Chikungunya and O'nyong-Nyong Viruses in Uganda: Implications For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uveal Involvement in Marburg Virus Disease B
Br J Ophthalmol: first published as 10.1136/bjo.61.4.265 on 1 April 1977. Downloaded from British Journal of Ophthalmology, 1977, 61, 265-266 Uveal involvement in Marburg virus disease B. S. KUMING AND N. KOKORIS From the Department of Ophthalmology, Johannesburg General Hospital and University of the Witwatersrand SUMMARY The first reported case of uveal involvement in Marburg virus disease is described. 'Ex Africa semper aliquid novi'. Two outbreaks of Marburg virus disease have been Rhodesia and had also been constantly at his documented. The first occurred in Marburg and bedside till his death. Lassa fever was suspected and Frankfurt, West Germany, in 1967 (Martini, 1969) she was given a unit of Lassa fever convalescent and the second in Johannesburg in 1975 (Gear, serum when she became desperately ill on the fifth 1975). This case report describes the third patient day. She also developed acute pancreatitis. Within in the Johannesburg outbreak, who developed an 52 hours she made a dramatic and uneventful anterior uveitis. The cause of the uveitis was proved recovery. Her illness mainly affected the haema- to be the Marburg virus by identiying it in a tissue topoietic, hepatic, and pancreatic systems. culture of her aqueous fluid. The subject of this report was a nurse who had helped to nurse patients 1 and 2. Nine days after the Case report death ofthe first patient she presented with lower back pain and high fever. She developed hepatitis, a mild Before describing the case history of the patient the disseminated intravascular coagulation syndrome, events leading to her contracting the disease must successfully treated with heparin, and the classical be briefly described. -

As a Model of Human Ebola Virus Infection
Viruses 2012, 4, 2400-2416; doi:10.3390/v4102400 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Review The Baboon (Papio spp.) as a Model of Human Ebola Virus Infection Donna L. Perry 1,*, Laura Bollinger 1 and Gary L.White 2 1 Integrated Research Facility, Division of Clinical Research, NIAID, NIH, Frederick, MD, USA; E-Mail: [email protected] 2 Department of Pathology, University of Oklahoma Baboon Research Resource, University of Oklahoma, Ft. Reno Science Park, OK, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-301-631-7249; Fax: +1-301-619-5029. Received: 8 October 2012; in revised form: 17 October 2012 / Accepted: 17 October 2012 / Published: 23 October 2012 Abstract: Baboons are susceptible to natural Ebola virus (EBOV) infection and share 96% genetic homology with humans. Despite these characteristics, baboons have rarely been utilized as experimental models of human EBOV infection to evaluate the efficacy of prophylactics and therapeutics in the United States. This review will summarize what is known about the pathogenesis of EBOV infection in baboons compared to EBOV infection in humans and other Old World nonhuman primates. In addition, we will discuss how closely the baboon model recapitulates human EBOV infection. We will also review some of the housing requirements and behavioral attributes of baboons compared to other Old World nonhuman primates. Due to the lack of data available on the pathogenesis of Marburg virus (MARV) infection in baboons, discussion of the pathogenesis of MARV infection in baboons will be limited. -

The Hemorrhagic Fevers of Southern Africa South African Institute For
THE YALE JOURNAL OF BIOLOGY AND MEDICINE 55 (1982), 207-212 The Hemorrhagic Fevers of Southern Africa with Special Reference to Studies in the South African Institute for Medical Research J.H.S. GEAR, M.D. National Institute for Virology, Johannesburg, South Africa Received April 19, 1982 In this review of studies on the hemorrhagic fevers of Southern Africa carried out in the South African Institute for Medical Research, attention has been called to occurrence of meningococcal septicemia in recruits to the mining industry and South African Army, to cases of staphylococcal and streptococcal septicemia with hemorrhagic manifestations, and to the occurrence of plague which, in its septicemic form, may cause a hemorrhagic state. "Onyalai," a bleeding disease in tropical Africa, often fatal, was related to profound throm- bocytopenia possibly following administration of toxic witch doctor medicine. Spirochetal diseases, and rickettsial diseases in their severe forms, are often manifested with hemorrhagic complications. Of enterovirus infections, Coxsackie B viruses occasionally caused severe hepa- titis associated with bleeding, especially in newborn babies. Cases of hemorrhagic fever presenting in February-March, 1975 are described. The first out- break was due to Marburg virus disease and the second, which included seven fatal cases, was caused by Rift Valley fever virus. In recent cases of hemorrhagic fever a variety of infective organisms have been incriminated including bacterial infections, rickettsial diseases, and virus diseases, including Herpesvirus hominis; in one patient, the hemorrhagic state was related to rubella. A boy who died in a hemorrhagic state was found to have Congo fever; another pa- tient who died of severe bleeding from the lungs was infected with Leptospira canicola, and two patients who developed a hemorrhagic state after a safari trip in Northern Botswana were infected with Trypanosoma rhodesiense. -

Ebola in the DRC: Report September 2020
The Congo Research Group (CRG) is an independent, non-profit research project dedicated to understanding the violence that affects millions of Congolese. We carry out rigorous research on different aspects of the conflict in the Democratic Republic of the Congo. All of our research is informed by deep historical and social knowledge of the problem at hand. We are based at the Center on International Cooperation at New York University. All of our publications, blogs and podcasts are available at: www.congoresearchgroup.org and www.gecongo.org This report was made possible thanks to funding from the European Union through its Instrument contributing to Stability and Peace. Cover photo: 17 January 2019, Beni, North Kivu region, Democratic Republic of Congo. A doctor talks with Julie, in her cube at the Ebola Treatment Center. Photo: World Bank / Vincent Tremeau Ebola in the DRC: Report September 2020 Table of Contents Executive Summary ...................................................................................................................................... 4 Introduction ................................................................................................................................................. 5 Ebola: From Neglected Tropical Disease to Global Health Security Threat ....................................................... 7 Medicine in DRC: From Colonial Tool to Site of Extraction .............................................................................. 8 The Building of a Parallel Health System .....................................................................................................11 -
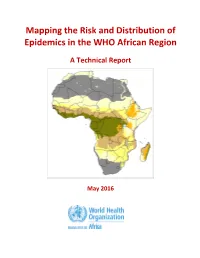
Mapping the Risk and Distribution of Epidemics in the WHO African Region
Mapping the Risk and Distribution of Epidemics in the WHO African Region A Technical Report May 2016 WHO/AFRO Library Cataloguing – in – Publication Data Mapping the Risk and Distribution of Epidemics in the WHO African Region: a technical report 1. Disease Outbreaks – statistics and numerical data 2. Epidemics – statistics and numerical data 3. Communicable Diseases – statistics and numerical data 4. Risk Assessment – supply and distribution – statistics and numerical data 5. Data collection – utilization 6. Africa I. Work Health Organization. Regional Office for Africa II. Title ISBN: 978-9290233084-4 (NLM Classification : WA 105) © WHO Regional Office for Africa, 2016 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. Copies of this publication may be obtained from the Library, WHO Regional Office for Africa, P.O. Box 6, Brazzaville, Republic of Congo (Tel: +47 241 39100; Fax: +47 241 39507; E-mail: [email protected]). Requests for permission to reproduce or translate this publication – whether for sale or for non-commercial distribution – should be sent to the same address. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Mark Woolhouse University of Edinburgh, UK
WHAT WILL CAUSE THE NEXT PANDEMIC? Mark Woolhouse University of Edinburgh, UK With thanks to: Feifei Zhang, Lu Lu, Liam Brierley, Alistair Morrison, Tara Wagner-Gamble and many others WHAT WILL CAUSE THE NEXT PANDEMIC? The 2018 list of disease priorities needing urgent R&D attention comprises: Crimean-Congo haemorrhagic fever (CCHF) Ebola virus disease and Marburg virus disease Lassa fever MERS-CoV and SARS Nipah and henipaviral diseases Rift Valley fever (RVF) The possibility that a serious Zika international epidemic could be Disease X caused by a pathogen currently unknown to cause human disease Candidates included “highly pathogenic coronaviral diseases other than MERS and SARS” Mark Woolhouse, University of Edinburgh, September 2020 WHAT WILL CAUSE THE NEXT PANDEMIC? • Virus discovery • Known viruses • Disease X • Virus diversity • SARS-CoV-2 WHAT WILL CAUSE THE NEXT PANDEMIC? • Virus discovery • Known viruses • Disease X • Virus diversity • SARS-CoV-2 HUMAN PATHOGEN SURVEY • Systematic review of primary literature • Formal methodology → Taylor et al. (2001) Phil. Trans. B • 70% EIDs are zoonotic • 70% EIDs caused by RNA viruses 214 recognised RNA virus species (to 2015) 55 genera 21 families (+1 unassigned genus) Mark Woolhouse, University of Edinburgh, September 2020 RNA VIRUS DISCOVERY Mark Woolhouse, University of Edinburgh, September 2020 Woolhouse & Brierley (2018) Scientific Data PREDICTING WHERE Risk maps created using a boosted regression tree model with 33 predictors. Models trained on 223 discoveries worldwide and 83 in China. Top predictors: GDP/GDP growth > urbanisation > climate > biodiversity. Discoveries since 2015 indicated (black triangles) and location of Wuhan shown. Mark Woolhouse, University of Edinburgh, September 2020 Zhang et al. -

Zoonotic Potential of International Trade in CITES-Listed Species Annexes B, C and D JNCC Report No
Zoonotic potential of international trade in CITES-listed species Annexes B, C and D JNCC Report No. 678 Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex C: CITES-listed species and directly associated zoonotic diseases Annex D: Full trade summaries by taxonomic family UNEP-WCMC & JNCC May 2021 © JNCC, Peterborough 2021 Zoonotic potential of international trade in CITES-listed species Prepared for JNCC Published May 2021 Copyright JNCC, Peterborough 2021 Citation UNEP-WCMC and JNCC, 2021. Zoonotic potential of international trade in CITES- listed species. JNCC Report No. 678, JNCC, Peterborough, ISSN 0963-8091. Contributing authors Stafford, C., Pavitt, A., Vitale, J., Blömer, N., McLardy, C., Phillips, K., Scholz, L., Littlewood, A.H.L, Fleming, L.V. & Malsch, K. Acknowledgements We are grateful for the constructive comments and input from Jules McAlpine (JNCC), Becky Austin (JNCC), Neville Ash (UNEP-WCMC) and Doreen Robinson (UNEP). We also thank colleagues from OIE for their expert input and review in relation to the zoonotic disease dataset. Cover Photographs Adobe Stock images ISSN 0963-8091 JNCC Report No. 678: Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex B: Taxonomic orders and associated zoonotic diseases Table B1: Taxonomic orders1 associated with at least one zoonotic disease according to the source papers, ranked by number of associated zoonotic diseases identified. -

Ebola and Marburg Virus Disease Epidemics: Preparedness, Alert, Control and Evaluation
EBOLA STRATEGY Ebola and Marburg virus disease epidemics: preparedness, alert, control and evaluation August 2014 © World Health Organization 2014. All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. WHO/HSE/PED/CED/2014.05 Contents Acknowledgements ............................................................................................................ 5 List of abbreviations and acronyms ................................................................................... 6 Chapter 1 – Introduction .................................................................................................... 7 1.1 Purpose of the document and target audience .................................................................... -

The Viral Cycle of Ebola Virus Disease and Marburg Virus
THE VIRAL CYCLE OF EBOLA VIRUS DISEASE SURSY AND MARBURG VIRUS DISEASE Reservoir of Marburg and presumed reservoir of Ebola : CONSUMPTION It is impossible to of fruit partially eaten by bats morphologically distinguish between Marburg virus and CONTACT Frugivorous and insectivorous Ebola virus. with the blood or secretions Both are filoviruses of infected carriers BATS that cause similar symptoms. healthy disease carriers HUNTING AND PREPARATION of infected bushmeat CONSUMPTION of fruit partially eaten by bats VISITING places that house bats (bites, saliva scratches, urine, 90% and excrement) estimated mortality rate for great apes infected by EVD SUSPECTED TRANSMISSION CONTACT CONTACT with blood or with the blood and secretions during hunting, secretions of sick people handling of dead or (vomit, excrement, sweat, sick animals and the tears, sperm) or preparation of infected contaminated bushmeat objects Victims and intermediary hosts HUMAN EPIDEMIC This project is financed by the European Union OI01001_FICHE A4_EBOLA-MARBURG_ANG.indd 1 16/04/2019 17:10 EBOLA AND MARBURG VIRUS DISEASES SURSY EBOLA VIRUS disease (EVD) and MARBURG VIRUS disease are COMPLEX ZOONOSES for which the transmission cycles remain the subject of scientific research. While these filoviruses are distinct, their cycles and their impact share many similar characteristics. UNDERSTANDING THE CYCLE OF WHAT SHOULD YOU DO EBOLA AND MARBURG VIRUS DISEASES CLINICAL SIGNS WHEN YOU SUSPECT A CASE IN WILDLIFE? CONCERNED SPECIES WARNING SIGNS in animals DO NOT TOUCH THE CARCASS without personal protective 1 equipment (PPE). Humans, non-human primates (chimpanzees, gorillas, monkeys), • Death from unknown and/or suspicious causes and duiker antelopes. of a large number of great apes or of other animals Pigs have been found to be susceptible to Ebola in laboratory susceptible to EVD infection. -
Zika Virus SCACM Audioconference January 24, 2017 PACE #: 362-001
A Review of Emerging and Re- Emerging Zoonotic Viruses of the 21st Century Ryan F. Relich, PhD, D(ABMM), MLS(ASCP)SM Assistant Professor, Clinical Pathology and Laboratory Medicine Indiana University School of Medicine Section Director, Clinical Microbiology and Serology (Eskenazi Health) Section Director, Clinical Virology Laboratory (IU Health) Medical Director, Special Pathogens Unit Laboratory (IU Health) Associate Medical Director, Division of Clinical Microbiology (IU Health) Associate Medical Director, Division of Molecular Pathology (IU Health) Indianapolis, IN USA Disclosures and disclaimers • Research funding/support • Abbott, BD Diagnostics, Beckman Coulter, Cepheid, Luminex Corporation, Roche, Sekisui, STAT-Diagnostica • Travel support by First Coast ID/CM Symposium • PASCV sponsorship Objectives • At the end of this presentation, audience members will be able to: • Describe the basic biology, ecology, and epidemiology of the viruses discussed; • Identify factors associated with the emergence or re- emergence of zoonotic viruses; and, • List clinical features of diseases caused by several zoonotic viruses, as well as their detection, treatment, and prevention. Outline • What are emerging zoonotic viruses and where do they come from? • Overview / introduction to selected viruses • Role of applied and basic research in detecting and controlling these agents • Summary What are emerging pathogens? • “Infectious diseases whose incidence has increased in the past 20 years and could increase in the future.” • Caused by • Newly recognized -

Marburg Hemorrhagic Fever
Marburg Hemorrhagic Fever Marburg hemorrhagic fever (Marburg HF) is a rare but severe hemorrhagic fever which affects both humans and non-human primates. Marburg HF is caused by Marburg virus, a genetically unique zoonotic (or, animal-borne) RNA virus of the filovirus family. The five species of Ebola virus are the only other known members of the filovirus family. Marburg virus was first recognized in 1967, when outbreaks of hemorrhagic fever occurred simultaneously in laboratories in Marburg and Frankfurt, Germany and in Belgrade, Yugoslavia (now Serbia). Thirty-one people became ill, initially laboratory workers followed by several medical personnel and family members who had cared for them. Seven deaths were reported. The first people infected had been exposed to imported African green monkeys or their tissues while conducting research. One additional case was diagnosed retrospectively. The reservoir host of Marburg virus is the African fruit bat, Rousettus aegyptiacus. Fruit bats infected with Marburg virus do not to show obvious signs of illness. Primates (including humans) can become infected with Marburg virus, and may develop serious disease with high mortality. Further study is needed to determine if other species may also host the virus. This Rousettus bat is a sighted, cave-dwelling bat widely distributed across Africa. Given the fruit bat's wide distribution, more areas are potentially at risk for outbreaks of Marburg HF than previously suspected. The virus is not known to be native to other continents, such as North America. Marburg HF typically appears in sporadic outbreaks throughout Africa; laboratory confirmed cases have been reported in Uganda, Zimbabwe, the Democratic Republic of the Congo, Kenya, Angola, and South Africa. -

Filoviruses: One of These Things Is (Not) Like the Other
Review Filoviruses: One of These Things is (not) Like the Other Scott M. Anthony 1 and Steven B. Bradfute 2,* Received: 6 August 2015 ; Accepted: 16 September 2015 ; Published: 29 September 2015 Academic Editor: Jens H. Kuhn 1 Immunology Graduate Program, The University of Texas Graduate School of Biomedical Sciences at Houston, Department of Immunology, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] 2 University of New Mexico, Center for Global Health, Department of Internal Medicine, MSC10 5550, 1 University of New Mexico, Albuquerque, NM 87131, USA * Correspondence: [email protected]; Tel.: +1-505-925-1021; Fax: +1-505-272-8441 Abstract: The family Filoviridae contains several of the most deadly pathogens known to date and the current Ebola virus disease (EVD) outbreak in Western Africa, due to Ebola virus (EBOV) infection, highlights the need for active and broad research into filovirus pathogenesis. However, in comparison, the seven other known filovirus family members are significantly understudied. Many of these, including Marburgviruses and Ebolaviruses other than EBOV, are also highly virulent and fully capable of causing widespread epidemics. This review places the focus on these non-EBOV filoviruses, including known immunological and pathological data. The available animal models, research tools and currently available therapeutics will also be discussed along with an emphasis in the large number of current gaps in knowledge of these less highlighted filoviruses. It is evident that much research is yet to be done in order to bring the non-EBOV filovirus field to the forefront of current research and, importantly, to the development of more effective vaccines and therapeutics to combat potential future outbreaks.