The Management of Common Skin Conditions in General Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Where Does Psoriasis Fit
Dr Shan Edwards Dermatologist Dermatology Clinic, Christchurch 11:00 - 11:55 WS #86: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? 12:05 - 13:00 WS #97: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? (Repeated) Differential diagnosis based on classic location Where does psoriasis fit in? Dr Shan Edwards , dermatologist Christchurch 2016 2 Conflict statement . This talk sponsored by LEO Pharma Pty Ltd . I have no other association financial or otherwise with LEO Pharma Pty Ltd 3 Acknowedgement I wish to thank and acknowledge and thank A/Prof Amanda Oakley for providing a lot of the material and allowing me to use it in this talk I would also like to acknowledge Dermnet NZ as a source for most of my clinical slides 4 How do you diagnose red scaly skin ? Take a history (90% diagnosis made on history) . When did scaly rash first appear? . What do you think caused it? . What treatments used and their effects? . Personal history of skin problems ? . Family history of similar disorders? . Occupation, hobbies, other life events? . Symptoms: itch? Other eg fever, weightloss unwell Other medical problems?(co-morbidities) . Current medicines : how long, any new ? 7 When did scaly rash first appear? . Infancy: seborrhoeic dermatitis/eczema . Toddler: atopic dermatitis/eczema . Pre-schooler/primary school: tinea capitis/corporis . Primary school: head lice . Teenage/adult: seborrhoeic dermatitis/eczema, psoriasis . Adult/elderly: drug rash, lymphoma, other less common skin conditions(PRP,Lupus) . All age groups:scabies 8 Dear Shan Re: Miss EM age 7yrs I am completely puzzled by EM’s rash and particularly so since there now appear to be other areas of her body being affected by it. -

Cutaneous Manifestations of COVID-19: a Systematic Review and Analysis of Individual Patient-Level Data
Volume 26 Number 12| December 2020 Dermatology Online Journal || Review 26(12):2 Cutaneous manifestations of COVID-19: a systematic review and analysis of individual patient-level data David S Lee1 MD, Paradi Mirmirani2,3 MD, Patrick E McCleskey4 MD, Majid Mehrpouya5 PhD, Farzam Gorouhi6,7 MD Affiliations: 1Department of Dermatology, The Permanente Medical Group, Pleasanton, California, USA, 2Department of Dermatology, University of California, San Francisco, California, USA, 3Department of Dermatology, The Permanente Medical Group, Vallejo, California, USA, 4Department of Dermatology, The Permanente Medical Group, Oakland, California, USA, 5Faculty of Engineering, University of Calgary, Calgary, Alberta, Canada, 6Department of Dermatology, The Permanente Medical Group, South Sacramento, California, USA, 7Department of Dermatology, University of California, Davis, California, USA Corresponding Author: Farzam Gorouhi MD FAAD, Kaiser Permanente, South Sacramento, 6600 Bruceville Road, Sacramento, CA 95823, Tel: 415-298-1345, Email: [email protected] Introduction Abstract In December 2019, reports from Wuhan, China Distinctive patterns in the cutaneous manifestations described new clusters of patients with severe of COVID-19 have been recently reported. We pneumonia linked to a novel coronavirus strain, now conducted a systematic review to identify case reports and case series characterizing cutaneous referred to as severe acute respiratory syndrome manifestations of confirmed COVID-19. Key coronavirus 2 (SARS-CoV-2), [1]. Coronavirus disease demographic and clinical data from each case were 2019 (COVID-19) has since reached pandemic extracted and analyzed. The primary outcome proportions, with over 12·7 million cases worldwide, measure was risk factor analysis of skin related 566,000 deaths, and 188 countries affected at the outcomes for severe COVID-19 disease. -

This Fact Sheet Provides Information to Patients with Eczema and Their Carers. About Topical Corticosteroids How to Apply Topic
This fact sheet provides information to patients with eczema and their carers. About topical corticosteroids You or your child’s doctor has prescribed a topical corticosteroid for the treatment of eczema. For treating eczema, corticosteroids are usually prepared in a cream or ointment and are applied topically (directly onto the skin). Topical corticosteroids work by reducing inflammation and helping to control an over-reactive response of the immune system at the site of eczema. They also tighten blood vessels, making less blood flow to the surface of the skin. Together, these effects help to manage the symptoms of eczema. There is a range of steroids that can be used to treat eczema, each with different strengths (potencies). On the next page, the potencies of some common steroids are shown, as well as the concentration that they are usually used in cream or ointment preparations. Using a moisturiser along with a steroid cream does not reduce the effect of the steroid. There are many misconceptions about the side effects of topical corticosteroids. However these treatments are very safe and patients are encouraged to follow the treatment regimen as advised by their doctor. How to apply topical corticosteroids How often should I apply? How much should I apply? Apply 1–2 times each day to the affected area Enough cream should be used so that the of skin according to your doctor’s instructions. entire affected area is covered. The cream can then be rubbed or massaged into the Once the steroid cream has been applied, inflamed skin. moisturisers can be used straight away if needed. -
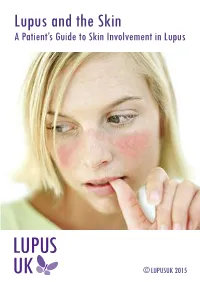
Lupus and the Skin a Patient’S Guide to Skin Involvement in Lupus
Lupus and the Skin A Patient’s Guide to Skin Involvement in Lupus © LUPUSUK 2015 LUPUS and the Skin LUPUS UK acknowledges with gratitude the assistance of Sue Brown, Consultant Nurse in Rheumatology (Connective Tissue Diseases), Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath and Dr Chris Lovell, Consultant Dermatologist, Royal United Hospital and Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath in the provision of clinical information towards the production of this booklet. ACKNOWLEDGEMENT The authors would like to thank Professor Peter Maddison, Consultant Rheumatologist and Dr Andrew Macfarlane, Consultant Dermatologist at Ysbyty Gwynedd, Bangor, Wales, who wrote the first edition of this booklet and have kindly agreed to its revision. LUPUS UK is the national charity caring for those with systemic lupus erythematosus (SLE) and discoid lupus erythematosus (DLE), supporting people as they develop the symptoms prior to diagnosis and those already diagnosed. You can help by taking up membership For more information contact: LUPUS UK, St James House, Eastern Road, Romford, Essex RM1 3NH Tel: 01708 731251 www.lupusuk.org.uk Reg. charity nos 1051610, SC039682 © LUPUS UK 2012 All rights reserved. No part of this book may be reproduced in any form without written permission from LUPUS UK. Index Section Page No 1 Introduction 1 2 Types of rashes 2 3 Mechanism of photosensitivity 5 4 Treatment of the skin in lupus 7 5 Sun protection 10 6 Quality of life 11 7 Fatigue 12 8 Self help 12 9 Research 14 10 Further reading 14 1. Introduction Many people with lupus may have skin problems, and a rash may be the first sign of the condition. -

New Insights Into the Effect of Amorolfine Nail Lacquer
Review article New insights into the effect of amorolfine nail lacquer C. Flagothier, C. Pie´ rard-Franchimont and G. E. Pie´ rard Department of Dermatopathology, University Hospital of Lie`ge, Lie`ge, Belgium Summary Despite improvements in antifungal strategies, the outcome of treating onychomycoses often remains uncertain. Several factors account for treatment failure, of which the pharmacokinetics and pharmacodynamics of the antifungal are of importance. The taxonomic nature and ungual location of the fungus cannot be neglected, besides the type of nail and its growth rate. In addition, the biological cycle of the fungus and the metabolic activity of the pathogen likely play a marked influence in drug response. The presence of natural antimicrobial peptides in the nail is also probably a key feature controlling the cure rates. There are many outstanding publications that cover the full spectrum of the field. The purpose of this review is to put in perspective some facets of activity of the topical treatment using amorolfine nail laquer. The antifungal activity of the drug is likely less pronounced in onychomycosis than that expected from conventional in vitro studies. However, the nail laquer formulation should reduce the propensity to form antifungal-resistant spores and limit the risk of reinfection. Key words: amorolfine, antifungal, fungus, onychomycosis, spore. Topical treatments are often considered to be less Introduction efficacious than current oral treatments. However, some During the last 2 decades, the efficacy of treating topical formulations may provide effects that cannot be onychomycoses has been considerably improved by achieved by other treatments. In discussing the treat- the introduction of new generations of potent antifun- ment of onychomycosis, it should not be forgotten that gals. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -

Scalp Eczema Factsheet the Scalp Is an Area of the Body That Can Be Affected by Several Types of Eczema
12 Scalp eczema factsheet The scalp is an area of the body that can be affected by several types of eczema. The scalp may be dry, itchy and scaly in a chronic phase and inflamed (red), weepy and painful in an acute (eczema flare) phase. Aside from eczema, there are a number of reasons why the scalp can become dry and itchy (e.g. psoriasis, fungal infection, ringworm, head lice etc.), so it is wise to get a firm diagnosis if there is uncertainty. Types of eczema • Hair clips and headgear – especially those containing that affect the scalp rubber or nickel. Seborrhoeic eczema (dermatitis) is one of the most See the NES booklet on Contact Dermatitis for more common types of eczema seen on the scalp and hairline. details. It can affect babies (cradle cap), children and adults. The Irritant contact dermatitis is a type of eczema that skin appears red and scaly and there is often dandruff as occurs when the skin’s surface is irritated by a substance well, which can vary in severity. There may also be a rash that causes the skin to become dry, red and itchy. on other parts of the face, such as around the eyebrows, For example, shampoos, mousses, hair gels, hair spray, eyelids and sides of the nose. Seborrhoeic eczema can perm solution and fragrance can all cause irritant contact become infected. See the NES factsheets on Adult dermatitis. See the NES booklet on Contact Dermatitis for Seborrhoeic Dermatitis and Infantile Seborrhoeic more details. Dermatitis and Cradle Cap for more details. -

Autoinvolutive Photoexacerbated Tinea Corporis Mimicking a Subacute Cutaneous Lupus Erythematosus
Letters to the Editor 141 low-potency steroids had no eŒect. Our patient was treated 4. Jarrat M, Ramsdell W. Infantile acropustulosis. Arch Dermatol with a modern glucocorticoid which has an improved risk– 1979; 115: 834–836. bene t ratio. The antipruritic and anti-in ammatory properties 5. Kahn G, Rywlin AM. Acropustulosis of infancy. Arch Dermatol of the steroid were increased by applying it in combination 1979; 115: 831–833. 6. Newton JA, Salisbury J, Marsden A, McGibbon DH. with a wet-wrap technique, which has already been shown to Acropustulosis of infancy. Br J Dermatol 1986; 115: 735–739. be extremely helpful in cases of acute exacerbations of atopic 7. Mancini AJ, Frieden IJ, Praller AS. Infantile acropustulosis eczema in combination with (3) or even without topical revisited: history of scabies and response to topical corticosteroids. steroids (8). Pediatr Dermatol 1998; 15: 337–341. 8. Abeck D, Brockow K, Mempel M, Fesq H, Ring J. Treatment of acute exacerbated atopic eczema with emollient-antiseptic prepara- tions using ‘‘wet-wrap’’ (‘‘wet-pyjama’’) technique. Hautarzt 1999; REFERENCES 50: 418–421. 1. Vignon-Pennam en M-D, Wallach D. Infantile acropustulosis. Arch Dermatol 1986; 122: 1155–1160. Accepted November 24, 2000. 2. Duvanel T, Harms M. Infantile Akropustulose. Hautarzt 1988; 39: 1–4. Markus Braun-Falco, Silke Stachowitz, Christina Schnopp, Johannes 3. Oranje AP, Wolkerstorfer A, de Waard-van der Spek FB. Treatment Ring and Dietrich Abeck of erythrodermic atopic dermatitis with ‘‘wet-wrap’’ uticasone Klinik und Poliklinik fu¨r Dermatologie und Allergologie am propionate 0,05% cream/emollient 1:1 dressing. -

Cytomegalovirus Infection Associated with Portal Vein Thrombosis and Thrombocytopenia: a Case Report
MÉDECINE INTERNE Cytomegalovirus infection associated with portal vein thrombosis and thrombocytopenia: a case report Gianfranco Di Prinzio1, Phung Nguyen Ung2, Anne-Sophie Valschaerts2, Olivier Borgniet2 CMV et Thrombose : We here present the case of portal vein thrombosis in a patient exhibiting symptoms of cytomegalovirus infection, confirmed by un binome sous-estimé serology and polymerase chain reaction (PCR) and complicated by Le Cytomegalovirus (CMV) est thrombocytopenia. The literature reveals growing evidence that responsable d’une infection virale human CMV likely plays a role in thrombotic disorders. However, commune et souvent banale chez le only 11 cases of CMV-induced visceral venous thrombosis have been sujet immunocompétent, mais qui described so far. On the other hand, thrombocytopenia is a well- n’est pas dépourvue de complications potentiellement graves. La thrombose known complication of CMV infection. The patient was successfully porte en est un exemple. Le cas que treated using high-dose immunoglobulins by intravenous route. nous décrivons concerne une patiente atteinte d’une infection à CMV, s’étant révélée par une éruption cutanée et s’étant compliquée d’une thrombose porte, en l’absence de thrombophilie connue. Une thrombopénie auto- A 36-year-old Caucasian woman was admitted to the emergency room immune est la seconde complication of our hospital, complaining since several days of sore throat, cough, survenue dans notre cas. Cet article a pour but de souligner l’enjeu d’un tel fever, headache, and rhinorrhea. She had been unsuccessfully treated diagnostic et de stimuler la réflexion sur with amoxicillin-clavulanate during the week preceding her admission. l’intérêt du dépistage échographique The medication was stopped owing to gastric intolerance. -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020
First independent framework for assessing pharmaceutical company action Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020 ACKNOWLEDGEMENTS The Access to Medicine Foundation would like to thank the following people and organisations for their contributions to this report.1 FUNDERS The Antimicrobial Resistance Benchmark research programme is made possible with financial support from UK AID and the Dutch Ministry of Health, Welfare and Sport. Expert Review Committee Research Team Reviewers Hans Hogerzeil - Chair Gabrielle Breugelmans Christine Årdal Gregory Frank Fatema Rafiqi Karen Gallant Nina Grundmann Adrián Alonso Ruiz Hans Hogerzeil Magdalena Kettis Ruth Baron Hitesh Hurkchand Joakim Larsson Dulce Calçada Joakim Larsson Marc Mendelson Moska Hellamand Marc Mendelson Margareth Ndomondo-Sigonda Kevin Outterson Katarina Nedog Sarah Paulin (Observer) Editorial Team Andrew Singer Anna Massey Deirdre Cogan ACCESS TO MEDICINE FOUNDATION Rachel Jones The Access to Medicine Foundation is an independent Emma Ross non-profit organisation based in the Netherlands. It aims to advance access to medicine in low- and middle-income Additional contributors countries by stimulating and guiding the pharmaceutical Thomas Collin-Lefebvre industry to play a greater role in improving access to Alex Kong medicine. Nestor Papanikolaou Address Contact Naritaweg 227-A For more information about this publication, please contact 1043 CB, Amsterdam Jayasree K. Iyer, Executive Director The Netherlands [email protected] +31 (0) 20 215 35 35 www.amrbenchmark.org 1 This acknowledgement is not intended to imply that the individuals and institutions referred to above endorse About the cover: Young woman from the Antimicrobial Resistance Benchmark methodology, Brazil, where 40%-60% of infections are analyses or results. -

Treatment of Diseases and Conditions Mediated By
(19) TZZ_ ___T (11) EP 1 572 115 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 38/07 (2006.01) A61K 38/08 (2006.01) 21.01.2015 Bulletin 2015/04 A61K 38/17 (2006.01) A61K 38/38 (2006.01) (21) Application number: 03799853.1 (86) International application number: PCT/US2003/037901 (22) Date of filing: 25.11.2003 (87) International publication number: WO 2004/050023 (17.06.2004 Gazette 2004/25) (54) TREATMENT OF DISEASES AND CONDITIONS MEDIATED BY INCREASED PHOSPHORYLATION BEHANDLUNG VON ERKRANKUNGEN UND ZUSTÄNDEN,DIE DURCH ERHÖHTE PHOSPHORYLIERUNG VERMITTELT WERDEN TRAITEMENT DE MALADIES ET D’ETATS A MEDIATION DE PHOSPHORYLATION ACCRUE (84) Designated Contracting States: • JIANG B ET AL: "Phosphopeptides derived from AT BE BG CH CY CZ DE DK EE ES FI FR GB GR hen egg yolk phosvitin: effect of molecular size HU IE IT LI LU MC NL PT RO SE SI SK TR on the calcium-binding properties." BIOSCIENCE, BIOTECHNOLOGY, AND (30) Priority: 27.11.2002 US 429924 P BIOCHEMISTRY MAY 2001, vol. 65, no. 5, May 2001 (2001-05), pages 1187-1190, XP002549556 (43) Date of publication of application: ISSN: 0916-8451 14.09.2005 Bulletin 2005/37 • KATAYAMA SHIGERU ET AL: "Antioxidative stress activity of oligophosphopeptides derived (73) Proprietor: Ampio Pharmaceuticals, Inc. from hen egg yolk phosvitin in Caco-2 cells." Englewood, CO 80112 (US) JOURNAL OF AGRICULTURAL AND FOOD CHEMISTRY 8 FEB 2006, vol. 54, no. 3, 8 February (72) Inventor: BAR-OR, David 2006 (2006-02-08), pages 773-778, XP002549557 Englewood, CO 80110 (US) ISSN: 0021-8561 • OKAMOTO ET AL: ’The interleukin-8 AP-1 and (74) Representative: Weber, Joachim kappa B-like sites are genetic end targets of Hoefer & Partner FK506-sensitive pathway accompanied by Patentanwälte calcium mobilization.’ JOURNAL OF Pilgersheimer Strasse 20 BIOLOGICAL CHEMISTRY vol.