.); [email protected] (M.F.A.) * Correspondence: [email protected] Simple Summary: Cancer is the prime cause of death globally. The altered stimulation of signaling pathways controlled by human kinases has often been observed in various human malignancies. The over-expression of SphK1 (a lipid kinase) and its metabolite S1P have been observed in various types of cancer and metabolic disorders, making it a potential therapeutic target. Here, we discuss the sphingolipid metabolism along with the critical enzymes involved in the pathway. The review provides comprehensive details of SphK isoforms, including their functional role, activation, and involvement in various human malignancies. An overview of different SphK inhibitors at different phases of clinical trials and can potentially be utilized as cancer therapeutics has also been reviewed. Citation: Gupta, P.; Taiyab, A.; Hussain, A.; Alajmi, M.F.; Islam, A.; Abstract: Sphingolipid metabolites have emerged as critical players in the regulation of various Hassan, M..I. Targeting the Sphingosine Kinase/Sphingosine- physiological processes. Ceramide and sphingosine induce cell growth arrest and apoptosis, whereas 1-Phosphate Signaling Axis in Drug sphingosine-1-phosphate (S1P) promotes cell proliferation and survival.