Primary Care Priorities in East Lothian
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
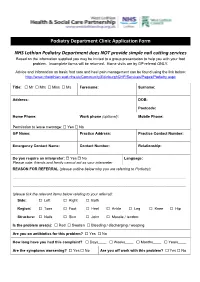
Podiatry Department Clinic Application Form NHS Lothian
Podiatry Department Clinic Application Form NHS Lothian Podiatry Department does NOT provide simple nail cutting services Based on the information supplied you may be invited to a group presentation to help you with your foot problem. Incomplete forms will be returned. Home visits are by GP referral ONLY. Advice and information on basic foot care and heel pain management can be found using the link below: http://www.nhslothian.scot.nhs.uk/Community/EdinburghCHP/Services/Pages/Podiatry.aspx Title: Mr Mrs Miss Ms Forename: Surname: Address: DOB: Postcode: Home Phone: Work phone (optional): Mobile Phone: Permission to leave message: Yes No GP Name: Practice Address: Practice Contact Number: Emergency Contact Name: Contact Number: Relationship: Do you require an interpreter: Yes No Language: Please note: friends and family cannot act as your interpreter REASON FOR REFERRAL (please outline below why you are referring to Podiatry): ......................................................................................................................................................................... ......................................................................................................................................................................... (please tick the relevant items below relating to your referral): Side: Left Right Both Region: Toes Foot Heel Ankle Leg Knee Hip Structure: Nails Skin Joint Muscle / tendon: Is the problem area(s): Red Swollen Bleeding / discharging / weeping Are you on -

NHS Lothian Sustainable Development Framework and Action Plan
In the face of climate change, the biggest threat to global health of the 21st century, we need to reassess and adapt to the challenge as an organisation and NHS Lothian as individuals within the organisation. Sustainable Development Framework and Action Plan This means understanding the impacts of climate change on health and illness, recognising that the NHS needs to be sustainable for future generations and Our Vision understanding the interdependence and opportunity of sustainability goals Our vision is to be a lead organisation in sustainable health care with all our such as those set out by the United Nations (UN). staff empowered to put sustainable healthcare at the heart of their practice. We will work with our partners and the communities we serve to put in place work practices, procurement systems and preventative interventions to minimise our environmental impact, protect the natural environment and enhance social value so that we are a sustainable service promoting good health and enhancing quality of life. Goals / strategic objectives 1. NHS Lothian will have zero carbon emissions by 2045 2. NHS Lothian will contribute to enhancing our natural environment 3. NHS Lothian will promote climate resilience and ensure that its services are The social, financial and environmental resources of the NHS are limited and adapted to climate change need to be used and managed sustainably. Environmental sustainability, good 4. NHS Lothian will ensure that sustainable development is embedded in all financial management and better, more equal health need to be driven forward its activities including governance and decision making, clinical practice, hand in hand. -

Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12
BOARD MEETING DATE: WEDNESDAY 4 FEBRUARY 2015 TIME: 9:30 A.M. - 12:00 P.M. VENUE: BOARDROOM, WAVERLEY GATE, 2-4 WATERLOO PLACE, EDINBURGH EH1 3EG Members are reminded that they should declare any financial and non-financial interests they have in the items of business for consideration, identifying the relevant agenda item and the nature of their interest. It is also a member’s duty under the Code of Conduct to ensure that any changes in circumstances are reported to the Corporate Services Manager within one month of them changing. AGENDA Agenda Lead Item Member Welcome to Members of the Public and the Press Apologies for Absence 1. Items for Approval 1.1. Minutes of the Board Meeting held on 3 December 2014 BH * 1.2. Minutes of the Special Board Meeting held on 14 January 2015 BH * 1.3. Running Action Note BH * 1.4. Performance Management AMcM * 1.5. Corporate Risk Register DF * 1.6. Committee Memberships BH * 1.7. Audit & Risk Committee - Minutes of 8 December 2014 JB * 1.8. Healthcare Governance Committee - Minutes of 25 November 2014 MB * 1.9. Finance & Resources Committee - Minutes of 12 November 2014 GW * 1.10. Strategic Planning Committee - Minutes of 13 November & 11 BH * December 2014 1.11. East Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12. Edinburgh Health & Social Care Partnership Shadow Board - RH * Minutes of 18 July 2014 1.13. Midlothian Health & Social Care Partnership Shadow Board Minutes PJ * of 23 October 2014 1.14. West Lothian Health & Care Partnership-Committee Sub - FT * Minutes of 18 December 2014 1.15. -

Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk www.nhslothian.scot.nhs.uk Date: 13/05/2020 Your Ref: Our Ref: 4385 Enquiries to : Richard Mutch Extension: 35687 Direct Line: 0131 465 5687 [email protected] [email protected] Dear FREEDOM OF INFORMATION – GP SYSTEMS I write in response to your request for information in relation to GP Systems within Lothian. I have been provided with information to help answer your request by the eHealth Department of NHS Lothian. Question: I would like to make a request for a list of GP practices within your health board area and the clinical system they use. Answer: Practice Clinical System Tyne Medical Practice ,Haddington- CEN Vision North Berwick Group Practice -CEN Vision The Orchard Medical Practice ,Haddington- CEN Vision Lammermuir Medical Practice, Haddington -CEN Vision Gullane MP - CEN Vision Whitesands Medical Practice,Dunbar-CEN Vision Lauderdale Medical Practice,Dunbar -CEN Vision Cromwell Harbour Medical Practice,Dunbar -CEN Vision East Linton EMIS Tranent MP - CEN Vision Prestonpans -CEN Vision The Riverside Medical Practice -CEN Vision Harbours Medical Practice -CEN Vision Inveresk Medical Practice -CEN Vision Ormiston MP-CEN Vision Craigmillar - CEN Vision GP Systems - May 2020 Durham Road -CEN Vision Baronscourt -CEN Vision Annandale Medical Practice,Bellevue MC- CEN Vision Hopetoun , Bellevue MC -CEN Vision Summerside -CEN Vision Victoria -CEN Vision Mill Lane -CEN Vision Southfield -

East Lothian Shifting the Balance of Care
East Lothian Shifting the Balance of Care Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Welcome Alison MacDonald Chief Officer East Lothian Health and Social Care Partnership Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Healthcare Vision Support Needed for Healthcare • Dunbar • Musselburgh • North Berwick • Tranent Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Community Hospital Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Consultation East Lothian IJB Strategic Plan 2019 – 2022 The Community View Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Andrew Milne Project Director NHS Lothian Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Considerations The Strategic Plan Service and Community Needs Multi Agency Working Capital Investment Property Transactions Governance and Funding Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act The Business Case Strategic Assessment - Submitted Initial Agreement Outline Business Case Full Business Case Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Governance Project Board Lothian Capital Investment Group Health and Social Care Partnership NHS Lothian Finances & Resources NHS Lothian Board Scottish Government Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Approach Feasibility -
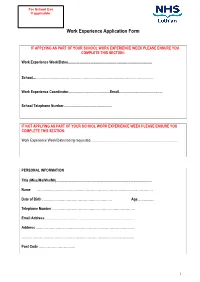
Work Experience Application Form
For School Use If applicable: Work Experience Application Form IF APPLYING AS PART OF YOUR SCHOOL WORK EXPERIENCE WEEK PLEASE ENSURE YOU COMPLETE THIS SECTION: Work Experience Week/Dates........................................................................................... School....……………………………………………………………………………………………. Work Experience Coordinator.............................................Email............................................... School Telephone Number.................................................... IF NOT APPLYING AS PART OF YOUR SCHOOL WORK EXPERIENCE WEEK PLEASE ENSURE YOU COMPLETE THIS SECTION: Work Experience Week/Dates being requested............................................................................................. PERSONAL INFORMATION Title (Miss/Ms/Mrs/Mr)....................................................................................................... Name …………………………………………………………………………………………… Date of Birth ……………………………………………………… Age.................. Telephone Number ………………………………………………………………… Email Address ……………………………………………………………………… Address ……………………………………………………………………………… ………………………………………………………………………………………… Post Code …………………………… 1 PLEASE INDICATE YOUR CHOSEN CAREER PATH …………………………………………………………………………………………. Please indicate your choice of placement and list your 1. preference in order (e.g. midwifery, cardiology) 2. 3. PLEASE INDICATE THE LOCATIONS YOU CAN CONSIDER Placement Location: using numbers (1 being your first choice, 2 being your second choice, etc) please mark all the areas that you could -

Closure of Belhaven Hospital Minor Injuries Unit RIA Jul 12
Audit Risk Level: High Rapid Impact Assessment summary report Each of the numbered sections below must be completed 1. Title of plan, policy or strategy being assessed. Closure of Minor Injuries Service, Belhaven Hospital, Dunbar 2. What will change as a result of this proposal? A recommendation will be made to East Lothian CHP sub committee to decommission the minor injuries service at Belhaven Hospital based on clinical governance and safety considerations. 3. Briefly describe public involvement in this proposal Through a series of meetings over several months, the Belhaven Hospital Forum, a constituency of local politicians, wide ranging community stakeholders, patients, health and social care representatives and clinicians have been involved in the planning and evolution of the proposal and have contributed thoughts and views which have been fundamental in shaping the recommendations. 4. Date of RIA 24 th July 2012 5. Who was present at the RIA? Identify facilitator and any partnership representative present Name Job Title Date of RIA Email training Carol Transformation [email protected] Lumsden and Integration Manager (Facilitator) [email protected] Thomas Partnership Miller Lead, East & Midlothian CHP [email protected] Sandra Glass Charge Nurse, Belhaven Hospital Gillian Wilson Public Partnership Forum, East Lothian CHP Steven Dunbar Bunyan Community Council 1 6. Population groups considered Potential differential impacts minority ethnic people (incl. No differential impact -

Annual Report and Accounts Year Ended 31St March 2019
Annual Report and Accounts Year ended 31st March 2019 NHS LOTHIAN ANNUAL REPORT AND ACCOUNTS FOR THE YEAR ENDED 31ST MARCH 2019 INDEX PAGE Annual Report 3 Section A: The Performance Report 3 1. Overview 3 2. Performance Analysis 14 Section B: The Accountability Report 31 Corporate Governance Report 31 - Directors report 31 - Statement of Health Board Members’ Responsibilities in respect of Accounts 32 - Statement of Chief Executive’s Responsibilities as the Accountable Officer of the Health Board 36 - The Governance Statement 37 Remuneration and Staff Report 46 Parliamentary Accountability Report 61 Independent Auditor’s Report 62 Accounts’ Primary Financial Statements 65 Notes to the Accounts 70 Accounts Direction 110 2 NHS LOTHIAN ANNUAL REPORT AND ACCOUNTS FOR THE YEAR ENDED 31ST MARCH 2019 ANNUAL REPORT SECTION A: THE PERFORMANCE REPORT 1. Overview This Overview aims to succinctly provide any reader with sufficient information to understand the NHS Board, its purpose, the key risks to the achievement of its objectives and how it has performed during the year. Should you wish to find out more detailed information we have provided this in the rest of the Performance Report, the Accountability Report and the financial statements. NHS Lothian routinely publishes a wide range of information on its services and activities on its website which you can find at: http://www.nhslothian.scot.nhs.uk/Pages/default.aspx Statement from the Chief Executive on the Performance of the NHS Board I would like to acknowledge the hard work of all of the Board’s staff, and thank them for all their efforts which allow us to continue to provide safe, effective, person-centred care. -

Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk Date: 30/12/2019 Our Ref: 4089 Enquiries to : Bryony Pillath Extension: 35676 Direct Line: 0131 465 5676 [email protected] Dear FREEDOM OF INFORMATION – CATERING I write in response to your request for information in relation to catering in NHS Lothian’s hospitals. Question: 1. What is the average cost per day in pound sterling allocated to feed an inpatient with non-exceptional dietary requirements staying in each of your hospitals for the last 5 years? For year please use calendar year up to 2019. For ‘hospitals’ please include sites where patients stay overnight on a ward and please ignore any sites that are self catering. Answer: Catering cost information is published for Scotland by the NHS National Services Scotland (NSS) Information Services Division (ISD) and can be found at the following weblinks: For 2019: https://www.isdscotland.org/Health-Topics/Finance/Costs/File-Listings-2019.asp For previous years: https://www.isdscotland.org/Health-Topics/Finance/Costs/costs- archive.asp Please click on the link, then download report R070-R110. Once the spreadsheet has opened look at tab R070. You can filter by health board; NHS Lothian is board code SSA20. Question: 2. Please list the hospital and care sites in your trust and state whether the catering service is outsourced and if outsourced please give the name of the company or companies this is currently outsourced to and the date of the outsourcing to this company. -

Review of Hospital-Based Complex Clinical Care NHS Lothian
Review of hospital-based complex clinical care NHS Lothian May 2016 Healthcare Improvement Scotland is committed to equality. We have assessed the inspection function for likely impact on equality protected characteristics as defined by age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation (Equality Act 2010). You can request a copy of the equality impact assessment report from the Healthcare Improvement Scotland Equality and Diversity Officer on 0141 225 6999 or email [email protected] © Healthcare Improvement Scotland 2016 First published May 2016 The publication is copyright to Healthcare Improvement Scotland. All or part of this publication may be reproduced, free of charge in any format or medium provided it is not for commercial gain. The text may not be changed and must be acknowledged as Healthcare Improvement Scotland copyright with the document’s date and title specified. Photographic images contained within this report cannot be reproduced without the permission of Healthcare Improvement Scotland. www.healthcareimprovementscotland.org Contents Executive summary 4 Context 5 About this review 7 Part 1: Hospital-based complex clinical care 8 Part 2: Governance, leadership and workforce 11 Part 3: Safe, person-centred and effective care 20 Part 4: Sustainability and capacity to improve 35 Appendix 1 – Recommendations 44 Appendix 2 – Review team and assurance group 47 Appendix 3 – Methodology 48 Review of hospital-based complex clinical care: NHS Lothian - May 2016 3 Executive summary Key messages • The NHS across Scotland is facing a number of challenges, due to an ageing population, particularly in areas providing care to patients with complex care needs. -

THE ROYAL EDINBURGH HOSPITAL a Guide for Patients, HOSPITAL Relatives and ROYAL EDINBURGH Carersthe ‘Publications’)
This booklet is on the NHS Lothian website at www.nhslothian.scot.nhs.uk (from the home page, click on ‘News and Publications’ and then THE EDINBURGH ROYAL HOSPITAL ‘Publications’). For a copy in , or your community Ref: 00541 The Royal Edinburgh Hospital, Guide for Patients, larger Relatives andprint, Carers Braille ARABIC THE ROYAL EDINBURGH HOSPITAL language, please call 0131 242 8181 and quote reference number 00541. A guide for patients, relatives and carers هﺬا اﻟﻜﺘﻴﺐ، ﻣﺴﺘﺸﻔﻰ أدﻧﺒﺮة اﻟﻤﻠﻜﻲ، ﻣﺮﺷﺪ ﻟﻠﻤﺮﺿﻰ، وأﻗﺎرﺑﻬﻢ، واﻟﻘﺎﺋﻤﻴﻦ ﻋﻠﻰ رﻋﺎﻳﺘﻬﻢ، ﻣﻮﺟﻮد ﻓﻲ ﻣﻮﻗﻊ اﻹﻧﺘﺮﻧﺖ اﻟﺨﺎص ﺑﺨﺪﻣﺔ اﻟﺼﺤﺔ اﻟﻮﻃﻨﻴﺔ (NHS) اﻟﻌﻨﻮان: www.nhslothian.scot.nhs.uk . ﻟﻠﺤﺼﻮل ﻋﻠﻰ ﻧﺴﺨﺔ ﻣﻦ اﻟﻜﺘﻴﺐ، ﻳﺮﺟﻰ اﻻﺗﺼﺎل هﺎﺗﻔﻴﺎً ﺑـﻮاﺳﻄﺔ اﻟﺮﻗﻢ:8181 242 0131 وذآﺮ رﻗﻢ اﻹﺷﺎرة 00541 ITS 00541-Simplified Chinese The Royal Edinburgh Hospital, a guide for patients, relatives and carers carers and relatives patients, for guide A www.nhslothian.scot.nhs.uk 00541নামক বকেলটিট এনএইচএস লািদয়ান এর ওেয়বসাইট এ পাওয় যােব বাংলায় এর একিট কিপ পাওয়ার জন দয় কের 0131 242 8181 এ ফান করেবন এবং রফাের নর 00541 উেখ করেবন ITS 00541-Traditional Chinese ࢷۤጛᏔཽܿĂ༫༫༫༫ၢĂᑍઐᑗᒎၢĂᑍઐᑗᒎ (The Royal EdinburghڐࢷۤጛᏔཽܿĂશଜڐቃݿᔇશଜ۾ቃݿᔇ۾ቃݿᔇ۾ Hospital, a guide for patients, relatives and carers) ᏲᏴ፞ਪਪۣॲᇗവᛇፎॊࠀ 00541 ༿༿༿༿ᒘ࢟ᒘ࢟ᒘ࢟ᒘ࢟۾ᎷჃནᒦᆪᆪ۾ăᎷჃནᒦᆪᆪ۾ࡼᆀᐶLjᆀᒍᆐ www.nhslothian.scot.nhs.ukăăăᎷჃནᒦᆪᆪ 00541ăăăܠ8181Lj݀༿ႁ߲ݬఠ 242 0131 ࢷۤጛᏔཽܿĂ༫ၢĂᑍઐᑗᒎ༫༫ၢĂᑍઐᑗᒎ (The Royal EdinburghڐࢷۤጛᏔཽܿĂ༫શଜڐቃݿᔇશଜ۾ቃݿᔇ۾ቃݿᔇ۾ Hospital, a guide for patients, relatives and carers) ᏲᏴ፞ਪਪۣॲᇗവᛇፎॊࠀ ༿༿༿༿ᒘ࢟ᒘ࢟ᒘ࢟ᒘ࢟۾ᎷჃནᒦᆪᆪ۾ăᎷჃནᒦᆪᆪ۾ࡼᆀᐶLjᆀᒍᆐ www.nhslothian.scot.nhs.ukăăăᎷჃནᒦᆪᆪ 00541. -

Prospect Bank Ward, Findlay House, 5 Seafield Street, Edinburgh, EH6 7LN
Mental Welfare Commission for Scotland Report on announced visit to: Prospect Bank Ward, Findlay House, 5 Seafield Street, Edinburgh, EH6 7LN Date of visit: 26 November 2018 Where we visited Prospect Bank is a 30-bed NHS continuing care ward for older adults with chronic and enduring mental health needs. The majority of patients on the ward have advanced dementia. Prospect Bank is one of two NHS continuing care wards that comprise Findlay House, a single-storey unit based on the former Eastern General Hospital site. The building is owned and managed by Robertson’s as part of a PFI initiative, with meals and laundry services provided by NHS Lothian. Prospect Bank is one of four national demonstrator sites currently participating in The Specialist Dementia Unit Improvement Programme, a Healthcare Improvement Scotland (HIS) initiative. Information on the project can be found at https://ihub.scot/improvement-programmes/focus-on-dementia/specialist-dementia- units/ We last visited this service on 7 July 2015, and made recommendations relating to increased activity provision, and for information relating to welfare proxies to be better documented in patient notes. On the day of this visit we wanted to meet with patients and visitors, follow up on the previous recommendations, and to find out more about the developments underway via the improvement pilot. Who we met with We met with and/or reviewed the care and treatment of eight patients and spoke with six carers, relatives, or friends. We met with the senior charge nurse, charge nurse, activities co-ordinator, and other members of the staff team.