Human Dissection Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study of Variation of Great Saphenous Veins and Its Surgical Significance (Original Study)
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 17, Issue 2 Ver. 10 February. (2018), PP 21-26 www.iosrjournals.org Study of Variation of Great Saphenous Veins and Its Surgical Significance (Original Study) Dr Surekha W. Meshram1, Dr. Yogesh Ganorkar2, Dr V.P. Rukhmode3, Dr. Tarkeshwar Golghate4 1(M.B.B.S,M.D) Associate Professor, Dept. of Anatomy Govt. Medical College Gondia, Maharashtra 2(M.B.B.S,M.D) Assistant Professor, Dept. of Anatomy Govt. Medical College Gondia, Maharashtra 3 (M.B.B.S, M.S) Professor and Head, Dept. of Anatomy Govt. Medical College Gondia, Maharashtra 4(M.B.B.S, M.D) Assiciate Professor, Dept. of Anatomy Govt. Medical College, Nagpur, Maharashtra Corresponding Author: Dr. Surekha W. Meshram Abstract Introduction: Veins of lower limbs are more involves for various venous disorders as compare to upper limbs. Most common venous disorders occurring in lower limbs are varicose veins, deep venous thrombosis and venous ulcers. Varicose veins are found in large population of world affecting both the males and females. Surgical operations are performed in all over the world to cure it. In the varicose vein surgery, surgeon successfully do the ligation as well as stripping of the great saphenous vein and its tributaries. Duplication of a great saphenous vein can be a potential cause for recurrent varicose veins after surgery as well as complications may occur during the surgery. Method: The present study was done by dissection method on 50 lower limbs of cadavers. Its aim was to identify the incidence and pattern of duplication of long saphenous vein in Indian population. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -
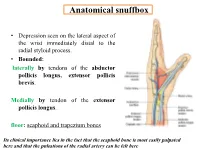
Anatomical Snuffbox
Anatomical snuffbox • Depression seen on the lateral aspect of the wrist immediately distal to the radial styloid process. • Bounded: laterally by tendons of the abductor pollicis longus, extensor pollicis brevis. Medially by tendon of the extensor pollicis longus. floor: scaphoid and trapezium bones Its clinical importance lies in the fact that the scaphoid bone is most easily palpated here and that the pulsations of the radial artery can be felt here Anatomical snuffbox Anatomical snuffbox • Contents: 2) Origin of the 1) The radial artery cephalic vein pass subcutaneously over the snuffbox. 3) Superficial branch of the radial nerve pass subcutaneously over the snuffbox. Blood supply of the hand Anastomoses occur between the radial and ulnar arteries via the superficial and deep palmar arches The Deep palmar arch is formed mainly by the radial artery while the superficial palmar arch is formed mainly by the ulnar artery 3-On entering the palm, it curves laterally behind (deep) the palmar 4-The arch is aponeurosis and in front completed on (superficial) of the long flexor the lateral side tendons forming by the the superficial palmar arch superficial branch of the radial artery. 2-Then it gives off its deep branch of which runs in front of the FR , and joins the radial artery to complete the deep palmar arch 1-Enters the hand anterior (superficial) to the Superficial flexor retinaculum palmar branch of radial artery through Guyon’s canal Radial artery 5-The superficial palmar arch gives off digital arteries from its convexity which pass to the fingers and supply them Superficial palmar arch Deep palmar branch of ulnar artery Superficial palmar branch of radial artery Ulnar artery Radial artery Radial Artery first dorsal interosseous muscle 1-From the floor of the anatomical snuff-box the radial artery leaves the dorsum of the hand by turning forward between the two heads of the first dorsal interosseous muscle. -

Brachium and Cubital Fossa
Anatomy Guy Dissection Sheet 1/15/2012 Brachium and Cubital Fossa Dr. Craig Goodmurphy Anatomy Guy Major Dissection Objectives – Anterior Compartment 1. Maintain the superficial veins but work the fascia of the brachium off the anterior compartment noting the intermuscular septae 2. Clean and identify the three muscle of the anterior arm and their attachments 3. Mobilize the contents of the brachial fascia as it extends from the axillary fascia to the elbow noting the median, ulnar and medial brachial and medial antebrachial cutaneous nerves 4. Follow the musculocutaneous nerve as it passes through the coracobrachialis and between the biceps and brachialis noting motor branches and the lateral antebrachial cutaneous nerve Major Dissection Objectives – Cubital Fossa & Posterior Compartment 6. Mobilize the cubital fossa veins and review the boundaries 7. Clean the biceps tendon and reflect the aponeurosis 8. Locate the contents of the fossa including the bifurcation of the brachial artery, median nerve and floor muscles 9. Have a partner elevate the arm to dissect posteriorly and remove the skin and fascia 10. Locate the three heads of the triceps and their attachments 11. Locate the profunda brachii artery and radial nerve at the triangular interval and between the brachialis and brachioradialis muscles Eastern Virginia Medical School 1 Anatomy Guy Dissection Sheet 1/15/2012 Brachium and Cubital Fossa Pearls & Problems Don’t 1. Cut the biceps muscle just mobilize it Do 2. Follow the cords and tubes from known to unknown as you clean them Do 3. Remove the duplicated deep veins but save the unpaired superficial veins Do 4. -

Elbow Checklist
Workbook Musculoskeletal Ultrasound September 26, 2013 Shoulder Checklist Long biceps tendon Patient position: Facing the examiner Shoulder in slight medial rotation; elbow in flexion and supination Plane/ region: Transverse (axial): from a) intraarticular portion to b) myotendinous junction (at level of the pectoralis major tendon). What you will see: Long head of the biceps tendon Supraspinatus tendon Transverse humeral ligament Subscapularis tendon Lesser tuberosity Greater tuberosity Short head of the biceps Long head of the biceps (musculotendinous junction) Humeral shaft Pectoralis major tendon Plane/ region: Logitudinal (sagittal): What you will see: Long head of biceps; fibrillar structure Lesser tuberosity Long head of the biceps tendon Notes: Subscapularis muscle and tendon Patient position: Facing the examiner Shoulder in lateral rotation; elbow in flexion/ supination Plane/ region: longitudinal (axial): full vertical width of tendon. What you will see: Subscapularis muscle, tendon, and insertion Supraspinatus tendon Coracoid process Deltoid Greater tuberosity Lesser tuberosity Notes: Do passive medial/ lateral rotation while examining Plane/ region: Transverse (sagittal): What you will see: Lesser tuberosity Fascicles of subscapularis tendon Supraspinatus tendon Patient position: Lateral to examiner Shoulder in extension and medial rotation Hand on ipsilateral buttock Plane/ region: Longitudinal (oblique sagittal) Identify the intra-articular portion of biceps LH in the transverse plane; then -

The Square Flap Technique for Burn Contractures: Clinical Experience and Analysis of Length Gain
Annals of Burns and Fire Disasters - vol. XXXI - n. 4 - December 2018 THE SQUARE FLAP TECHNIQUE FOR BURN CONTRACTURES: CLINICAL EXPERIENCE AND ANALYSIS OF LENGTH GAIN DOUBLE LAMBEAU RHOMBOÏDE POUR BRIDE SÉQUELLAIRE DE BRÛ- LURE: EXPÉRIENCE PRATIQUE ET ANALYSE DE LA LONGUEUR GAGNÉE Hifny M.A. Department of Plastic Surgery, Faculty of Medicine, Qena University Hospital, South Valley University, Egypt SUMMARY. Post-burn contractures, affecting the joints especially, are demanding problems. Many surgical techniques have been designated for burn contracture release. The aim of this study is to investigate the efficiency of the square flap technique to release a post-burn scar contracture, and assess the post-operative length gain that can be achieved by simple mathematical calculation. In this study, sixteen patients with linear contracture bands were treated with the square flap tech- nique. The anatomical distribution of the contractures was: axilla, cubital fossa, flank, perineum and popliteal fossa. Scar maturity ranged from 4 months - 9 years. Square flap width and contracture band length before and immediately after surgery were recorded by simple mathematical calculation. Flap complication was assessed. Patient satisfaction was also assessed during the follow-up period. All square flaps were effective in lengthening the contracture bands. The length of the contracture that was released ranged from 2 to 6 cm. The gain in length provided with this technique ranged from 212 to 350%, average 247%, and adequate contracture release was achieved in all cases postoperatively. All square flaps healed uneventfully except for one (6%), which demonstrated limited epidermolysis that healed by secondary intention. The fol- low-up interval ranged from 6 months to 1.5 years. -

Distal Radial Approach Through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention
Korean Circ J. 2018 Dec;48(12):1131-1134 https://doi.org/10.4070/kcj.2018.0293 pISSN 1738-5520·eISSN 1738-5555 Editorial Distal Radial Approach through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention Jae-Hyung Roh, MD, PhD, and Jae-Hwan Lee , MD, PhD Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea ► See the article “Feasibility of Coronary Angiography and Percutaneous Coronary Intervention via Left Snuffbox Approach” in volume 48 on page 1120. Received: Aug 27, 2018 The anatomical snuffbox, also known as the radial fossa, is a triangular-shaped depression Accepted: Sep 17, 2018 on the radial, dorsal aspect of the hand at the level of the carpal bones. It is clearly observed Figure 1 1)2) Correspondence to when the thumb is extended ( ). The bottom of the snuffbox is supported by carpal Jae-Hwan Lee, MD, PhD bones composed of the scaphoid and trapezium. The medial and lateral borders are bounded Division of Cardiology, Department of Internal by tendons of the extensor pollicis longus and the extensor pollicis brevis, respectively. The Medicine, Chungnam National University proximal border is formed by the styloid process of the radius. Within this narrow triangular Hospital, Chungnam National University space, various structures are located, including the distal radial artery (RA), a branch of the School of Medicine, 282, Munhwa-ro, Jung-gu, radial nerve, and the cephalic vein. Daejeon 35015, Korea. E-mail: [email protected] The anatomy of the hand arteries is illustrated in Figure 2. -

Ultrasound-Guided Access of the Distal Radial Artery at the Anatomical Snuffbox for Catheter-Based Vascular Interventions: a Technical Guide
Title: Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. Authors: Anastasia Hadjivassiliou, MBBS, BSc; Ferdinand Kiemeneij, M.D, PhD; Sandeep Nathan, M.D, MSc; Darren Klass, M.D, PhD DOI: 10.4244/EIJ-D-19-00555 Citation: Hadjivassiliou A, Kiemeneij F, Nathan S, Klass D. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. EuroIntervention 2019; Jaa-625 2019, doi: 10.4244/EIJ-D-19-00555 Manuscript submission date: 10 June 2019 Revisions received: 24 July 2019 Accepted date: 01 August 2019 Online publication date: 06 August 2019 Disclaimer: This is a PDF file of a "Just accepted article". This PDF has been published online early without copy editing/typesetting as a service to the Journal's readership (having early access to this data). Copy editing/typesetting will commence shortly. Unforeseen errors may arise during the proofing process and as such Europa Digital & Publishing exercise their legal rights concerning these potential circumstances. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide Anastasia Hadjivassiliou, MBBS, BSc1; Ferdinand Kiemeneij, MD, PhD2; Sandeep Nathan, MD, MSc3; Darren Klass, MD, PhD1 1. Department of Interventional Radiology, Vancouver General Hospital, University of British Columbia, Canada 2. Department of Cardiology, Tergooi Hospital, Blaricum, the Netherlands 3. University of Chicago Medicine, Chicago, IL, USA Short title: Ultrasound guided distal radial artery access at the anatomical snuffbox Corresponding author: Dr Darren Klass Department of Radiology, Vancouver General Hospital 899 West 12th Avenue, V5Z 1M9, Vancouver, BC, Canada Email address: [email protected] Disclaimer : As a public service to our readership, this article -- peer reviewed by the Editors of EuroIntervention - has been published immediately upon acceptance as it was received. -

Unusual Cubital Fossa Anatomy – Case Report
Anatomy Journal of Africa 2 (1): 80-83 (2013) Case Report UNUSUAL CUBITAL FOSSA ANATOMY – CASE REPORT Surekha D Shetty, Satheesha Nayak B, Naveen Kumar, Anitha Guru. Correspondence: Dr. Satheesha Nayak B, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State, India. 576104 Email: [email protected] SUMMARY The median nerve is known to show variations in its origin, course, relations and distribution. But in almost all cases it passes through the cubital fossa. We saw a cubital fossa without a median nerve. The median nerve had a normal course in the upper part of front of the arm but in the distal third of the arm it passed in front of the medial epicondyle of humerus, surrounded by fleshy fibres of pronator teres muscle. Its course and distribution in the forearm was normal. In the same limb, the fleshy fibres of the brachialis muscle directly continued into the forearm as brachioradialis, there being no fibrous septum separating the two muscles from each other. The close relationship of the nerve to the epicondyle might make it vulnerable in the fractures of the epicondyle. The muscle fibres surrounding the nerve might pull up on the nerve and result in altered sensory-motor functions of the hand. Since the brachialis and brachioradialis are two muscles supplied by two different nerves, this continuity of the muscles might result in compression/entrapment of the radial nerve in it. Key words: Median nerve, cubital fossa, brachialis, brachioradialis, entrapment INTRODUCTION The median nerve is the main content of and broad tendon which is inserted into the cubital fossa along with brachial artery and ulnar tuberosity and to a rough surface on the biceps brachii tendon. -

Carpal Box and Open Cup Radiography
.............................................................................................................. ON THE JOB Carpal Box and Open Cup Radiography Dan L. Hobbs, M.S.R.S., Scaphoid fractures of the wrist are will include a discussion of the blood R.T.(R)(CT)(MR), is an asso- common and account for 71% of all car- supply to this bone. Next, there will be ciate professor in the depart- pal bone fractures. In the United States, a brief discussion of the mechanism of ment of radiographic science approximately 345 000 new scaphoid frac- injury, and the article will conclude with at Idaho State University in tures occur each year.1 Additionally, sta- a review of 3 positioning techniques that Pocatello. tistics have shown that scaphoid fractures can be employed to help diagnose scaph- account for 2% to 7% of all orthopedic oid fractures. Acknowledgement: Joshua fractures; they are the most commonly Howard , a student in the undiagnosed fracture.2 If an undiag- Anatomy radiographic science program nosed fracture is left without proper The scaphoid is located on the radial at Idaho State University, con- immobilization, a portion of the scaphoid side of the wrist in the anatomical snuff tributed valuable research to may die; therefore, it is imperative that box, which is located between the extensor this article. proper diagnosis, radiographic evalua- pollicis brevis and extensor pollicis longus tion and therapeutic treatment begin as tendons. (See Fig. 1.) It is the largest bone soon as possible. in the proximal row of carpals and can be The purpose of this article is to described as being complex because of its acquaint the radiographer with a few non- twisted shape; some describe it as being traditional methods used to image this boat-shaped.3 It articulates with the radius, fracture. -

Lower Limb Venous Drainage
Vascular Anatomy of Lower Limb Dr. Gitanjali Khorwal Arteries of Lower Limb Medial and Lateral malleolar arteries Lower Limb Venous Drainage Superficial veins : Great Saphenous Vein and Short Saphenous Vein Deep veins: Tibial, Peroneal, Popliteal, Femoral veins Perforators: Blood flow deep veins in the sole superficial veins in the dorsum But In leg and thigh from superficial to deep veins. Factors helping venous return • Negative intra-thoracic pressure. • Transmitted pulsations from adjacent arteries. • Valves maintain uni-directional flow. • Valves in perforating veins prevent reflux into low pressure superficial veins. • Calf Pump—Peripheral Heart. • Vis-a –tergo produced by contraction of heart. • Suction action of diaphragm during inspiration. Dorsal venous arch of Foot • It lies in the subcutaneous tissue over the heads of metatarsals with convexity directed distally. • It is formed by union of 4 dorsal metatarsal veins. Each dorsal metatarsal vein recieves blood in the clefts from • dorsal digital veins. • and proximal and distal perforating veins conveying blood from plantar surface of sole. Great saphenous Vein Begins from the medial side of dorsal venous arch. Supplemented by medial marginal vein Ascends 2.5 cm anterior to medial malleolus. Passes posterior to medial border of patella. Ascends along medial thigh. Penetrates deep fascia of femoral triangle: Pierces the Cribriform fascia. Saphenous opening. Drains into femoral vein. superficial epigastric v. superficial circumflex iliac v. superficial ext. pudendal v. posteromedial vein anterolateral vein GREAT SAPHENOUS VEIN anterior leg vein posterior arch vein dorsal venous arch medial marginal vein Thoraco-epigastric vein Deep external pudendal v. Tributaries of Great Saphenous vein Tributaries of Great Saphenous vein saphenous opening superficial epigastric superficial circumflex iliac superficial external pudendal posteromedial vein anterolateral vein adductor c. -

DEPARTMENT of ANATOMY IGMC SHIMLA Competency Based Under
DEPARTMENT OF ANATOMY IGMC SHIMLA Competency Based Under Graduate Curriculum - 2019 Number COMPETENCY Objective The student should be able to At the end of the session student should know AN1.1 Demonstrate normal anatomical position, various a) Define and demonstrate various positions and planes planes, relation, comparison, laterality & b) Anatomical terms used for lower trunk, limbs, joint movement in our body movements, bony features, blood vessels, nerves, fascia, muscles and clinical anatomy AN1.2 Describe composition of bone and bone marrow a) Various classifications of bones b) Structure of bone AN2.1 Describe parts, blood and nerve supply of a long bone a) Parts of young bone b) Types of epiphysis c) Blood supply of bone d) Nerve supply of bone AN2.2 Enumerate laws of ossification a) Development and ossification of bones with laws of ossification b) Medico legal and anthropological aspects of bones AN2.3 Enumerate special features of a sesamoid bone a) Enumerate various sesamoid bones with their features and functions AN2.4 Describe various types of cartilage with its structure & a) Differences between bones and cartilage distribution in body b) Characteristics features of cartilage c) Types of cartilage and their distribution in body AN2.5 Describe various joints with subtypes and examples a) Various classification of joints b) Features and different types of fibrous joints with examples c) Features of primary and secondary cartilaginous joints d) Different types of synovial joints e) Structure and function of typical synovial