Hand Surgery: a Guide for Medical Students
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brachial-Plexopathy.Pdf
Brachial Plexopathy, an overview Learning Objectives: The brachial plexus is the network of nerves that originate from cervical and upper thoracic nerve roots and eventually terminate as the named nerves that innervate the muscles and skin of the arm. Brachial plexopathies are not common in most practices, but a detailed knowledge of this plexus is important for distinguishing between brachial plexopathies, radiculopathies and mononeuropathies. It is impossible to write a paper on brachial plexopathies without addressing cervical radiculopathies and root avulsions as well. In this paper will review brachial plexus anatomy, clinical features of brachial plexopathies, differential diagnosis, specific nerve conduction techniques, appropriate protocols and case studies. The reader will gain insight to this uncommon nerve problem as well as the importance of the nerve conduction studies used to confirm the diagnosis of plexopathies. Anatomy of the Brachial Plexus: To assess the brachial plexus by localizing the lesion at the correct level, as well as the severity of the injury requires knowledge of the anatomy. An injury involves any condition that impairs the function of the brachial plexus. The plexus is derived of five roots, three trunks, two divisions, three cords, and five branches/nerves. Spinal roots join to form the spinal nerve. There are dorsal and ventral roots that emerge and carry motor and sensory fibers. Motor (efferent) carries messages from the brain and spinal cord to the peripheral nerves. This Dorsal Root Sensory (afferent) carries messages from the peripheral to the Ganglion is why spinal cord or both. A small ganglion containing cell bodies of sensory NCS’s sensory fibers lies on each posterior root. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -
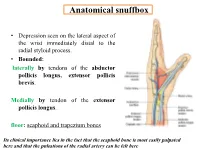
Anatomical Snuffbox
Anatomical snuffbox • Depression seen on the lateral aspect of the wrist immediately distal to the radial styloid process. • Bounded: laterally by tendons of the abductor pollicis longus, extensor pollicis brevis. Medially by tendon of the extensor pollicis longus. floor: scaphoid and trapezium bones Its clinical importance lies in the fact that the scaphoid bone is most easily palpated here and that the pulsations of the radial artery can be felt here Anatomical snuffbox Anatomical snuffbox • Contents: 2) Origin of the 1) The radial artery cephalic vein pass subcutaneously over the snuffbox. 3) Superficial branch of the radial nerve pass subcutaneously over the snuffbox. Blood supply of the hand Anastomoses occur between the radial and ulnar arteries via the superficial and deep palmar arches The Deep palmar arch is formed mainly by the radial artery while the superficial palmar arch is formed mainly by the ulnar artery 3-On entering the palm, it curves laterally behind (deep) the palmar 4-The arch is aponeurosis and in front completed on (superficial) of the long flexor the lateral side tendons forming by the the superficial palmar arch superficial branch of the radial artery. 2-Then it gives off its deep branch of which runs in front of the FR , and joins the radial artery to complete the deep palmar arch 1-Enters the hand anterior (superficial) to the Superficial flexor retinaculum palmar branch of radial artery through Guyon’s canal Radial artery 5-The superficial palmar arch gives off digital arteries from its convexity which pass to the fingers and supply them Superficial palmar arch Deep palmar branch of ulnar artery Superficial palmar branch of radial artery Ulnar artery Radial artery Radial Artery first dorsal interosseous muscle 1-From the floor of the anatomical snuff-box the radial artery leaves the dorsum of the hand by turning forward between the two heads of the first dorsal interosseous muscle. -

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -

Ulnar Claw-Hand Related Neglected Post-Traumatic Anterior Shoulder Joint Dislocation
Open Access Library Journal 2017, Volume 4, e3454 ISSN Online: 2333-9721 ISSN Print: 2333-9705 Ulnar Claw-Hand Related Neglected Post-Traumatic Anterior Shoulder Joint Dislocation Hermawan Nagar Rasyid Department of Orthopaedics and Traumatology, Faculty of Medicine, Universitas Padjadjaran, Dr. Hasan Sadikin Teaching Hospital, Bandung, Indonesia How to cite this paper: Rasyid, H.N. Abstract (2017) Ulnar Claw-Hand Related Neglected Post-Traumatic Anterior Shoulder Joint Shoulder joint is the most frequently dislocated joint. Humeral head disloca- Dislocation. Open Access Library Journal, tion pushed the nerve toward medial side. Neglected shoulder dislocation is 4: e3454. difficult to manage and requires extensive procedures to obtain good func- https://doi.org/10.4236/oalib.1103454 tional outcome. In the case of negligence, it is often found loss of the anterior Received: February 13, 2017 capsule due to absorption of the capsule. Nerve lesions, in particular the ulnar Accepted: March 17, 2017 nerve, often do not receive attention. Clinically, it often occurred from neura- Published: March 20, 2017 praxia to severe condition like claw-hand deformity. In my experience of a Copyright © 2017 by author and Open neglected case, there was a 53-year-old woman who presented to the ortho- Access Library Inc. paedic clinic with a left anterior shoulder fracture dislocation following a fall This work is licensed under the Creative onto the right shoulder and upper right arm. She had treated herself at home Commons Attribution International for around six months before visiting the clinic. She also complained of some License (CC BY 4.0). http://creativecommons.org/licenses/by/4.0/ deformities on her ring and little fingers, known as ulnar claw-hand. -

UNMH Orthopedic Surgery Clinical Privileges
UNMH Orthopedic Surgery Clinical Privileges Name: Effective Dates: To: o Initial privileges (initial appointment) o Renewal of privileges (reappointment) o Expansion of privileges (modification) All new applicants must meet the following requirements as approved by the UNMH Board of Trustees effective: 05/30/2014 INSTRUCTIONS Applicant: Check off the "Requested" box for each privilege requested. Applicants have the burden of producing information deemed adequate by the Hospital for a proper evaluation of current competence, current clinical activity, and other qualifications and for resolving any doubts related to qualifications for requested privileges. Department Chair: Check the appropriate box for recommendation on the last page of this form. If recommended with conditions or not recommended, provide condition or explanation on the last page of this form. OTHER REQUIREMENTS 1. Note that privileges granted may only be exercised at UNM Hospitals and clinics that have the appropriate equipment, license, beds, staff, and other support required to provide the services defined in this document. Site-specific services may be defined in hospital or department policy. 2. This document defines qualifications to exercise clinical privileges. The applicant must also adhere to any additional organizational, regulatory, or accreditation requirements that the organization is obligated to meet. Qualifications for Orthopedic Surgery Practice Area Code: 42 Version Code: 05-2014a Initial Applicant - To be eligible to apply for privileges in orthopedic -

06-1733 ) Issued: October 17, 2006 DEPARTMENT of the NAVY, MARINE ) CORPS, Camp Lejeune, NC, Employer ) ______)
United States Department of Labor Employees’ Compensation Appeals Board __________________________________________ ) L.S., Appellant ) ) and ) Docket No. 06-1733 ) Issued: October 17, 2006 DEPARTMENT OF THE NAVY, MARINE ) CORPS, Camp LeJeune, NC, Employer ) __________________________________________ ) Appearances: Case Submitted on the Record Appellant, pro se Office of Solicitor, for the Director DECISION AND ORDER Before: ALEC J. KOROMILAS, Chief Judge MICHAEL E. GROOM, Alternate Judge JAMES A. HAYNES, Alternate Judge JURISDICTION On July 24, 2006 appellant filed a timely appeal from the Office of Workers’ Compensation Programs’ June 9, 2006 merit decision terminating her compensation. Pursuant to 20 C.F.R. §§ 501.2(c) and 501.3(d)(2), the Board has jurisdiction over the merits of this case. ISSUE The issue is whether the Office met its burden of proof to terminate appellant’s compensation effective June 10, 2006 on the grounds that she no longer had residuals of her employment injury after that date. FACTUAL HISTORY On May 5, 2000 appellant, then a 52-year-old registered dental hygienist, filed an occupational disease claim alleging that she sustained a ganglion cyst on the dorsum of her right wrist due to repeatedly grasping instruments at work. The Office accepted that appellant sustained a ganglion cyst of her right wrist. She stopped work on May 5, 2000 to undergo an excision of the mass of her ganglion cyst and repair of the extensor tendon of the right long finger. The surgery was performed by Dr. Richard S. Bahner, an attending Board-certified orthopedic surgeon, and was authorized by the Office. In July 2000, appellant returned to light-duty work on a full-time basis for the employing establishment. -

POST-OPERATIVE INSTRUCTIONS for HAND / UPPER EXTREMITY SURGERY Department of Orthopaedics ------After Your Surgery, Follow the Instructions As Checked Below
POST-OPERATIVE INSTRUCTIONS FOR HAND / UPPER EXTREMITY SURGERY Department of Orthopaedics --------------------------------------------------------------------------------------------------------------------------------------------------------------- After your surgery, follow the instructions as checked below. Instructions following anesthesia or sedation The medicines and/or anesthesia that you received today are strong and will affect your body for at least the next few hours. You may have trouble with coordination or thinking because of these medicines. For your safety, follow these instructions carefully for the next 24 hours: Do not drive at all. You must be taken home today by a responsible adult. Do not drink any alcoholic beverages You should rest today. Do not go to work. You should not do things that require you to think and act quickly. You should not do things that require careful work. For example, avoid cooking, sewing, and operating machinery or electrical appliances. You should not make important decisions or sign legal papers today. The medicines may make you feel drowsy or sick to your stomach. Or you may have a poor appetite. If these problems last longer than 24 hour or if they are severe, call your doctor. Medicines Refer to separate “Patient Medication List” Pain and Prescription Medicine You have been given a prescription for pain medicine. Take it as directed. Do not drive or drink alcohol while you are taking “narcotic” pain medicines. This includes medicine like: Percocet® (oxycodone hydrochloride; acetaminophen), Tylenol #3® (acetaminophen; codeine) and Vicodin® (hydrocodone bitartrate; acetaminophen). Nausea, dizziness and drowsiness are normal side effects of prescribed pain medicine. If you have these symptoms and can not tolerate them, stop taking the medicine. -

Distal Radial Approach Through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention
Korean Circ J. 2018 Dec;48(12):1131-1134 https://doi.org/10.4070/kcj.2018.0293 pISSN 1738-5520·eISSN 1738-5555 Editorial Distal Radial Approach through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention Jae-Hyung Roh, MD, PhD, and Jae-Hwan Lee , MD, PhD Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea ► See the article “Feasibility of Coronary Angiography and Percutaneous Coronary Intervention via Left Snuffbox Approach” in volume 48 on page 1120. Received: Aug 27, 2018 The anatomical snuffbox, also known as the radial fossa, is a triangular-shaped depression Accepted: Sep 17, 2018 on the radial, dorsal aspect of the hand at the level of the carpal bones. It is clearly observed Figure 1 1)2) Correspondence to when the thumb is extended ( ). The bottom of the snuffbox is supported by carpal Jae-Hwan Lee, MD, PhD bones composed of the scaphoid and trapezium. The medial and lateral borders are bounded Division of Cardiology, Department of Internal by tendons of the extensor pollicis longus and the extensor pollicis brevis, respectively. The Medicine, Chungnam National University proximal border is formed by the styloid process of the radius. Within this narrow triangular Hospital, Chungnam National University space, various structures are located, including the distal radial artery (RA), a branch of the School of Medicine, 282, Munhwa-ro, Jung-gu, radial nerve, and the cephalic vein. Daejeon 35015, Korea. E-mail: [email protected] The anatomy of the hand arteries is illustrated in Figure 2. -
The Efficacy and Safety of Gabapentin in Carpal Tunnel Patients: Open Label Trial
Original Article The efficacy and safety of gabapentin in carpal tunnel patients: Open label trial A. Kemal Erdemoglu Ayhan Varlibas, Kirikkale University, Faculty of Medicine, Department of Neurology, Kirikkale, 07100, Turkey Abstract Background: Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy caused by median nerve compression at the wrist. It results in loss of considerable man days and the effectiveness the various treatment modalities are still debated. Aim: To study the efficacy of gabapentin in patients with CTS. The study aim is to investigate the efficacy of gabapentin in patients with CTS patients who were refractory to the other conservative measures or unwilling for the surgical procedure. Materials and Methods: Forty one patients diagnosed as idiopathic CTS were included in the study. Patients were assessed with symptom severity scale (SSS) and functional status scale (FSS) scores of Boston Carpal Tunnel Questionnaire (BCTQ) before and at 1, 3, and 6 months of the treatment. Response to therapy was determined by using SSS and FSS scores of Address for correspondence: BCTQ. Results: The median dosage of gabapentin was 1800 mg/daily. Side effects Dr. A. Kemal Erdemoglu were mild and transient. There was a statistically significant difference in both symptom Kirikkale University, Faculty of Medicine, SSS and FSS scores between before and after treatment in patient groups at the end Department of Neurology, of six months (P < 0.001). According to grading the changes in subscales of BCTQ, Kirikkale, 07100, TURKEY. of 41 patients, 34.1 and 29.3 had a ≥ 40% decrease in SSS and FSS, respectively. E-mail: [email protected] Conclusion: Gabapentin was found to be partially effective and safe in symptomatic treatment of CTS patients. -

Wrist and Hand Examina[On
Wrist and Hand Examinaon Daniel Lueders, MD Assistant Professor Physical Medicine and Rehabilitaon Objecves • Understand the osseous, ligamentous, tendinous, and neural anatomy of the wrist and hand • Outline palpable superficial landmarks in the wrist and hand • Outline evaluaon of and differen.aon between nerves to the wrist and hand • Describe special tes.ng of wrist and hand Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Inspec.on • Ecchymosis • Erythema • Deformity • Laceraon Inspec.on • Common Finger Deformies • Swan Neck Deformity • Boutonniere Deformity • Hypertrophic nodules • Heberden’s, Bouchard’s Inspec.on • Swan Neck Deformity • PIP hyperextension, DIP flexion • Pathology is at PIP joint • Insufficiency of volar/palmar plate and suppor.ng structures • Distally, the FDP tendon .ghtens from PIP extension causing secondary DIP flexion • Alternavely, extensor tendon rupture produces similar deformity Inspec.on • Boutonniere Deformity • PIP flexion, DIP hyperextension • Pathology is at PIP joint • Commonly occurs from insufficiency of dorsal and lateral suppor.ng structures at PIP joint • Lateral bands migrate volar/palmar, creang increased flexion moment • Results in PIP “buTon hole” effect dorsally Inspec.on • Nodules • Osteoarthri.c • Hypertrophic changes of OA • PIP - Bouchard’s nodule • DIP - Heberden’s nodule • Rheumatoid Arthri.s • MCP joints affected most • Distal radioulnar joint can also be affected -

Ultrasound-Guided Access of the Distal Radial Artery at the Anatomical Snuffbox for Catheter-Based Vascular Interventions: a Technical Guide
Title: Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. Authors: Anastasia Hadjivassiliou, MBBS, BSc; Ferdinand Kiemeneij, M.D, PhD; Sandeep Nathan, M.D, MSc; Darren Klass, M.D, PhD DOI: 10.4244/EIJ-D-19-00555 Citation: Hadjivassiliou A, Kiemeneij F, Nathan S, Klass D. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. EuroIntervention 2019; Jaa-625 2019, doi: 10.4244/EIJ-D-19-00555 Manuscript submission date: 10 June 2019 Revisions received: 24 July 2019 Accepted date: 01 August 2019 Online publication date: 06 August 2019 Disclaimer: This is a PDF file of a "Just accepted article". This PDF has been published online early without copy editing/typesetting as a service to the Journal's readership (having early access to this data). Copy editing/typesetting will commence shortly. Unforeseen errors may arise during the proofing process and as such Europa Digital & Publishing exercise their legal rights concerning these potential circumstances. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide Anastasia Hadjivassiliou, MBBS, BSc1; Ferdinand Kiemeneij, MD, PhD2; Sandeep Nathan, MD, MSc3; Darren Klass, MD, PhD1 1. Department of Interventional Radiology, Vancouver General Hospital, University of British Columbia, Canada 2. Department of Cardiology, Tergooi Hospital, Blaricum, the Netherlands 3. University of Chicago Medicine, Chicago, IL, USA Short title: Ultrasound guided distal radial artery access at the anatomical snuffbox Corresponding author: Dr Darren Klass Department of Radiology, Vancouver General Hospital 899 West 12th Avenue, V5Z 1M9, Vancouver, BC, Canada Email address: [email protected] Disclaimer : As a public service to our readership, this article -- peer reviewed by the Editors of EuroIntervention - has been published immediately upon acceptance as it was received.