Communicable Disease Threats Report, 18 November 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uveal Involvement in Marburg Virus Disease B
Br J Ophthalmol: first published as 10.1136/bjo.61.4.265 on 1 April 1977. Downloaded from British Journal of Ophthalmology, 1977, 61, 265-266 Uveal involvement in Marburg virus disease B. S. KUMING AND N. KOKORIS From the Department of Ophthalmology, Johannesburg General Hospital and University of the Witwatersrand SUMMARY The first reported case of uveal involvement in Marburg virus disease is described. 'Ex Africa semper aliquid novi'. Two outbreaks of Marburg virus disease have been Rhodesia and had also been constantly at his documented. The first occurred in Marburg and bedside till his death. Lassa fever was suspected and Frankfurt, West Germany, in 1967 (Martini, 1969) she was given a unit of Lassa fever convalescent and the second in Johannesburg in 1975 (Gear, serum when she became desperately ill on the fifth 1975). This case report describes the third patient day. She also developed acute pancreatitis. Within in the Johannesburg outbreak, who developed an 52 hours she made a dramatic and uneventful anterior uveitis. The cause of the uveitis was proved recovery. Her illness mainly affected the haema- to be the Marburg virus by identiying it in a tissue topoietic, hepatic, and pancreatic systems. culture of her aqueous fluid. The subject of this report was a nurse who had helped to nurse patients 1 and 2. Nine days after the Case report death ofthe first patient she presented with lower back pain and high fever. She developed hepatitis, a mild Before describing the case history of the patient the disseminated intravascular coagulation syndrome, events leading to her contracting the disease must successfully treated with heparin, and the classical be briefly described. -

As a Model of Human Ebola Virus Infection
Viruses 2012, 4, 2400-2416; doi:10.3390/v4102400 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Review The Baboon (Papio spp.) as a Model of Human Ebola Virus Infection Donna L. Perry 1,*, Laura Bollinger 1 and Gary L.White 2 1 Integrated Research Facility, Division of Clinical Research, NIAID, NIH, Frederick, MD, USA; E-Mail: [email protected] 2 Department of Pathology, University of Oklahoma Baboon Research Resource, University of Oklahoma, Ft. Reno Science Park, OK, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-301-631-7249; Fax: +1-301-619-5029. Received: 8 October 2012; in revised form: 17 October 2012 / Accepted: 17 October 2012 / Published: 23 October 2012 Abstract: Baboons are susceptible to natural Ebola virus (EBOV) infection and share 96% genetic homology with humans. Despite these characteristics, baboons have rarely been utilized as experimental models of human EBOV infection to evaluate the efficacy of prophylactics and therapeutics in the United States. This review will summarize what is known about the pathogenesis of EBOV infection in baboons compared to EBOV infection in humans and other Old World nonhuman primates. In addition, we will discuss how closely the baboon model recapitulates human EBOV infection. We will also review some of the housing requirements and behavioral attributes of baboons compared to other Old World nonhuman primates. Due to the lack of data available on the pathogenesis of Marburg virus (MARV) infection in baboons, discussion of the pathogenesis of MARV infection in baboons will be limited. -

Wnv-Case-Definition.Pdf
Draft Case Definition for West Nile Fever Animal and Plant Health Inspection Service West Nile Fever Veterinary Services October 2018 Case Definition (Notifiable) 1. Clinical Signs 1.1 Clinical Signs: West Nile Fever (WNF) is a zoonotic mosquito-borne viral disease caused by the West Nile virus (WNV), a Flavivirus of the family Flaviviridae. Many vertebrate species are susceptible to natural WNV infection; however, fatal neurological outbreaks have only been documented in equids, humans, geese, wild birds (particularly corvids), squirrels, farmed alligators, and dogs. Birds serve as the natural host reservoir of WNV. The incubation period is estimated to be three to 15 days in horses Ten to 39 percent of unvaccinated horses infected with WNV will develop clinical signs. Most clinically affected horses exhibit neurological signs such as ataxia (including stumbling, staggering, wobbly gait, or incoordination) or at least two of the following: circling, hind limb weakness, recumbency or inability to stand (or both), multiple limb paralysis, muscle fasciculation, proprioceptive deficits, altered mental status, blindness, lip droop/paralysis, teeth grinding. Behavioral changes including somnolence, listlessness, apprehension, or periods of hyperexcitability may occur. Other common clinical signs include colic, lameness, anorexia, and fever. 2. Laboratory criteria: 2.1 Agent isolation and identification: The virus can be identified by polymerase chain reaction (PCR) and virus isolation (VI). Preferred tissues from equids are brain or spinal cord. 2.2 Serology: Antibody titers can be identified in paired serum samples by IgM and IgG capture enzyme linked immunosorbent assay (ELISA), plaque reduction neutralization test (PRNT), and virus neutralization (VN). Only a single serum sample is required for IgM capture ELISA, and this is the preferred serologic test in live animals. -

The Hemorrhagic Fevers of Southern Africa South African Institute For
THE YALE JOURNAL OF BIOLOGY AND MEDICINE 55 (1982), 207-212 The Hemorrhagic Fevers of Southern Africa with Special Reference to Studies in the South African Institute for Medical Research J.H.S. GEAR, M.D. National Institute for Virology, Johannesburg, South Africa Received April 19, 1982 In this review of studies on the hemorrhagic fevers of Southern Africa carried out in the South African Institute for Medical Research, attention has been called to occurrence of meningococcal septicemia in recruits to the mining industry and South African Army, to cases of staphylococcal and streptococcal septicemia with hemorrhagic manifestations, and to the occurrence of plague which, in its septicemic form, may cause a hemorrhagic state. "Onyalai," a bleeding disease in tropical Africa, often fatal, was related to profound throm- bocytopenia possibly following administration of toxic witch doctor medicine. Spirochetal diseases, and rickettsial diseases in their severe forms, are often manifested with hemorrhagic complications. Of enterovirus infections, Coxsackie B viruses occasionally caused severe hepa- titis associated with bleeding, especially in newborn babies. Cases of hemorrhagic fever presenting in February-March, 1975 are described. The first out- break was due to Marburg virus disease and the second, which included seven fatal cases, was caused by Rift Valley fever virus. In recent cases of hemorrhagic fever a variety of infective organisms have been incriminated including bacterial infections, rickettsial diseases, and virus diseases, including Herpesvirus hominis; in one patient, the hemorrhagic state was related to rubella. A boy who died in a hemorrhagic state was found to have Congo fever; another pa- tient who died of severe bleeding from the lungs was infected with Leptospira canicola, and two patients who developed a hemorrhagic state after a safari trip in Northern Botswana were infected with Trypanosoma rhodesiense. -

Rift Valley Fever for Host Innate Immunity in Resistance to a New
A New Mouse Model Reveals a Critical Role for Host Innate Immunity in Resistance to Rift Valley Fever This information is current as Tânia Zaverucha do Valle, Agnès Billecocq, Laurent of September 25, 2021. Guillemot, Rudi Alberts, Céline Gommet, Robert Geffers, Kátia Calabrese, Klaus Schughart, Michèle Bouloy, Xavier Montagutelli and Jean-Jacques Panthier J Immunol 2010; 185:6146-6156; Prepublished online 11 October 2010; Downloaded from doi: 10.4049/jimmunol.1000949 http://www.jimmunol.org/content/185/10/6146 Supplementary http://www.jimmunol.org/content/suppl/2010/10/12/jimmunol.100094 http://www.jimmunol.org/ Material 9.DC1 References This article cites 46 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/185/10/6146.full#ref-list-1 Why The JI? Submit online. by guest on September 25, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American -
West Nile Virus Questions and Answers
West Nile Virus Questions and Answers Q: How do people get infected with West Nile Virus (WNV)? A: The most likely way a human would become infected with WNV is through the bite of an infected mosquito. Some people have also become infected with WNV following receipt of contaminated blood or blood products, or transplanted organs from an infected donor. Mothers who are recently infected with WNV may also transmit the virus to their unborn child, or to their baby while breastfeeding. Q: Who is at risk for getting West Nile encephalitis? A: All residents of areas where WNV activity has been identified are at risk of getting West Nile encephalitis. Q: What is the time from exposure to onset of disease symptoms for West Nile encephalitis in humans? A: Usually 3 to 15 days. Q: What are the symptoms of West Nile virus infection? A: Most people who are infected with WNV will not have any noticeable illness, or have a mild form of illness called West Nile Fever. Persons with West Nile Fever typically experience symptoms of fever, headache, nausea, muscle weakness, and body aches lasting 2 to 6 days or longer. Sensitivity when looking at light and a skin rash appearing on the trunk of the body may also be present. Approximately 20% of persons infected with WNV will develop more severe neurologic disease that may be life-threatening. Adults over the age of 50 years are at greater risk of having serious disease. Potential symptoms of severe infection (West Nile encephalitis or meningitis) include intense headache, dizziness, severe muscle weakness, neck stiffness, vomiting, disorientation, mental confusion, tremors, muscle paralysis, or convulsions and coma. -

Ebola in the DRC: Report September 2020
The Congo Research Group (CRG) is an independent, non-profit research project dedicated to understanding the violence that affects millions of Congolese. We carry out rigorous research on different aspects of the conflict in the Democratic Republic of the Congo. All of our research is informed by deep historical and social knowledge of the problem at hand. We are based at the Center on International Cooperation at New York University. All of our publications, blogs and podcasts are available at: www.congoresearchgroup.org and www.gecongo.org This report was made possible thanks to funding from the European Union through its Instrument contributing to Stability and Peace. Cover photo: 17 January 2019, Beni, North Kivu region, Democratic Republic of Congo. A doctor talks with Julie, in her cube at the Ebola Treatment Center. Photo: World Bank / Vincent Tremeau Ebola in the DRC: Report September 2020 Table of Contents Executive Summary ...................................................................................................................................... 4 Introduction ................................................................................................................................................. 5 Ebola: From Neglected Tropical Disease to Global Health Security Threat ....................................................... 7 Medicine in DRC: From Colonial Tool to Site of Extraction .............................................................................. 8 The Building of a Parallel Health System .....................................................................................................11 -

West Nile Virus
Oklahoma State Department of Health Acute Disease Service Public Health Fact Sheet West Nile Virus What is West Nile virus? West Nile virus is one of a group of viruses called arboviruses that are spread by mosquitoes and may cause illness in birds, animals, and humans. West Nile virus was not known to be present in the United States until the summer of 1999. Previously, West Nile virus was only found in Africa, western Asia, the Middle East, and Eastern Europe. Where is West Nile virus in the United States? West Nile virus was first identified as a disease threat in the United States during the summer of 1999 and was limited to the northeastern states through 2000. However, the virus rapidly expanded its geographic range. By the end of 2004, West Nile virus had spread from the Atlantic to the Pacific coast with viral activity confirmed in all 48 contiguous states. How is it spread? West Nile virus is primarily spread through the bite of an infected mosquito. Mosquitoes pick up the virus when they feed on infected birds. The virus must then circulate in the mosquito for a few days before they are capable of passing the infection to animals or humans while biting. West Nile virus is not spread person to person through casual contact such as touching or kissing. Rarely, West Nile virus has also been spread through blood transfusions, although blood banks do screen blood supply for the infection. How long does it take to get sick after a bite from an infected mosquito? It takes about three to 15 days for both human and equine (horse, mule, or donkey) illness to occur after a bite from infected mosquito. -

DSHS Arbovirus Activity 061817
Arbovirus Activity in Texas 2017 Surveillance Report June 2018 Texas Department of State Health Services Infectious Disease Control Unit Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California serogroup viruses (CAL), chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2017, reported human arboviral disease cases were attributed to WNV (54%), ZIKV (22%), DENV (17%), and CHIKV (6%) (Table 1). Animal infections or disease caused by CAL, EEEV, SLEV, and WNV were also reported during 2017. Table 1. Year-End Arbovirus Activity Summary, Texas, 2017 California Serogroup Viruses California serogroup viruses (CAL) are bunyaviruses and include California encephalitis virus (CEV), Jamestown Canyon virus, Keystone virus, La Crosse virus (LACV), snowshoe hare virus, and Trivittatus virus. These viruses are maintained in a cycle between mosquito vectors and vertebrate hosts in forest habitats. In the United States (U.S.), approximately 80-100 reported cases of human neuroinvasive disease are caused by LACV each year (CDC), mostly in mid-Atlantic and southeastern states. From 2002-2016, Texas reported a total of 5 cases of human CAL disease (range: 0-3 cases/year): 1 case of CEV neuroinvasive disease and 4 cases of LACV neuroinvasive disease. In 2017, one CEV-positive mosquito pool was identified in Orange County (Figure 1); no human cases of CAL disease were reported. -
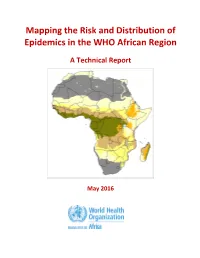
Mapping the Risk and Distribution of Epidemics in the WHO African Region
Mapping the Risk and Distribution of Epidemics in the WHO African Region A Technical Report May 2016 WHO/AFRO Library Cataloguing – in – Publication Data Mapping the Risk and Distribution of Epidemics in the WHO African Region: a technical report 1. Disease Outbreaks – statistics and numerical data 2. Epidemics – statistics and numerical data 3. Communicable Diseases – statistics and numerical data 4. Risk Assessment – supply and distribution – statistics and numerical data 5. Data collection – utilization 6. Africa I. Work Health Organization. Regional Office for Africa II. Title ISBN: 978-9290233084-4 (NLM Classification : WA 105) © WHO Regional Office for Africa, 2016 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. Copies of this publication may be obtained from the Library, WHO Regional Office for Africa, P.O. Box 6, Brazzaville, Republic of Congo (Tel: +47 241 39100; Fax: +47 241 39507; E-mail: [email protected]). Requests for permission to reproduce or translate this publication – whether for sale or for non-commercial distribution – should be sent to the same address. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

West Nile Virus
West Nile Virus Frequently Asked Questions What is West Nile virus? West Nile virus is a viral infection that is spread by the bite of an infected mosquito. Mosquitoes get infected with the West Nile virus by feeding on infected birds. The infected mosquitoes then spread the virus by biting humans and other animals, such as horses. Identified in the United States in 1999, West Nile virus is seen most often during the summer and early fall months. Who gets West Nile virus? Anyone can get infected with the West Nile virus. The virus can affect anyone bitten by an infected mosquito. People over the age of 50 and people with weak immune systems are at greater risk of developing severe illness. How do people get West Nile virus? The virus is spread by the bite of a mosquito infected with the West Nile virus. What are the symptoms of West Nile virus? Many people infected with West Nile virus do not become ill and may not develop symptoms. About 20% of infected people will develop West Nile fever. When symptoms do occur, they may be mild or severe and show up 3 to 15 days after being bitten by an infected mosquito. • Mild symptoms inlcude flu-like illness with fever, headache, body aches, nausea and sometimes swollen lymph glands or a skin rash on the chest, stomach and back. • Severe symptoms include high fever, neck stiffness and swelling of the brain (encephalitis) which can lead to coma, convulsions and death. Less than 1% of infected people will develop severe symptoms. -

Mark Woolhouse University of Edinburgh, UK
WHAT WILL CAUSE THE NEXT PANDEMIC? Mark Woolhouse University of Edinburgh, UK With thanks to: Feifei Zhang, Lu Lu, Liam Brierley, Alistair Morrison, Tara Wagner-Gamble and many others WHAT WILL CAUSE THE NEXT PANDEMIC? The 2018 list of disease priorities needing urgent R&D attention comprises: Crimean-Congo haemorrhagic fever (CCHF) Ebola virus disease and Marburg virus disease Lassa fever MERS-CoV and SARS Nipah and henipaviral diseases Rift Valley fever (RVF) The possibility that a serious Zika international epidemic could be Disease X caused by a pathogen currently unknown to cause human disease Candidates included “highly pathogenic coronaviral diseases other than MERS and SARS” Mark Woolhouse, University of Edinburgh, September 2020 WHAT WILL CAUSE THE NEXT PANDEMIC? • Virus discovery • Known viruses • Disease X • Virus diversity • SARS-CoV-2 WHAT WILL CAUSE THE NEXT PANDEMIC? • Virus discovery • Known viruses • Disease X • Virus diversity • SARS-CoV-2 HUMAN PATHOGEN SURVEY • Systematic review of primary literature • Formal methodology → Taylor et al. (2001) Phil. Trans. B • 70% EIDs are zoonotic • 70% EIDs caused by RNA viruses 214 recognised RNA virus species (to 2015) 55 genera 21 families (+1 unassigned genus) Mark Woolhouse, University of Edinburgh, September 2020 RNA VIRUS DISCOVERY Mark Woolhouse, University of Edinburgh, September 2020 Woolhouse & Brierley (2018) Scientific Data PREDICTING WHERE Risk maps created using a boosted regression tree model with 33 predictors. Models trained on 223 discoveries worldwide and 83 in China. Top predictors: GDP/GDP growth > urbanisation > climate > biodiversity. Discoveries since 2015 indicated (black triangles) and location of Wuhan shown. Mark Woolhouse, University of Edinburgh, September 2020 Zhang et al.