Cholesterol-Interacting Layered Phyllosilicates for Suppressing Gastrointestinal Cholesterol Absorption
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Joint Assessment Report Was Discussed by the Phvwp at Its Meeting in July 2007 and Finalised in September 2007
ASSESSMENT REPORT on the benefit:risk of fibrates EXECUTIVE SUMMARY 1. BACKGROUND In the light of the established role of statins in the primary and secondary prevention of cardiovascular disease (CVD) and safety concerns arising from the use of fibrates, the CHMP Pharmacovigilance Working Party (PhVWP) agreed to undertake a benefit:risk assessment of this class of medicines. The objective was to establish the current place of fibrates in the treatment of cardiovascular and dyslipidaemic diseases, and in diabetes mellitus; also to provide recommendations regarding amendments of the Summary of Product Characteristics (SPC), as necessary. Fibrates exert their effects mainly by activating the peroxisome proliferator-activated receptor-alpha (PPAR-alpha). Unique in this class, bezafibrate is an agonist for all three PPAR isoforms alpha, gamma, and delta. Fibrates have been shown to reduce plasma triglycerides by 30% to 50% and raise the level of high density lipoprotein cholesterol (HDL- C) by 2% to 20%. Their effect on low density lipoprotein cholesterol (LDL-C) is variable, ranging from no effect to a small decrease of the order of 10%. Today there are four licensed fibrates: bezafibrate, fenofibrate, gemfibrozil and ciprofibrate. Their currently approved indications are quite broad and in many cases still use the old Fredrickson classification for dyslipidaemias. 2. METHODOLOGY In February 2006 a List of Questions was agreed by the PhVWP for the Marketing Authorisation Holders (MAHs) of medicinal products containing one of the four currently licensed fibrates (Annex 1). Other clofibrate-containing medicinal products (e.g. etofibrate, etofyllinclofibrate) were excluded from this class review, since these are available only in a few member states via national marketing authorizations. -

PI Changes for Fibrates
Changes to Product Information as approved by the CHMP on 21 October 2010, pending endorsement by the European Commission 1 BEZAFIBRATE ANNEX I -SUMMARY OF PRODUCT CHARACTERISTICS 4.1 Therapeutic indications (to replace current text) [Product name] is indicated as an adjunct to diet and other non-pharmacological treatment (e.g. exercise, weight reduction) for the following: - Treatment of severe hypertriglyceridaemia with or without low HDL cholesterol. - Mixed hyperlipidaemia when a statin is contraindicated or not tolerated. 5.1 Pharmacodynamic properties (Additional text) There is evidence that treatment with fibrates may reduce coronary heart disease events but they have not been shown to decrease all cause mortality in the primary or secondary prevention of cardiovascular disease ANNEX III -LABELLING AND PACKAGE LEAFLET What [Product name] is and what it is used for [Product name] belongs to a group of medicines, commonly known as fibrates. These medicines are used to lower the level of fats (lipids) in the blood. For example the fats known as triglycerides. [Product name] is used, alongside a low fat diet and other non-medical treatments such as exercise and weight loss, to lower levels of fats in the blood. 2 CIPROFIBRATE ANNEX I -SUMMARY OF PRODUCT CHARACTERISTICS 4.1 Therapeutic indications (to replace current text) [Product name] is indicated as an adjunct to diet and other non-pharmacological treatment (e.g. exercise, weight reduction) for the following: - Treatment of severe hypertriglyceridaemia with or without low HDL cholesterol. - Mixed hyperlipidaemia when a statin is contraindicated or not tolerated. 5.1 Pharmacodynamic properties (Additional text) There is evidence that treatment with fibrates may reduce coronary heart disease events but they have not been shown to decrease all cause mortality in the primary or secondary prevention of cardiovascular disease ANNEX III -LABELLING AND PACKAGE LEAFLET What [Product name] is and what it is used for [Product name] belongs to a group of medicines, commonly known as fibrates. -

Fenofibrate, Bezafibrate, Ciprofibrate and Gemfibrozil Procedure Number
28 February 2011 EMA/CHMP/580013/2012 Assessment report for fenofibrate, bezafibrate, ciprofibrate, and gemfibrozil containing medicinal products pursuant to Article 31 of Directive 2001/83/EC, as amended INN: fenofibrate, bezafibrate, ciprofibrate and gemfibrozil Procedure number: EMEA/H/A-1238 Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. 7 Westferry Circus ● Canary Wharf ● London E14 4HB ● United Kingdom Telephone +44 (0)20 7418 8400 Facsimile +44 (0)20 7523 7051 E -mail [email protected] Website www.ema.europa.eu An agency of the European Union © European Medicines Agency, 2013. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 3 1.1. Referral of the matter to the CHMP ......................................................................... 3 2. Scientific discussion ................................................................................ 3 2.1. Introduction......................................................................................................... 3 2.2. Clinical aspects .................................................................................................... 4 2.2.1. PhVWP recommendation ..................................................................................... 4 2.2.2. CHMP review ..................................................................................................... 7 2.2.3. Discussion ..................................................................................................... -

Methods of Chromatographic Determination of Medicines Decreasing the Level of Cholesterol
Acta Poloniae Pharmaceutica ñ Drug Research, Vol. 67 No. 5 pp. 455ñ461, 2010 ISSN 0001-6837 Polish Pharmaceutical Society ANALYSIS METHODS OF CHROMATOGRAPHIC DETERMINATION OF MEDICINES DECREASING THE LEVEL OF CHOLESTEROL ELØBIETA KUBLIN1, BARBARA KACZMARSKA-GRACZYK1, EWA MALANOWICZ1 and ALEKSANDER P. MAZUREK1,2 1Department of Basic and Applied Pharmacy, National Medicines Institute, 30/34 Che≥mska St., 00-725 Warszawa, Poland 2Department of Drug Chemistry, Medical University of Warsaw, 1 Banacha St., 02- 097 Warszawa, Poland Abstract: With reference to common application of HPLC to routine analytical tests on medicinal products decreasing the level of cholesterol, including three compounds from this group ñ fenofibrate, bezafibrate and etofibrate, we developed a new method for determining two other compounds ñ ciprofibrate and gemfibrozil. The developed HPLC method may be used for identification and qualitative determination of selected com- pounds ñ derivatives of aryloxyalkylcarboxylic acids as well as it may be used for simultaneous separation and determination of all compounds from the group of fibrates using one column and the same methodology. The results and statistical data indicate good sensitivity and precision. The RSD value presented is equivalent to the newly developed method of determinination of ciprofibrate and gemfibrozil in the substances and medicinal products ñ capsules and coated tablets. Keywords: hyperlipidemia, HPLC, derivatives of aryloxyalkylcarboxylic acids, bezafibrate, ciprofibrate, fibrate, gemfibrozil, etofibrate, clofibrate Hyperlipidemia (HLP) is a group of disorders The selected medicines applied in the treat- in the lipid balance of various pathogenesis, which ment of hyperlipidemia, particularily leading to a demonstrate an increase in the cholesterol concen- decrease in the level of cholesterol, have been apart tration, mostly the level of lipoprotein fractions of from statins, the derivatives of aryloxyalkyl-car- low density (LDL) and/or the concentration of boxylic acids ñ so called fibrates. -

Update of Comparative Effectiveness of Lipid-Modifying Agents
Evidence-based Practice Center Systematic Review Protocol Project Title: Update of Comparative Effectiveness of Lipid-Modifying Agents I. Background and Objectives for the Systematic Review Epidemiology and Practice Guidelines Cardiovascular disease (CVD) affects 83.6 million Americans.1 CVD includes a variety of conditions such as myocardial infarction, stroke, heart failure, arrhythmia, heart valve disease, and hypertension. In 2009, CVD contributed to 32.3 percent of U.S. deaths and is a leading cause of disability.1 Atherosclerosis plays a major role in the development of certain cardiovascular diseases—coronary heart disease (CHD) including myocardial infarction, angina, and heart failure and cerebrovascular accident. These atherosclerotic diseases affect 15.4 million Americans.1 Elevated blood lipids are a major risk factor for atherosclerotic CVD. Abnormal lipoprotein metabolism predisposes individuals to atherosclerosis, especially increased concentrations of apolipoprotein B (apo B)-100–containing low-density lipoprotein (LDL-c). Oxidized LDL is atherogenic, causing endothelial damage, alteration of vascular tone, and recruitment of monocytes and macrophages. Many studies have underscored the importance of LDL-c in development of atherosclerotic CVD.2,3 Due to the consistent and robust association of higher LDL-c levels with atherosclerotic CVD across experimental and epidemiologic studies, therapeutic strategies to decrease risk have focused on LDL-c reduction as the primary goal. The trial results are most compelling regarding the reduction of CHD by lowering LDL-c. 4,5 Based on this evidence, the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) report established three CHD risk strata together with guidelines regarding the initiation of treatment and therapeutic targets based on LDL-c cutoffs. -

Anatomical Classification Guidelines V2020 EPHMRA ANATOMICAL
EPHMRA ANATOMICAL CLASSIFICATION GUIDELINES 2020 Anatomical Classification Guidelines V2020 "The Anatomical Classification of Pharmaceutical Products has been developed and maintained by the European Pharmaceutical Marketing Research Association (EphMRA) and is therefore the intellectual property of this Association. EphMRA's Classification Committee prepares the guidelines for this classification system and takes care for new entries, changes and improvements in consultation with the product's manufacturer. The contents of the Anatomical Classification of Pharmaceutical Products remain the copyright to EphMRA. Permission for use need not be sought and no fee is required. We would appreciate, however, the acknowledgement of EphMRA Copyright in publications etc. Users of this classification system should keep in mind that Pharmaceutical markets can be segmented according to numerous criteria." © EphMRA 2020 Anatomical Classification Guidelines V2020 CONTENTS PAGE INTRODUCTION A ALIMENTARY TRACT AND METABOLISM 1 B BLOOD AND BLOOD FORMING ORGANS 28 C CARDIOVASCULAR SYSTEM 35 D DERMATOLOGICALS 50 G GENITO-URINARY SYSTEM AND SEX HORMONES 57 H SYSTEMIC HORMONAL PREPARATIONS (EXCLUDING SEX HORMONES) 65 J GENERAL ANTI-INFECTIVES SYSTEMIC 69 K HOSPITAL SOLUTIONS 84 L ANTINEOPLASTIC AND IMMUNOMODULATING AGENTS 92 M MUSCULO-SKELETAL SYSTEM 102 N NERVOUS SYSTEM 107 P PARASITOLOGY 118 R RESPIRATORY SYSTEM 120 S SENSORY ORGANS 132 T DIAGNOSTIC AGENTS 139 V VARIOUS 141 Anatomical Classification Guidelines V2020 INTRODUCTION The Anatomical Classification was initiated in 1971 by EphMRA. It has been developed jointly by Intellus/PBIRG and EphMRA. It is a subjective method of grouping certain pharmaceutical products and does not represent any particular market, as would be the case with any other classification system. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Treatment Strategy for Dyslipidemia in Cardiovascular Disease Prevention: Focus on Old and New Drugs
pharmacy Article Treatment Strategy for Dyslipidemia in Cardiovascular Disease Prevention: Focus on Old and New Drugs Donatella Zodda 1,*, Rosario Giammona 2 and Silvia Schifilliti 2 1 Drug Department of Local Health Unit (ASP), Viale Giostra, 98168 Messina, Italy 2 Clinical Pharmacy Fellowship, University of Messina, Viale Annunziata, 98168 Messina, Italy; [email protected] (R.G.); silvia.schifi[email protected] (S.S.) * Correspondence: [email protected]; Tel.: +39-090-3653902 Received: 12 November 2017; Accepted: 11 January 2018; Published: 21 January 2018 Abstract: Prevention and treatment of dyslipidemia should be considered as an integral part of individual cardiovascular prevention interventions, which should be addressed primarily to those at higher risk who benefit most. To date, statins remain the first-choice therapy, as they have been shown to reduce the risk of major vascular events by lowering low-density lipoprotein cholesterol (LDL-C). However, due to adherence to statin therapy or statin resistance, many patients do not reach LDL-C target levels. Ezetimibe, fibrates, and nicotinic acid represent the second-choice drugs to be used in combination with statins if lipid targets cannot be reached. In addition, anti-PCSK9 drugs (evolocumab and alirocumab) provide an effective solution for patients with familial hypercholesterolemia (FH) and statin intolerance at very high cardiovascular risk. Recently, studies demonstrated the effects of two novel lipid-lowering agents (lomitapide and mipomersen) for the management of homozygous FH by decreasing LDL-C values and reducing cardiovascular events. However, the costs for these new therapies made the cost–effectiveness debate more complicated. Keywords: lipid lowering therapy; dyslipidemia; statins; fibrate; PCSK9 inhibitors; lomitapide 1. -

Use of Cholesterol-Lowering Medications of Patients with Myocardial Infarction from 2007-2015 in Cardiology Clinic to “Mother Teresa” University Hospital in Albania
Pharmacology & Pharmacy, 2016, 7, 236-245 Published Online June 2016 in SciRes. http://www.scirp.org/journal/pp http://dx.doi.org/10.4236/pp.2016.76030 Use of Cholesterol-Lowering Medications of Patients with Myocardial Infarction from 2007-2015 in Cardiology Clinic to “Mother Teresa” University Hospital in Albania Kleva Shpati1, Rudina Prifti1, Dritan Shpati2, Zana Bruci3, Erina Hilaj1 1Department of Pharmacy, Albanian University, Tirana, Albania 2Hospital Mbreteresha Geraldine, Tirana University, Tirana, Albania 3Faculty of Medicine, Tirana University, Tirana, Albania Received 29 September 2015; accepted 26 June 2016; published 29 June 2016 Copyright © 2016 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Background: Coronary Heart Disease (CHD) remains the leading cause of morbidity and mortality in Albania. According to Institute of Statistics of Albania (ISA), CHD remains in the 5 first places caused mortality and morbidity in our country. Currently, all the protocol treatments to Mother Teresa University Hospital (MTUH) are focused on low-density lipoprotein cholesterol (LDL-C) as the primary target for risk reduction therapy, followed by triglycerides (TG) and high-density lipoprotein cholesterol (HDL). Our clinicians recommend that the intensity and target goals of LDL-C-lowering therapy should be adjusted to individual treatment. The choice of a specific drug from anti hypercholesterolemia class depends on several factors which need to be evaluated better from our health providers. Methods and Findings: Data was collected between 2007 to 2015 at Mother Teresa University Hospital (MTUH), Intensive Care Unit in Cardiology Clinic. -

Review of Existing Classification Efforts
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.1.1 Review of existing classification efforts Due date of deliverable: (15.01.2008) Actual submission date: (07.02.2008) Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UGent Revision 1.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public X PP Restricted to other programme participants (including the Commission Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) Task 4.1 : Review of existing classification efforts Authors: Kristof Pil, Elke Raes, Thomas Van den Neste, An-Sofie Goessaert, Jolien Veramme, Alain Verstraete (Ghent University, Belgium) Partners: - F. Javier Alvarez (work package leader), M. Trinidad Gómez-Talegón, Inmaculada Fierro (University of Valladolid, Spain) - Monica Colas, Juan Carlos Gonzalez-Luque (DGT, Spain) - Han de Gier, Sylvia Hummel, Sholeh Mobaser (University of Groningen, the Netherlands) - Martina Albrecht, Michael Heiβing (Bundesanstalt für Straßenwesen, Germany) - Michel Mallaret, Charles Mercier-Guyon (University of Grenoble, Centre Regional de Pharmacovigilance, France) - Vassilis Papakostopoulos, Villy Portouli, Andriani Mousadakou (Centre for Research and Technology Hellas, Greece) DRUID 6th Framework Programme Deliverable D.4.1.1. Revision 1.0 Review of Existing Classification Efforts Page 2 of 127 Introduction DRUID work package 4 focusses on the classification and labeling of medicinal drugs according to their influence on driving performance. -
Study Protocol 1002-046 Amendment 1, 10 April 2017
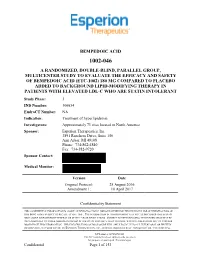
1. TITLE PAGE BEMPEDOIC ACID 1002-046 A RANDOMIZED, DOUBLE-BLIND, PARALLEL GROUP, MULTICENTER STUDY TO EVALUATE THE EFFICACY AND SAFETY OF BEMPEDOIC ACID (ETC-1002) 180 MG COMPARED TO PLACEBO ADDED TO BACKGROUND LIPID-MODIFYING THERAPY IN PATIENTS WITH ELEVATED LDL-C WHO ARE STATIN INTOLERANT Study Phase: 3 IND Number: 106654 EudraCT Number: NA Indication: Treatment of hyperlipidemia Investigators: Approximately 71 sites located in North America Sponsor: Esperion Therapeutics, Inc. 3891 Ranchero Drive, Suite 150 Ann Arbor, MI 48108 Phone: 734-862-4840 Fax: 734-582-9720 Sponsor Contact: Medical Monitor: Version Date Original Protocol: 25 August 2016 Amendment 1: 10 April 2017 Confidentiality Statement THIS CONFIDENTIAL INFORMATION IS ABOUT AN INVESTIGATIONAL DRUG PROVIDED FOR THE EXCLUSIVE USE OF INVESTIGATORS OF THIS DRUG AND IS SUBJECT TO RECALL AT ANY TIME. THE INFORMATION IN THIS DOCUMENT MAY NOT BE DISCLOSED UNLESS SUCH DISCLOSURE IS REQUIRED BY FEDERAL OR STATE LAW OR REGULATIONS. SUBJECT TO THE FOREGOING, THIS INFORMATION MAY BE DISCLOSED ONLY TO THOSE PERSONS INVOLVED IN THE STUDY WHO HAVE NEED TO KNOW, WITH THE OBLIGATION NOT TO FURTHER DISSEMINATE THIS INFORMATION. THESE RESTRICTIONS ON DISCLOSURE WILL APPLY EQUALLY TO ALL FUTURE ORAL OR WRITTEN INFORMATION, SUPPLIED TO YOU BY ESPERION THERAPEUTICS, INC., WHICH IS DESIGNATED AS “PRIVILEGED” OR “CONFIDENTIAL. NCT number: NCT02988115 This NCT number has been applied to the document for purposes of posting on clinicaltrials.gov Confidential Page 1 of 153 Bempedoic Acid Esperion Therapeutics, Inc. Clinical Study Protocol 1002-046 Amendment 1, 10 April 2017 2. SYNOPSIS Name of Sponsor: Esperion Therapeutics, Inc. -

Pharmaceuticals (Monocomponent Products) ………………………..………… 31 Pharmaceuticals (Combination and Group Products) ………………….……
DESA The Department of Economic and Social Affairs of the United Nations Secretariat is a vital interface between global and policies in the economic, social and environmental spheres and national action. The Department works in three main interlinked areas: (i) it compiles, generates and analyses a wide range of economic, social and environmental data and information on which States Members of the United Nations draw to review common problems and to take stock of policy options; (ii) it facilitates the negotiations of Member States in many intergovernmental bodies on joint courses of action to address ongoing or emerging global challenges; and (iii) it advises interested Governments on the ways and means of translating policy frameworks developed in United Nations conferences and summits into programmes at the country level and, through technical assistance, helps build national capacities. Note Symbols of United Nations documents are composed of the capital letters combined with figures. Mention of such a symbol indicates a reference to a United Nations document. Applications for the right to reproduce this work or parts thereof are welcomed and should be sent to the Secretary, United Nations Publications Board, United Nations Headquarters, New York, NY 10017, United States of America. Governments and governmental institutions may reproduce this work or parts thereof without permission, but are requested to inform the United Nations of such reproduction. UNITED NATIONS PUBLICATION Copyright @ United Nations, 2005 All rights reserved TABLE OF CONTENTS Introduction …………………………………………………………..……..……..….. 4 Alphabetical Listing of products ……..………………………………..….….…..….... 8 Classified Listing of products ………………………………………………………… 20 List of codes for countries, territories and areas ………………………...…….……… 30 PART I. REGULATORY INFORMATION Pharmaceuticals (monocomponent products) ………………………..………… 31 Pharmaceuticals (combination and group products) ………………….……........