Treatment of Diseases and Conditions Mediated By
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Management of Common Skin Conditions in General Practice
Management of Common Skin Conditions In General Practice including the “red rash made easy” © Arroll, Fishman & Oakley, Department of General Practice and Primary Health Care University of Auckland, Tamaki Campus Reviewed by Hon A/Prof Amanda Oakley - 2019 http://www.dermnetnz.org Management of Common Skin Conditions In General Practice Contents Page Derm Map 3 Classic location: infants & children 4 Classic location: adults 5 Dermatology terminology 6 Common red rashes 7 Other common skin conditions 12 Common viral infections 14 Common bacterial infections 16 Common fungal infections 17 Arthropods 19 Eczema/dermatitis 20 Benign skin lesions 23 Skin cancers 26 Emergency dermatology 28 Clinical diagnosis of melanoma 31 Principles of diagnosis and treatment 32 Principles of treatment of eczema 33 Treatment sequence for psoriasis 34 Topical corticosteroids 35 Combination topical steroid + antimicrobial 36 Safety with topical corticosteroids 36 Emollients 37 Antipruritics 38 For further information, refer to: http://www.dermnetnz.org And http://www.derm-master.com 2 © Arroll, Fishman & Oakley, Department of General Practice and Primary Health Care, University of Auckland, Tamaki Campus. Management of Common Skin Conditions In General Practice DERM MAP Start Is the patient sick ? Yes Rash could be an infection or a drug eruption? No Insect Bites – Crop of grouped papules with a central blister or scab. Is the patient in pain or the rash Yes Infection: cellulitis / erysipelas, impetigo, boil is swelling, oozing or crusting? / folliculitis, herpes simplex / zoster. Urticaria – Smooth skin surface with weals that evolve in minutes to hours. No Is the rash in a classic location? Yes See our classic location chart . -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Taking a Dermatological Approach to Treating Ocular Surface Diseases
Taking a Dermatological Approach to treating Ocular Surface Diseases MARC GLEESON | CHIEF EXECUTIVE OFFICER OIS@SECO 2020 for Meibomian Gland Dysfunction, Contact Lens Discomfort & Blepharitis Copyright© Azura Ophthalmics | Confidential Meibomian Gland Contact Lens Blepharitis Demodex Dysfunction Discomfort Patient Administered Patient Administered Patient Administered Rx Proven activity against Rx Chronic Treatment Rx Chronic Treatment Treatment applied to Demodex applied to the eyelid applied to the eyelid the eyelid Allows continuation of New Chemical Entity In Office Physician Only Contact Lens Wear Administered Rx Treatment Lid Margin Involvement Hyperkeratinization of the Gland Orifice +/- Inflammation Copyright© Azura Ophthalmics | Confidential (MGD) Reduced secretion of lipids leads to instability of the tear film Modified sebaceous (oil-producing) and drying of the ocular surface, leading to damage and the glands responsible for secreting the signs and symptoms of dry eye disease (DED). outer lipid layer (meibum) of the tear film, which lubricates the ocular Obstructive MGD is the most common cause of evaporative surface during blinking and protects dry DED,1,3 and clinical signs of obstructive MGD are present against tear evaporation1,2 in 86% of DED patients4 MGD traditionally regarded as a hypersecretory disorder associated with bacterial infection and inflammation,1 which has guided the approach to treatment, often unsuccessfully 1Blackie et al. Cornea. 2010 | 2Knop et al. Invest Ophthalmol Vis Sci. 2011 | 3Baudouin et al. -
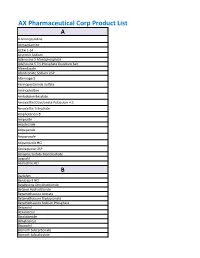
AX Pharmaceutical Corp Product List
AX Pharmaceutical Corp Product List A 4-Aminopyridine Acetazolamine ACTH 1-24 Acyclovir Sodium Adenosine 5 Monophosphate Adenosine 5 Tri-Phosphate Disodium Salt Albendazole Alendronate Sodium USP Alternogest Aminopentamide Sulfate Aminophylline Amlodipine Besylate Amoxicillin/Clavulanate Potassium 4:1 Amoxicillin Trihydrate Amphotericin B Ampicillin Anastrozole Aripepazole Aripiprazole Atipamezole HCl Atovaquone USP Atropine Sulfate Monohydrate Avanafil Azelastine HCl B Baclofen Benazepril HCl Betahistine Dihydrochloride Betaine Hydrochloride Betamethasone Acetate Betamethasone Dipropionate Betamethasone Sodium Phosphate Betaxolol Bexarotene Bicalutamide Bimatoprost Bisacodyl Bismuth Subcarbonate Bismuth Subsalicylate Bleomycin A5 Hydrochloride Bleomycin Sulfate Bretylium Tosylate Brimonidine Brinzolamide Bromhexine Bromocriptine Mesylate Brompheniramine Maleate Budesonide Bumetanide Bupivacaine Base Bupivacaine Hydrochloride Buprenorphine Bupropion HCl Buspirone Hydrochloride Busulfan Butaphosphan Butylated Hydroxyanisole C Cabergoline Calamine Calcium Glycerophosphate Calcium Levulinate Dihydrate Capsaicin Captopril Carbamazepine Carbazochrome Carbenoxolone Carbetocin Acetate Carbidopa Carbocisteine Carboplatin Carmustine Carprofen Carvedilol Cefadroxil Hemihydrate Cefadroxil Monohydrate Cefazolin Cefazolin Sodium Cefdinir Cefotaxime Cefotetan Disodium Cefpodoxime Cefpodoxime Proxetil Ceftazidime Ceftiofur Free Acid Ceftiofur Sodium Ceftriaxone Cefuroxime (Ceftin) Celecoxib Cephalexin Base Cephalexin Monohydrate Cesium Chloride Cetirizine -

DRAFT NOTE for GUIDANCE on ORGANIC IMPURITIES in 3 ACTIVE PHARMACEUTICAL INGREDIENTS and FINISHED 4 PHARMACEUTICAL PRODUCTS 5 (July 2016)
Working document QAS/15.606/Rev2 July 2016 Draft document for comment 1 2 DRAFT NOTE FOR GUIDANCE ON ORGANIC IMPURITIES IN 3 ACTIVE PHARMACEUTICAL INGREDIENTS AND FINISHED 4 PHARMACEUTICAL PRODUCTS 5 (July 2016) 6 7 DRAFT FOR COMMENT 8 Should you have any comments on the attached text, please send these to Dr Herbert Schmidt, Medicines Quality Assurance, Technologies, Standards and Norms, World Health Organization, 1211 Geneva 27, Switzerland; email: [email protected]; fax: (+41 22) 791 4730) by 16 September 2016. In order to speed up the process for receiving draft monographs and for sending comments, please let us have your email address (to [email protected]) and we will add it to our electronic mailing list. Please specify if you wish to receive monographs. 9 10 ____________________________________________________________________________________________________ 11 © World Health Organization 2016 12 All rights reserved. 13 This draft is intended for a restricted audience only, i.e. the individuals and organizations having received this draft. The 14 draft may not be reviewed, abstracted, quoted, reproduced, transmitted, distributed, translated or adapted, in part or in whole, 15 in any form or by any means outside these individuals and organizations (including the organizations' concerned staff and 16 member organizations) without the permission of the World Health Organization. The draft should not be displayed on any 17 website. 18 Please send any request for permission to: 19 Dr Sabine Kopp, Group Lead, Medicines Quality Assurance, Technologies, Standards and Norms, Department of Essential 20 Medicines and Health Products, World Health Organization, CH-1211 Geneva 27, Switzerland. 21 Fax: (41-22) 791 4730; email: [email protected]. -

Chemical Names and CAS Numbers Final
Chemical Abstract Chemical Formula Chemical Name Service (CAS) Number C3H8O 1‐propanol C4H7BrO2 2‐bromobutyric acid 80‐58‐0 GeH3COOH 2‐germaacetic acid C4H10 2‐methylpropane 75‐28‐5 C3H8O 2‐propanol 67‐63‐0 C6H10O3 4‐acetylbutyric acid 448671 C4H7BrO2 4‐bromobutyric acid 2623‐87‐2 CH3CHO acetaldehyde CH3CONH2 acetamide C8H9NO2 acetaminophen 103‐90‐2 − C2H3O2 acetate ion − CH3COO acetate ion C2H4O2 acetic acid 64‐19‐7 CH3COOH acetic acid (CH3)2CO acetone CH3COCl acetyl chloride C2H2 acetylene 74‐86‐2 HCCH acetylene C9H8O4 acetylsalicylic acid 50‐78‐2 H2C(CH)CN acrylonitrile C3H7NO2 Ala C3H7NO2 alanine 56‐41‐7 NaAlSi3O3 albite AlSb aluminium antimonide 25152‐52‐7 AlAs aluminium arsenide 22831‐42‐1 AlBO2 aluminium borate 61279‐70‐7 AlBO aluminium boron oxide 12041‐48‐4 AlBr3 aluminium bromide 7727‐15‐3 AlBr3•6H2O aluminium bromide hexahydrate 2149397 AlCl4Cs aluminium caesium tetrachloride 17992‐03‐9 AlCl3 aluminium chloride (anhydrous) 7446‐70‐0 AlCl3•6H2O aluminium chloride hexahydrate 7784‐13‐6 AlClO aluminium chloride oxide 13596‐11‐7 AlB2 aluminium diboride 12041‐50‐8 AlF2 aluminium difluoride 13569‐23‐8 AlF2O aluminium difluoride oxide 38344‐66‐0 AlB12 aluminium dodecaboride 12041‐54‐2 Al2F6 aluminium fluoride 17949‐86‐9 AlF3 aluminium fluoride 7784‐18‐1 Al(CHO2)3 aluminium formate 7360‐53‐4 1 of 75 Chemical Abstract Chemical Formula Chemical Name Service (CAS) Number Al(OH)3 aluminium hydroxide 21645‐51‐2 Al2I6 aluminium iodide 18898‐35‐6 AlI3 aluminium iodide 7784‐23‐8 AlBr aluminium monobromide 22359‐97‐3 AlCl aluminium monochloride -

345 Part 524—Ophthalmic and Top- Ical Dosage Form New Ani- Mal Drugs
Food and Drug Administration, HHS Pt. 524 (3) Steers fed in confinement for slaugh- PART 524—OPHTHALMIC AND TOP- ter—(i) Amount. 72 mg zeranol (one im- ICAL DOSAGE FORM NEW ANI- plant consisting of 6 pellets, each pel- MAL DRUGS let containing 12 mg zeranol) per im- plant dose. Sec. (ii) Indications for use. For increased 524.86 Amitraz. rate of weight gain and improved feed 524.154 Bacitracin, neomycin, and poly- efficiency. myxin B ophthalmic ointment. (iii) Limitations. Implant 524.155 Bacitracin, neomycin, polymyxin B, subcutaneously in ear only. Safety and and hydrocortisone ophthalmic oint- effectiveness have not been established ment. 524.390 Chloramphenicol ophthalmic oint- in veal calves. A withdrawal period has ment. not been established for this product in 524.402 Chlorhexidine. preruminating calves. Do not use in 524.450 Clotrimazole. calves to be processed for veal. 524.463 Copper naphthenate. (4) Pasture cattle (slaughter, stocker, 524.575 Cyclosporine ophthalmic ointment. feeder steers, and heifers)—(i) Amount. 524.590 Diclofenac. 138 mg zeranol (one implant consisting 524.660 Dimethyl sulfoxide. 524.770 Doramectin. of 7 pellets, each of 6 pellets containing 524.775 Emodepside and praziquantel. 20 mg zeranol and a seventh pellet con- 524.802 Enrofloxacin and silver sulfadiazine taining 18 mg zeranol) per implant otic emulsion. dose. 524.814 Eprinomectin. (ii) Indications for use. For increased 524.900 Famphur. rate of weight gain. 524.920 Fenthion. (iii) Limitations. Implant 524.916 Fentanyl. 524.955 Florfenicol, terbinafine, and subcutaneously in ear only. Safety and betamethasone acetate otic gel. effectiveness have not been established 524.957 Florfenicol, terbinafine, and in veal calves. -

The Crucial Role of Topical Therapy
11/21/2019 The Crucial Role of Options for management of skin Topical Therapy disease in Managing skin disease in dogs Joel Griffies, DVM Diplomate ACVD Animal Dermatology Clinic Marietta, GA www.animaldermatology.com 1 2 Topical Therapy Topical Therapy Disadvantages Advantages ◦ More labor intensive/time consuming ◦ Ease of access ◦ Effect may take longer ◦ Safety ◦ Cost? +/- ◦ Lack of systemic side effects ◦ Useful Adjunctive ◦ Replacement for systemic therapies in some 3 4 Topical therapy MYTH - Bathing is bad Questions/Objectives ◦When & Why is topical therapy a useful Reality tool ◦Bathing has been shown to significantly ◦How do we choose what to prescribe help outcome in a variety of skin disorders ◦How does that differ with the condition ◦IF – we’re using the right products being treated for the right problem… 5 6 1 11/21/2019 Topical therapy Normal epidermal anatomy Questions/Objectives ◦When & Why is topical therapy a useful Formation of stratum corneum & tool cornified cell envelope Extrusion of lamellar granules ◦Allergy (ceramides, cholesterol, ◦Infections free fatty acids) ◦Parasites Lipid production (lamellar granules) ◦Keratinization defects Keratin production Proliferative stem cells ◦Many others Cell layers of the epidermis. From Muller & Kirk’s Small Animal Dermatology. We have access! Modified from Proksch E Folster-Holst R, Brautigam M et al : Role of the epidermal barrier in atopic dermatitis. J Dtsch Dermatol Ges 7:899-910 Fig. 2. p901 7 8 Normal epidermal anatomy Formation of stratum corneum & cornified cell envelope Extrusion of lamellar granules (ceramides, cholesterol, free fatty acids) Lipid production (lamellar granules) Keratin production Proliferative stem cells Cell layers of the epidermis. -
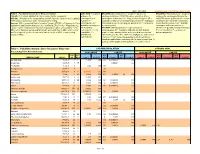
Table 1. Prioritized Chronic Dose-Response Values for Screening Risk Assessments
Date: 6/18/2018 Revisions since 5/9/2014 are shown in red. Table 1. Prioritized Chronic Dose-Response Values. IARC WOE = weight of EPA WOE (2005 Guidelines) = weight of evidence for EPA WOE (1986 Guidelines) = weight of CAS NO. = Chemical Abstracts Services number for the compound. evidence for carcinogenicity under 2005 EPA cancer guidelines (CH = evidence for carcinogenicity under the HAP NO. = Position of the compound on the HAP list in the Clean Air Act (112[b][2]). carcinogenicity in carcinogenic to humans; LH = likely to be carcinogenic; SE = 1986 EPA cancer guidelines (A = human "999" denotes substances under consideration for listing. humans (1 = suggestive evidence of carcinogenic potential; InI = inadequate carcinogen; B1 = probable carcinogen, Sources: IRIS = Integrated Risk Information System; ATSDR = US Agency for Toxic carcinogenic; 2A = information to assess carcinogenic potential; NH = not likely to limited human evidence; B2 = probable Substances and Disease Registry; CAL = California EPA; P-CAL = Proposed CAL; probably carcinogenic; be carcinogenic). carcinogen, sufficient evidence in HEAST = EPA Health Effects Assessment Summary Tables; EPA-OAQPS = EPA 2B = possibly EPA MOA (2005 Guidelines) = mode of action for animals; C = possible human carcinogen; Office of Air Quality Planning and Standards; EPA-ORD = EPA Office of Research carcinogenic; 3 = not carcinogenicity. M = mutagenic and early life data lacking; D = not classifiable; E = evidence of and Development (preferred consensus values not yet on IRIS, or superseding classifiable; 4 = m-rpf = relative potency factors were used to derive unit risk noncarcinogenicity). values on IRIS) probably not values based on the cancer risk of benzo[a]pyrene as the index carcinogenic). -

Selenium Compounds Are Federal Hazardous Air Pollutants and Were Identified As Toxic Air Contaminants in April 1993 Under AB 2728
SELENIUM COMPOUNDS Selenium compounds are federal hazardous air pollutants and were identified as toxic air contaminants in April 1993 under AB 2728. CAS Registry Number of Selenium: 7782-49-2 Se Selenium monosulfide: 7446-34-6 SeS Molecular Formula of Selenium: Se Selenium monosulfide: SSe Elemental selenium exists in several allotropic forms. The amorphous form is either red in powder form, or black in vitreous form. The crystalline monoclinic prism form is deep red and the black crystalline hexagonal form (the most stable variety) is a lustrous metallic gray. Selenium is odorless and insoluble in water and alcohol, but soluble in chloroform, methylene iodide, benzene, quinoline, nitric acid, sulfuric acid, ether, carbon disulfide, aqueous potassium cyanide and potassium sulfate solutions (HSDB, 1991; Sax, 1989). Selenium possesses photovoltaic (converts radiant energy to electrical energy) and photoconductive (where electrical resistance decreases with increased illumination) properties. There are six isotopes (Merck, 1989). The properties of selenium compounds vary with the individual selenium compound. Selenium sulfide is the only selenium compound currently shown to be carcinogenic in animals. It is a bright orange powder which emits toxic fumes of selenium and sulfur oxides when heated to decomposition (Sax, 1989). It is soluble in benzene and carbon disulfide. Examples of Selenium Compounds Selenic acid Selenium dioxide Selenourea Seleninyl bis(dimethylamide) Selenium hexafluoride Selsun Seleninyl bromide Selenium monosulfide -

Analysis of US FDA-Approved Drugs Containing Sulfur Atoms
Top Curr Chem (Z) (2018) 376:5 https://doi.org/10.1007/s41061-018-0184-5 REVIEW Analysis of US FDA‑Approved Drugs Containing Sulfur Atoms Kevin A. Scott1,2 · Jon T. Njardarson1 Received: 20 November 2017 / Accepted: 5 January 2018 / Published online: 22 January 2018 © Springer International Publishing AG, part of Springer Nature 2018 Abstract In this review, we discuss all sulfur-containing FDA-approved drugs and their structures. The second section of the review is dedicated to structural analy- sis and is divided into 14 subsections, each focusing on one type of sulfur-contain- ing moiety. A concise graphical representation of each class features drugs that are organized on the basis of structural similarity, evolutionary relevance, and medical indication. This review ofers a unique and comprehensive overview of the struc- tural features of all sulfur-containing FDA-approved drugs to date. Keywords Sulfonamide · Thioether · Sulfoxide · Sulfone · Sulfate · Sulfur heterocycle Abbreviations 6-APA 6-Aminopenicillanic acid ADP Adenosine diphosphate cGMP Cyclic guanosine monophosphate COX-2 Cyclooxygenase-2 GERD Gastroesophageal refux disease GPCR G protein-coupled receptor HIV Human immunodefciency virus mRNA Messenger RNA NSAID Nonsteroidal anti-infammatory drugs SMN1 Survival motor neuron 1 This article is part of the Topical Collection “Sulfur Chemistry”, edited by Xuefeng Jiang. * Jon T. Njardarson [email protected] 1 Department of Chemistry and Biochemistry, University of Arizona, Tucson, AZ 85721, USA 2 Department of Pharmacology -

350 Part 524—Ophthalmic And
§ 522.2690 21 CFR Ch. I (4–1–20 Edition) (3) Steers fed in confinement for slaugh- PART 524—OPHTHALMIC AND TOP- ter—(i) Amount. 72 mg zeranol (one im- ICAL DOSAGE FORM NEW ANI- plant consisting of 6 pellets, each pel- MAL DRUGS let containing 12 mg zeranol) per im- plant dose. Sec. (ii) Indications for use. For increased 524.86 Amitraz. rate of weight gain and improved feed 524.154 Bacitracin, neomycin, and poly- efficiency. myxin B ophthalmic ointment. (iii) Limitations. Implant 524.155 Bacitracin, neomycin, polymyxin B, subcutaneously in ear only. Safety and and hydrocortisone ophthalmic oint- ment. effectiveness have not been established 524.390 Chloramphenicol ophthalmic oint- in veal calves. A withdrawal period has ment. not been established for this product in 524.402 Chlorhexidine. preruminating calves. Do not use in 524.450 Clotrimazole. calves to be processed for veal. 524.463 Copper naphthenate. (4) Pasture cattle (slaughter, stocker, 524.575 Cyclosporine ophthalmic ointment. feeder steers, and heifers)—(i) Amount. 524.590 Diclofenac. 524.660 Dimethyl sulfoxide. 138 mg zeranol (one implant consisting 524.770 Doramectin. of 7 pellets, each of 6 pellets containing 524.775 Emodepside and praziquantel. 20 mg zeranol and a seventh pellet con- 524.802 Enrofloxacin and silver sulfadiazine taining 18 mg zeranol) per implant otic emulsion. dose. 524.814 Eprinomectin. (ii) Indications for use. For increased 524.815 Eprinomectin and praziquantel. rate of weight gain. 524.900 Famphur. 524.920 Fenthion. (iii) Limitations. Implant 524.955 Florfenicol, terbinafine, and subcutaneously in ear only. Safety and betamethasone acetate otic gel. effectiveness have not been established 524.957 Florfenicol, terbinafine, and in veal calves.