Seniors Delirium Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients Research Questions: 1. How many schizophrenia patients are prescribed recommended first-line second-generation treatments for schizophrenia? 2. How many schizophrenia patients switch to an injectable antipsychotic after stabilization on an oral antipsychotic? 3. How many schizophrenia patients are prescribed 2 or more concomitant antipsychotics? 4. Are claims for long-acting injectable antipsychotics primarily billed as pharmacy or physician administered claims? 5. Does adherence to antipsychotic therapy differ between patients with claims for different routes of administration (oral vs. long-acting injectable)? Conclusions: In total, 4663 schizophrenia patients met inclusion criteria, and approximately 14% of patients (n=685) were identified as treatment naïve without claims for antipsychotics in the year before their first antipsychotic prescription. Approximately 45% of patients identified as treatment naïve had a history of remote antipsychotic use, but it is unclear if antipsychotics were historically prescribed for schizophrenia. Oral second-generation antipsychotics which are recommended as first-line treatment in the MHCAG schizophrenia algorithm were prescribed as initial treatment in 37% of treatment naive patients and 28% of all schizophrenia patients. Recommended agents include risperidone, paliperidone, and aripiprazole. Utilization of parenteral antipsychotics was limited in patients with schizophrenia. Overall only 8% of patients switched from an oral to an injectable therapy within 6 months of their first claim. Approximately, 60% of all schizophrenia patients (n=2512) had claims for a single antipsychotic for at least 12 continuous weeks and may be eligible to transition to a long-acting injectable antipsychotic. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Inhaled Loxapine Monograph
Inhaled Loxapine Monograph Inhaled Loxapine (ADASUVE) National Drug Monograph February 2015 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Inhaled loxapine is a typical antipsychotic used in the treatment of acute Action agitation associated with schizophrenia and bipolar I disorder in adults. Loxapine’s mechanism of action for reducing agitation in schizophrenia and bipolar I disorder is unknown. Its effects are thought to be mediated through blocking postsynaptic dopamine D2 receptors as well as some activity at the serotonin 5-HT2A receptors. Indication(s) Under Review in Inhaled loxapine is a typical antipsychotic indicated for the acute treatment of this document (may include agitation associated with schizophrenia or bipolar I disorder in adults. off label) Off-label use Agitation related to any other cause not due to schizophrenia and bipolar I disorder. Dosage Form(s) Under 10mg oral inhalation using a new STACCATO inhaler device. Review REMS REMS No REMS Post-marketing Study Required See Other Considerations for additional REMS information Pregnancy Rating C Executive Summary Efficacy Inhaled loxapine was superior to placebo in reducing acute agitation at 2 hours post dose measured by the Positive and Negative Syndrome Scale-Excited Component (PEC) in patients with bipolar I disorder and schizophrenia. -

Should Inverse Agonists Be Defined by Pharmacological Mechanism Or
CNS Spectrums,(2019), 24 419 – 425. © Cambridge University Press 2018. This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. doi:10.1017/S1092852918000986 ORIGINAL RESEARCH Switching stable patients with schizophrenia from their oral antipsychotics to aripiprazole lauroxil: a post hoc safety analysis of the initial 12-week crossover period Peter J. Weiden,1* Yangchun Du,2 Chih-Chin Liu,2 and Arielle D. Stanford3 1 Medical Affairs, Alkermes, Inc., Waltham, Massachusetts, USA 2 Clinical Development, Alkermes, Inc., Waltham, Massachusetts, USA 3 Clinical Science, Alkermes, Inc., Waltham, Massachusetts, USA Objective. Switching antipsychotic medications is common in patients with schizophrenia who are experiencing persistent symptoms or tolerability issues associated with their current drug regimen. This analysis assessed the safety of switching from an oral antipsychotic to the long-acting injectable antipsychotic aripiprazole lauroxil (AL). Methods. This was a post hoc analysis of outpatients with schizophrenia who were prescribed an oral antipsychotic and who enrolled in an international, open-label, long-term (52-week) safety study of AL. The analysis focused on the first 3 injections of AL 882 mg over 12 weeks, divided into the immediate 4-week crossover period between the first and second AL injections (initiation phase) and the subsequent 8 weeks (stabilization phase). Patients were grouped by preswitch oral antipsychotic medication, and safety and clinical symptoms were assessed. Results. In total, 190 patients had switched from one of the following oral antipsychotic medications: aripiprazole, conventional antipsychotics, risperidone/paliperidone, olanzapine, or quetiapine. -

Advice on Prescribing for Adults with Obsessive-Compulsive Disorder (OCD)
Advice on Prescribing for Adults with Obsessive-Compulsive Disorder (OCD) Dr Lynne M Drummond, Local and National OCD Services, Behavioural and Cognitive Psychotherapy Unit, South West London and St George’s Menat Health NHS Trust 9th April 2008 Introduction Obsessive-Compulsive Disorder (OCD) is a common psychiatric disorder which untreated has a chronic often deteriorating course. OCD does respond well to treatment with either psychological approaches involving Graded Exposure and Self-Imposed Ritual Prevention (ERP) or with specific pharmacological agents. This paper aims to outline the various psychopharmacological approaches. Psychopharmacological approaches Repeated trials have demonstrated that drugs which act of the serotonin system are effective in many patients with OCD (SRI and SSRIs) • The Selective Serotonin Reuptake Inhibitors (SSRIs) are generally used as first line rather than clomipramine (a Serotonin Reuptake Inhibitor- SRI) due to fewer side effects. • There is little evidence of any particular advantage of any of the SSRIs apart from some evidence that Escitalopram* may reduce relapse of OCD. • In general if there is no response to the SRI on maximal doses for 12 weeks it is worthwhile switching to an alternative. • However there is evidence that benefit from SRI can accrue over as long as 2 years Drug Dose Major side effects Any special features Seizures in a small number of patients The first SRI to and less likely if demonstrate Clomipramine Up to 225mg at <250mg effectiveness in night (increase reducing OCD slowly as tolerated) Sexual Dysfunction symptoms in 80 % Dry mouth; blurred It is a tricyclic vision drowsiness; antidepressant weight gain and orthostatic hypotension 1 50 mg in evening Gastro-intestinal initially and upsets; anorexia and increased weight loss. -

Decrease in Brain Serotonin 2 Receptor Binding In
ORIGINAL ARTICLE Decrease in Brain Serotonin 2 Receptor Binding in Patients With Major Depression Following Desipramine Treatment A Positron Emission Tomography Study With Fluorine-18–Labeled Setoperone Lakshmi N. Yatham, MBBS, FRCPC; Peter F. Liddle, PhD, MBBS; Joelle Dennie, MSc; I-Shin Shiah, MD; Michael J. Adam, PhD; Carol J. Lane, MSc; Raymond W. Lam, MD; Thomas J. Ruth, PhD Background: The neuroreceptor changes involved in Results: Eight of the 10 patients responded to desipra- therapeutic efficacy of various antidepressants remain un- mine treatment as indicated by more than 50% decrease clear. Preclinical studies have shown that long-term ad- in Hamilton Depression Rating Scale scores. Depressed ministration of various antidepressants causes down- patients showed a significant decrease in 5-HT2 recep- regulation of brain serotonin 2 (5-HT2) receptors in rodents, tor binding as measured by setoperone binding in fron- but it is unknown if similar changes occur following anti- tal, temporal, parietal, and occipital cortical regions fol- depressant treatment in depressed patients. Our purpose, lowing desipramine treatment. The decrease in 5-HT2 therefore, was to assess the effects of treatment with desi- receptor binding was observed bilaterally and was par- pramine hydrochloride on brain 5-HT2 receptors in de- ticularly prominent in frontal cortex. pressed patients using positron emission tomography (PET) and fluorine-18 (18F)–labeled setoperone. Conclusions: Depressed patients showed a significant reduction in available 5-HT2 receptors in the brain fol- Methods: Eleven patients who met DSM-IV criteria for lowing desipramine treatment, but it is unknown if this major depression as determined by a structured clinical change in 5-HT2 receptors is due to clinical improve- interview for DSM-III-R diagnosis and suitable for treat- ment or an effect of desipramine that is unrelated to clini- ment with desipramine were recruited. -

CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (Also Belong to Psychiatric Medication Category) • Codeine (In 222® Tablets, Tylenol® No
CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (also belong to psychiatric medication category) • codeine (in 222® Tablets, Tylenol® No. 1/2/3/4, Fiorinal® C, Benzodiazepines Codeine Contin, etc.) • heroin • alprazolam (Xanax®) • hydrocodone (Hycodan®, etc.) • chlordiazepoxide (Librium®) • hydromorphone (Dilaudid®) • clonazepam (Rivotril®) • methadone • diazepam (Valium®) • morphine (MS Contin®, M-Eslon®, Kadian®, Statex®, etc.) • flurazepam (Dalmane®) • oxycodone (in Oxycocet®, Percocet®, Percodan®, OxyContin®, etc.) • lorazepam (Ativan®) • pentazocine (Talwin®) • nitrazepam (Mogadon®) • oxazepam ( Serax®) Alcohol • temazepam (Restoril®) Inhalants Barbiturates • gases (e.g. nitrous oxide, “laughing gas”, chloroform, halothane, • butalbital (in Fiorinal®) ether) • secobarbital (Seconal®) • volatile solvents (benzene, toluene, xylene, acetone, naptha and hexane) Buspirone (Buspar®) • nitrites (amyl nitrite, butyl nitrite and cyclohexyl nitrite – also known as “poppers”) Non-Benzodiazepine Hypnotics (also belong to psychiatric medication category) • chloral hydrate • zopiclone (Imovane®) Other • GHB (gamma-hydroxybutyrate) • Rohypnol (flunitrazepam) CENTRAL NERVOUS SYSTEM STIMULANTS Amphetamines Caffeine • dextroamphetamine (Dexadrine®) Methelynedioxyamphetamine (MDA) • methamphetamine (“Crystal meth”) (also has hallucinogenic actions) • methylphenidate (Biphentin®, Concerta®, Ritalin®) • mixed amphetamine salts (Adderall XR®) 3,4-Methelynedioxymethamphetamine (MDMA, Ecstasy) (also has hallucinogenic actions) Cocaine/Crack -

Beyond Amitriptyline
children Review Beyond Amitriptyline: A Pediatric and Adolescent Oriented Narrative Review of the Analgesic Properties of Psychotropic Medications for the Treatment of Complex Pain and Headache Disorders Robert Blake Windsor 1,2,*, Michael Sierra 2,3, Megan Zappitelli 2,3 and Maria McDaniel 1,2 1 Division of Pediatric Pain Medicine, Department of Pediatrics, Prisma Health, Greenville, SC 29607, USA; [email protected] 2 School of Medicine Greenville, University of South Carolina, Greenville, SC 29607, USA; [email protected] (M.S.); [email protected] (M.Z.) 3 Division of Child and Adolescent Psychiatry, Department of Psychiatry, Prisma Health, Greenville, SC 29607, USA * Correspondence: [email protected] Received: 30 October 2020; Accepted: 25 November 2020; Published: 2 December 2020 Abstract: Children and adolescents with recurrent or chronic pain and headache are a complex and heterogenous population. Patients are best served by multi-specialty, multidisciplinary teams to assess and create tailored, individualized pain treatment and rehabilitation plans. Due to the complex nature of pain, generalizing pharmacologic treatment recommendations in children with recurrent or chronic pains is challenging. This is particularly true of complicated patients with co-existing painful and psychiatric conditions. There is an unfortunate dearth of evidence to support many pharmacologic therapies to treat children with chronic pain and headache. This narrative review hopes to supplement the available treatment options for this complex population by reviewing the pediatric and adult literature for analgesic properties of medications that also have psychiatric indication. The medications reviewed belong to medication classes typically described as antidepressants, alpha 2 delta ligands, mood stabilizers, anti-psychotics, anti-sympathetic agents, and stimulants. -

Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gutlbrain Interaction): a Rome Foundation Working Team Report Douglas A
Gastroenterology 2018;154:1140–1171 SPECIAL REPORT Neuromodulators for Functional Gastrointestinal Disorders (Disorders of GutLBrain Interaction): A Rome Foundation Working Team Report Douglas A. Drossman,1,2 Jan Tack,3 Alexander C. Ford,4,5 Eva Szigethy,6 Hans Törnblom,7 and Lukas Van Oudenhove8 1Center for Functional Gastrointestinal and Motility Disorders, University of North Carolina, Chapel Hill, North Carolina; 2Center for Education and Practice of Biopsychosocial Care and Drossman Gastroenterology, Chapel Hill, North Carolina; 3Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium; 4Leeds Institute of Biomedical and Clinical Sciences, University of Leeds, Leeds, United Kingdom; 5Leeds Gastroenterology Institute, St James’s University Hospital, Leeds, United Kingdom; 6Departments of Psychiatry and Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania; 7Departments of Internal Medicine and Clinical Nutrition, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; and 8Laboratory for BrainÀGut Axis Studies, Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium BACKGROUND & AIMS: Central neuromodulators (antide- summary information and guidelines for the use of central pressants, antipsychotics, and other central nervous neuromodulators in the treatment of chronic gastrointestinal systemÀtargeted medications) are increasingly used for treat- symptoms and FGIDs. Further studies are needed to confirm ment -

Schizophrenia Or Bipolar Disorder
Appendix D- NICE’s response to consultee and commentator comments on the draft scope and provisional matrix National Institute for Health and Clinical Excellence Proposed Single Technology Appraisal (STA) Loxapine inhalation for the treatment of acute agitation and disturbed behaviours associated with schizophrenia or bipolar disorder Response to consultee and commentator comments on the draft remit and draft scope (pre-referral) Comment 1: the draft remit Section Consultees Comments Action Appropriateness Alexza Yes as this topic is relevant to New Horizons: A Shared Vision for Mental Health Comment noted. No Pharmaceuticals (2009)1 and to The National Service Framework for Mental Health: Modern action required. Standards and Service Models (1999).2 Royal College of The appraisal of use of alternative matrices for drug delivery is important. It is Comment noted. No Pathologists particularly important in situation where there may be difficulties in administering action required. traditional drugs via intramuscular or intravenous routes. Therefore this worthy of NICE appraisal. Royal College of It is appropriate to consider novel methods to administer medications for this Comment noted. No Nursing condition. action required. Wording Alexza Revise to: Comment noted. Pharmaceuticals To appraise the clinical and cost effectiveness of Staccato® loxapine within the Consultees agreed that licensed indication for the rapid control of agitation and disturbed behaviors in the draft remit should patients with schizophrenia or in patients with bipolar -

Endoscopic Treatment of Pharmacobezoar Caused by Slow-Release Clomipramine and Quetiapine Overdose
Netherlands Journal of Critical Care Submitted August 2020; Accepted January 2021 CASE REPORT Endoscopic treatment of pharmacobezoar caused by slow-release clomipramine and quetiapine overdose S.J.P. Hiel1, A. Osinski1, J.T. Kamphuis2 1Department of Intensive Care, 2Department of Gastroenterology, Maxima Medical Center, Veldhoven, the Netherlands Correspondence S.J.P. Hiel - [email protected] Keywords - slow-release clomipramine, intoxication, pharmacobezoar, endoscopy Abstract Case report A pharmacobezoar is a rare entity characterised by an An 18-year-old female known with chronic depression was accumulation of undigested pills in the gastrointestinal tract. admitted to our hospital approximately two hours after taking It is often induced by massive drug consumption, especially an overdose of tablets. She supposedly ingested 50 tablets of slow-release tablets. We describe an 18-year-old female with slow-release clomipramine 75 mg (3.75 g total) and 100 tablets a pharmacobezoar after taking an overdose of slow-release of slow-release quetiapine 25 mg (2.5 g total). She was found clomipramine and slow-release quetiapine. Because of a in a state of reduced responsiveness by her mother who called decline in her level of consciousness, she was intubated. As the emergency services. standard treatment with activated charcoal, gastric lavage On examination at the emergency department, a very thin and laxatives was insufficiently effective, it was decided patient with a body weight of 50 kg (body mass index of 17.3 to remove the tablets endoscopically. The patient did not kg/m2) was seen. Glasgow coma scale (GCS) was E3-M5-V3. have any post-procedural complications and showed a full Her pupils were slightly, equally dilated and responsive to recovery. -
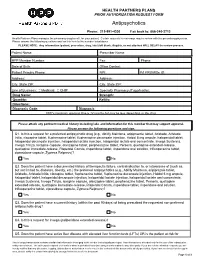
Antipsychotics
HEALTH PARTNERS PLANS PRIOR AUTHORIZATION REQUEST FORM Antipsychotics Phone: 215-991-4300 Fax back to: 866-240-3712 Health Partners Plans manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the number listed above. PLEASE NOTE: Any information (patient, prescriber, drug, labs) left blank, illegible, or not attached WILL DELAY the review process. Patient Name: Prescriber Name: HPP Member Number: Fax: Phone: Date of Birth: Office Contact: Patient Primary Phone: NPI: PA PROMISe ID: Address: Address: City, State ZIP: City, State ZIP: Line of Business: Medicaid CHIP Specialty Pharmacy (if applicable): Drug Name: Strength: Quantity: Refills: Directions: Diagnosis Code: Diagnosis: HPP’s maximum approval time is 12 months but may be less depending on the drug. Please attach any pertinent medical history including labs and information for this member that may support approval. Please answer the following questions and sign. Q1. Is this a request for a preferred antipsychotic drug (e.g., Abilify Maintena, aripiprazole tablet, Aristada, Aristada Initio, clozapine tablet, fluphenazine tablet, fluphenazine decanoate injection, Haldol 5 mg ampule, haloperidol tablet, haloperidol decanoate injection, haloperidol lactate injection, haloperidol lactate oral concentrate, Invega Sustenna, Invega Trinza, loxapine capsule, olanzapine tablet, perphenazine tablet, Perseris, quetiapine extended-release, quetiapine immediate-release,