Nuclear Phospholipase C &Beta
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Silencing of Phosphoinositide-Specific
ANTICANCER RESEARCH 34: 4069-4076 (2014) Silencing of Phosphoinositide-specific Phospholipase C ε Remodulates the Expression of the Phosphoinositide Signal Transduction Pathway in Human Osteosarcoma Cell Lines VINCENZA RITA LO VASCO1, MARTINA LEOPIZZI2, DANIELA STOPPOLONI3 and CARLO DELLA ROCCA2 Departments of 1Sense Organs , 2Medicine and Surgery Sciences and Biotechnologies and 3Biochemistry Sciences “A. Rossi Fanelli”, Sapienza University, Rome, Italy Abstract. Background: Ezrin, a member of the signal transduction pathway (5). The reduction of PIP2 ezrin–radixin–moesin family, is involved in the metastatic induces ezrin dissociation from the plasma membrane (6). spread of osteosarcoma. Ezrin binds phosphatydil inositol-4,5- The levels of PIP2 are regulated by the PI-specific bisphosphate (PIP2), a crucial molecule of the phospholipase C (PI-PLC) family (7), constituting thirteen phosphoinositide signal transduction pathway. PIP2 levels are enzymes divided into six sub-families on the basis of amino regulated by phosphoinositide-specific phospholipase C (PI- acid sequence, domain structure, mechanism of recruitment PLC) enzymes. PI-PLCε isoform, a well-characterized direct and tissue distribution (7-15). PI-PLCε, a direct effector of effector of rat sarcoma (RAS), is at a unique convergence RAS (14-15), might be the point of convergence for the point for the broad range of signaling pathways that promote broad range of signalling pathways that promote the RAS GTPase-mediated signalling. Materials and Methods. By RASGTPase-mediated signalling (16). using molecular biology methods and microscopic analyses, In previous studies, we suggested a relationship between we analyzed the expression of ezrin and PLC genes after PI-PLC expression and ezrin (17-18). -
Genetic Variants in PLCB4/PLCB1 As Susceptibility Loci for Coronary Artery
www.nature.com/scientificreports OPEN Genetic variants in PLCB4/PLCB1 as susceptibility loci for coronary artery aneurysm formation in Received: 27 March 2015 Accepted: 04 September 2015 Kawasaki disease in Han Chinese Published: 05 October 2015 in Taiwan Ying-Ju Lin1,2, Jeng-Sheng Chang3,4, Xiang Liu5, Hsinyi Tsang5, Wen-Kuei Chien6, Jin-Hua Chen6,7, Hsin-Yang Hsieh3,8, Kai-Chung Hsueh9, Yi-Tzone Shiao10, Ju-Pi Li2,11, Cheng-Wen Lin12, Chih-Ho Lai13, Jer-Yuarn Wu2,14, Chien-Hsiun Chen2,14, Jaung-Geng Lin2, Ting-Hsu Lin1, Chiu-Chu Liao1, Shao-Mei Huang1, Yu-Ching Lan15, Tsung-Jung Ho2, Wen-Miin Liang16, Yi-Chun Yeh16, Jung-Chun Lin17 & Fuu-Jen Tsai1,2,18 Kawasaki disease (KD) is an acute, inflammatory, and self-limited vasculitis affecting infants and young children. Coronary artery aneurysm (CAA) formation is the major complication of KD and the leading cause of acquired cardiovascular disease among children. To identify susceptible loci that might predispose patients with KD to CAA formation, a genome-wide association screen was performed in a Taiwanese KD cohort. Patients with both KD and CAA had longer fever duration and delayed intravenous immunoglobulin treatment time. After adjusting for these factors, 100 susceptibility loci were identified. Four genes were identified from a single cluster of 35 using the Ingenuity Pathway Analysis (IPA) Knowledge Base. Silencing KCNQ5, PLCB1, PLCB4, and PLCL1 inhibited the effect of lipopolysaccharide-induced endothelial cell inflammation with varying degrees of proinflammatory cytokine expression. PLCB1 showed the most significant inhibition. Endothelial cell inflammation was also inhibited by using a phospholipase C (PLC) inhibitor. -
A Meta-Analysis of Gene Expression Data Highlights Synaptic Dysfunction
www.nature.com/scientificreports OPEN A meta-analysis of gene expression data highlights synaptic dysfunction in the hippocampus of brains with Alzheimer’s disease Saeedeh Hosseinian1, Ehsan Arefan2,3 ✉ , Hassan Rakhsh-Khorshid4, Mehdi Eivani 5, Ameneh Rezayof6, Hamid Pezeshk 7,8 & Sayed-Amir Marashi 1 Since the world population is ageing, dementia is going to be a growing concern. Alzheimer’s disease is the most common form of dementia. The pathogenesis of Alzheimer’s disease is extensively studied, yet unknown remains. Therefore, we aimed to extract new knowledge from existing data. We analysed about 2700 upregulated genes and 2200 downregulated genes from three studies on the CA1 of the hippocampus of brains with Alzheimer’s disease. We found that only the calcium signalling pathway enriched by 48 downregulated genes was consistent between all three studies. We predicted miR-129 to target nine out of 48 genes. Then, we validated miR-129 to regulate six out of nine genes in HEK cells. We noticed that four out of six genes play a role in synaptic plasticity. Finally, we confrmed the upregulation of miR-129 in the hippocampus of brains of rats with scopolamine-induced amnesia as a model of Alzheimer’s disease. We suggest that future research should investigate the possible role of miR-129 in synaptic plasticity and Alzheimer’s disease. This paper presents a novel framework to gain insight into potential biomarkers and targets for diagnosis and treatment of diseases. Alzheimer’s disease (AD) is the most common form of dementia. It mostly afects people aged 65 and older, pro- gresses slowly and leads to death in an average of nine years afer diagnosis. -
Supplementary Data
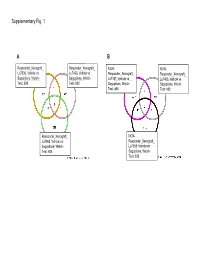
Supplementary Fig. 1 A B Responder_Xenograft_ Responder_Xenograft_ NON- NON- Lu7336, Vehicle vs Lu7466, Vehicle vs Responder_Xenograft_ Responder_Xenograft_ Sagopilone, Welch- Sagopilone, Welch- Lu7187, Vehicle vs Lu7406, Vehicle vs Test: 638 Test: 600 Sagopilone, Welch- Sagopilone, Welch- Test: 468 Test: 482 Responder_Xenograft_ NON- Lu7860, Vehicle vs Responder_Xenograft_ Sagopilone, Welch - Lu7558, Vehicle vs Test: 605 Sagopilone, Welch- Test: 333 Supplementary Fig. 2 Supplementary Fig. 3 Supplementary Figure S1. Venn diagrams comparing probe sets regulated by Sagopilone treatment (10mg/kg for 24h) between individual models (Welsh Test ellipse p-value<0.001 or 5-fold change). A Sagopilone responder models, B Sagopilone non-responder models. Supplementary Figure S2. Pathway analysis of genes regulated by Sagopilone treatment in responder xenograft models 24h after Sagopilone treatment by GeneGo Metacore; the most significant pathway map representing cell cycle/spindle assembly and chromosome separation is shown, genes upregulated by Sagopilone treatment are marked with red thermometers. Supplementary Figure S3. GeneGo Metacore pathway analysis of genes differentially expressed between Sagopilone Responder and Non-Responder models displaying –log(p-Values) of most significant pathway maps. Supplementary Tables Supplementary Table 1. Response and activity in 22 non-small-cell lung cancer (NSCLC) xenograft models after treatment with Sagopilone and other cytotoxic agents commonly used in the management of NSCLC Tumor Model Response type -

Supplementary Materials and Tables a and B
SUPPLEMENTARY MATERIAL 1 Table A. Main characteristics of the subset of 23 AML patients studied by high-density arrays (subset A) WBC BM blasts MYST3- MLL Age/Gender WHO / FAB subtype Karyotype FLT3-ITD NPM status (x109/L) (%) CREBBP status 1 51 / F M4 NA 21 78 + - G A 2 28 / M M4 t(8;16)(p11;p13) 8 92 + - G G 3 53 / F M4 t(8;16)(p11;p13) 27 96 + NA G NA 4 24 / M PML-RARα / M3 t(15;17) 5 90 - - G G 5 52 / M PML-RARα / M3 t(15;17) 1.5 75 - - G G 6 31 / F PML-RARα / M3 t(15;17) 3.2 89 - - G G 7 23 / M RUNX1-RUNX1T1 / M2 t(8;21) 38 34 - + ND G 8 52 / M RUNX1-RUNX1T1 / M2 t(8;21) 8 68 - - ND G 9 40 / M RUNX1-RUNX1T1 / M2 t(8;21) 5.1 54 - - ND G 10 63 / M CBFβ-MYH11 / M4 inv(16) 297 80 - - ND G 11 63 / M CBFβ-MYH11 / M4 inv(16) 7 74 - - ND G 12 59 / M CBFβ-MYH11 / M0 t(16;16) 108 94 - - ND G 13 41 / F MLLT3-MLL / M5 t(9;11) 51 90 - + G R 14 38 / F M5 46, XX 36 79 - + G G 15 76 / M M4 46 XY, der(10) 21 90 - - G NA 16 59 / M M4 NA 29 59 - - M G 17 26 / M M5 46, XY 295 92 - + G G 18 62 / F M5 NA 67 88 - + M A 19 47 / F M5 del(11q23) 17 78 - + M G 20 50 / F M5 46, XX 61 59 - + M G 21 28 / F M5 46, XX 132 90 - + G G 22 30 / F AML-MD / M5 46, XX 6 79 - + M G 23 64 / M AML-MD / M1 46, XY 17 83 - + M G WBC: white blood cell. -

Supplementary Table 1
Supplementary Table 1. 492 genes are unique to 0 h post-heat timepoint. The name, p-value, fold change, location and family of each gene are indicated. Genes were filtered for an absolute value log2 ration 1.5 and a significance value of p ≤ 0.05. Symbol p-value Log Gene Name Location Family Ratio ABCA13 1.87E-02 3.292 ATP-binding cassette, sub-family unknown transporter A (ABC1), member 13 ABCB1 1.93E-02 −1.819 ATP-binding cassette, sub-family Plasma transporter B (MDR/TAP), member 1 Membrane ABCC3 2.83E-02 2.016 ATP-binding cassette, sub-family Plasma transporter C (CFTR/MRP), member 3 Membrane ABHD6 7.79E-03 −2.717 abhydrolase domain containing 6 Cytoplasm enzyme ACAT1 4.10E-02 3.009 acetyl-CoA acetyltransferase 1 Cytoplasm enzyme ACBD4 2.66E-03 1.722 acyl-CoA binding domain unknown other containing 4 ACSL5 1.86E-02 −2.876 acyl-CoA synthetase long-chain Cytoplasm enzyme family member 5 ADAM23 3.33E-02 −3.008 ADAM metallopeptidase domain Plasma peptidase 23 Membrane ADAM29 5.58E-03 3.463 ADAM metallopeptidase domain Plasma peptidase 29 Membrane ADAMTS17 2.67E-04 3.051 ADAM metallopeptidase with Extracellular other thrombospondin type 1 motif, 17 Space ADCYAP1R1 1.20E-02 1.848 adenylate cyclase activating Plasma G-protein polypeptide 1 (pituitary) receptor Membrane coupled type I receptor ADH6 (includes 4.02E-02 −1.845 alcohol dehydrogenase 6 (class Cytoplasm enzyme EG:130) V) AHSA2 1.54E-04 −1.6 AHA1, activator of heat shock unknown other 90kDa protein ATPase homolog 2 (yeast) AK5 3.32E-02 1.658 adenylate kinase 5 Cytoplasm kinase AK7 -

Potent Lipolytic Activity of Lactoferrin in Mature Adipocytes
Biosci. Biotechnol. Biochem., 77 (3), 566–571, 2013 Potent Lipolytic Activity of Lactoferrin in Mature Adipocytes y Tomoji ONO,1;2; Chikako FUJISAKI,1 Yasuharu ISHIHARA,1 Keiko IKOMA,1;2 Satoru MORISHITA,1;3 Michiaki MURAKOSHI,1;4 Keikichi SUGIYAMA,1;5 Hisanori KATO,3 Kazuo MIYASHITA,6 Toshihide YOSHIDA,4;7 and Hoyoku NISHINO4;5 1Research and Development Headquarters, Lion Corporation, 100 Tajima, Odawara, Kanagawa 256-0811, Japan 2Department of Supramolecular Biology, Graduate School of Nanobioscience, Yokohama City University, 3-9 Fukuura, Kanazawa-ku, Yokohama, Kanagawa 236-0004, Japan 3Food for Life, Organization for Interdisciplinary Research Projects, The University of Tokyo, 1-1-1 Yayoi, Bunkyo-ku, Tokyo 113-8657, Japan 4Kyoto Prefectural University of Medicine, Kawaramachi-Hirokoji, Kamigyou-ku, Kyoto 602-8566, Japan 5Research Organization of Science and Engineering, Ritsumeikan University, 1-1-1 Nojihigashi, Kusatsu, Shiga 525-8577, Japan 6Department of Marine Bioresources Chemistry, Faculty of Fisheries Sciences, Hokkaido University, 3-1-1 Minatocho, Hakodate, Hokkaido 041-8611, Japan 7Kyoto City Hospital, 1-2 Higashi-takada-cho, Mibu, Nakagyou-ku, Kyoto 604-8845, Japan Received October 22, 2012; Accepted November 26, 2012; Online Publication, March 7, 2013 [doi:10.1271/bbb.120817] Lactoferrin (LF) is a multifunctional glycoprotein resistance, high blood pressure, and dyslipidemia. To found in mammalian milk. We have shown in a previous prevent progression of metabolic syndrome, lifestyle clinical study that enteric-coated bovine LF tablets habits must be improved to achieve a balance between decreased visceral fat accumulation. To address the energy intake and consumption. In addition, the use of underlying mechanism, we conducted in vitro studies specific food factors as helpful supplements is attracting and revealed the anti-adipogenic action of LF in pre- increasing attention. -

Identification of a Novel Binding Partner of Phospholipase Cb1: Translin-Associated Factor X
Identification of a Novel Binding Partner of Phospholipase Cb1: Translin-Associated Factor X Omozuanvbo R. Aisiku1, Loren W. Runnels2, Suzanne Scarlata1* 1 Department of Physiology and Biophysics, Stony Brook University, Stony Brook, New York, United States of America, 2 Department of Pharmacology, University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School, New Brunswick, New Jersey, United States of America Abstract Mammalian phospholipase Cb1 (PLCb1) is activated by the ubiquitous Gaq family of G proteins on the surface of the inner leaflet of plasma membrane where it catalyzes the hydrolysis of phosphatidylinositol 4,5 bisphosphate. In general, PLCb1is mainly localized on the cytosolic plasma membrane surface, although a substantial fraction is also found in the cytosol and, under some conditions, in the nucleus. The factors that localize PLCb1in these other compartments are unknown. Here, we identified a novel binding partner, translin-associated factor X (TRAX). TRAX is a cytosolic protein that can transit into the nucleus. In purified form, PLCb1 binds strongly to TRAX with an affinity that is only ten-fold weaker than its affinity for its functional partner, Gaq. In solution, TRAX has little effect on the membrane association or the catalytic activity of PLCb1. However, TRAX directly competes with Gaq for PLCb1 binding, and excess TRAX reverses Gaq activation of PLCb1. In C6 glia cells, endogenous PLCb1 and TRAX colocalize in the cytosol and the nucleus, but not on the plasma membrane where TRAX is absent. In Neuro2A cells expressing enhanced yellow and cyano fluorescent proteins (i.e., eYFP- PLCb1 and eCFP-TRAX), Fo¨rster resonance energy transfer (FRET) is observed mostly in the cytosol and a small amount is seen in the nucleus. -

Supplementary Table 2: Infection-Sensitive Genes
Supplementary Table 2: Infection-Sensitive Genes Supplementary Table 2: Upregulated with Adenoviral Infection (pages 1 - 7)- genes that were significant by ANOVA as well as significantly increased in control compared to both 'infected control' (Ad-LacZ) and 'calcineurin infected' (Ad-aCaN). Downregulated with Adenoviral Infection (pages 7 - 13) as above except for direction of change. Columns: Probe Set- Affymetrix probe set identifier for RG-U34A microarray, Symbol and Title- annotated information for above probe set (annotation downloaded June, 2004), ANOVA- p-value for 1-way Analysis of Variance, Uninfected, Ad-LacZ and Ad- aCaN- mean ± SEM expression for uninfected control, adenovirus mediated LacZ treated control, and adenovirus mediated calcineurin treated cultures respectively. Upregulated with Adenoviral Infection Probe Set Symbol Title ANOVA Uninfected Ad-LacZ Ad-aCaN Z48444cds_at Adam10 a disintegrin and metalloprotease domain 10 0.00001 837 ± 31 1107 ± 24 1028 ± 29 L26986_at Adcy8 adenylyl cyclase 8 0.00028 146 ± 12 252 ± 21 272 ± 21 U94340_at Adprt ADP-ribosyltransferase 1 0.00695 2096 ± 100 2783 ± 177 2586 ± 118 U01914_at Akap8 A kinase anchor protein 8 0.00080 993 ± 44 1194 ± 65 1316 ± 44 AB008538_at Alcam activated leukocyte cell adhesion molecule 0.01012 2775 ± 136 3580 ± 216 3429 ± 155 M34176_s_at Ap2b1 adaptor-related protein complex 2, beta 1 subunit 0.01389 2408 ± 199 2947 ± 143 3071 ± 116 D44495_s_at Apex1 apurinic/apyrimidinic endonuclease 1 0.00089 4959 ± 185 5816 ± 202 6057 ± 158 U16245_at Aqp5 aquaporin 5 0.02710 -

Differences in Metabolomic and Transcriptomic Profiles Between
Genes Nutr (2013) 8:411–423 DOI 10.1007/s12263-012-0328-0 RESEARCH PAPER Differences in metabolomic and transcriptomic profiles between responders and non-responders to an n-3 polyunsaturated fatty acids (PUFAs) supplementation Iwona Rudkowska • Ann-Marie Paradis • Elisabeth Thifault • Pierre Julien • Olivier Barbier • Patrick Couture • Simone Lemieux • Marie-Claude Vohl Received: 9 July 2012 / Accepted: 27 November 2012 / Published online: 19 December 2012 Ó Springer-Verlag Berlin Heidelberg 2012 Abstract Studies have demonstrated large within-popu- key genes in lipid metabolism: fatty acid desaturase 2, lation heterogeneity in plasma triacylglycerol (TG) phospholipase A2 group IVA, arachidonate 15-lipoxyge- response to n-3 PUFA supplementation. The objective of nase, phosphatidylethanolamine N-methyltransferase, the study was to compare metabolomic and transcriptomic monoglyceride lipase, and glycerol-3-phosphate acyl- profiles of responders and non-responders of an n-3 PUFA transferase, were expressed in opposing direction between supplementation. Thirty subjects completed a 2-week run- subgroups. In sum, results highlight key differences in lipid in period followed by a 6-week supplementation with n-3 metabolism of non-responders compared to responders PUFA (3 g/d). Six subjects did not lower their plasma TG after an n-3 PUFA supplementation, which may explain the (?9 %) levels (non-responders) and were matched to 6 inter-individual variability in plasma TG response. subjects who lowered TG (-41 %) concentrations (responders) after the n-3 PUFA supplementation. Pre-n-3 Keywords Lipidomics Á Metabolic pathways Á PUFA supplementation characteristics did not differ Metabolites Á Microarray Á Nutrigenomics between the non-responders and responders except for plasma glucose concentrations. -

Original Article Mir-423-5P Inhibits the Proliferation and Metastasis of Glioblastoma Cells by Targeting Phospholipase C Beta 1
Int J Clin Exp Pathol 2019;12(8):2941-2950 www.ijcep.com /ISSN:1936-2625/IJCEP0096628 Original Article miR-423-5p inhibits the proliferation and metastasis of glioblastoma cells by targeting phospholipase C beta 1 Peng Zhao1, Shukai Sun1, Yu’e Zhai1, Qingwu Tian1, Tingting Zhou1, Jing Li2 Departments of 1Clinical Laboratory, 2Nephrology, Affiliated Hospital of Qingdao University, Qingdao, China Received May 7, 2019; Accepted June 25, 2019; Epub August 1, 2019; Published August 15, 2019 Abstract: Glioma is a common brain tumor which is highly invasive, responds poorly to therapy, and has a poor prognosis. There is growing evidence that an abnormal expression of many genes is related to glioma and leads to glioma cell growth and metastasis. Phospholipase C beta 1 (PLCB1) plays critical roles in intracellular transduction and regulating signal activation, which are important to tumorigenesis. Therefore, it could bind to miRNA as a target gene. The purpose of our study was to confirm that PLCB1 plays a critical role in suppressing glioma progression. We found that the expression of miR-423-5p was reduced, but the expression of PLCB1 was increased, in glioma tissues and cells. To explore whether miR-423-5p affects PLCB1, a bioinformatics approach suggested that miR- 423-5p can directly target PLCB1. Moreover, we observed, using luciferase reporter assays, that miR-423-5p could target PLCB1 3’-UTR. Functionally, the overexpression of miR-423-5p could attenuate the proliferation, invasion, and migration and promote the apoptosis of glioma cells. Furthermore, we found that miR-423-5p could enhance p- ERK expression in glioma cells. -

Acetylcholine Induces Yeast to Hyphal Form Transition in Candida Albicans
mic eno s & G B l i a o g l o n g u y F Ali and Karuppayil, Fungal Genom Biol 2018, 8:1 Fungal Genomics & Biology DOI: 10.4172/2165-8056.1000154 ISSN: 2165-8056 Research Open Access Acetylcholine Induces Yeast to Hyphal Form Transition in Candida Albicans Ali A and Karuppayil SM* Former Director, School of Life Sciences, Swami Ramanand Teerth Marathwada University, India *Corresponding author:: Sankunny Mohan Karuppayil, Former Director, School of Life Sciences Swami Ramanand Teerth Marathwada University, India, Tel: +919764386253; E-mail:[email protected] Received date: March 12, 2018; Accepted date: March 28, 2018; Published date: April 04, 2018 Copyright: © 2018 Ali A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: In Candida Albicans, yeast to hyphal form transition can be induced by serum, proline, glucose, and N-acetyl glucosamine. Acetylcholine is a neuromodulator which can stimulate both muscarinic and nicotinic acetylcholine receptors in humans. In this study, we are reporting that acetylcholine can induce yeast to hyphal form transition in C. Albicans. The adenylyl cyclase inhibitor, MDL 12, 330A inhibited this transition indicating the role of cAMP. Muscarinic receptors in C. Albicans did not report yet. We have reported that C. Albicans Rrp9 exhibits identity and similarity with the human muscarinic receptor M1. In humans, activation of muscarinic M1 receptor can produce cAMP through inositol phosphate pathway. The inositol phosphate pathway in C.