Are You Suprised ?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Oral Microbiome of Healthy Japanese People at the Age of 90
applied sciences Article The Oral Microbiome of Healthy Japanese People at the Age of 90 Yoshiaki Nomura 1,* , Erika Kakuta 2, Noboru Kaneko 3, Kaname Nohno 3, Akihiro Yoshihara 4 and Nobuhiro Hanada 1 1 Department of Translational Research, Tsurumi University School of Dental Medicine, Kanagawa 230-8501, Japan; [email protected] 2 Department of Oral bacteriology, Tsurumi University School of Dental Medicine, Kanagawa 230-8501, Japan; [email protected] 3 Division of Preventive Dentistry, Faculty of Dentistry and Graduate School of Medical and Dental Science, Niigata University, Niigata 951-8514, Japan; [email protected] (N.K.); [email protected] (K.N.) 4 Division of Oral Science for Health Promotion, Faculty of Dentistry and Graduate School of Medical and Dental Science, Niigata University, Niigata 951-8514, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-45-580-8462 Received: 19 August 2020; Accepted: 15 September 2020; Published: 16 September 2020 Abstract: For a healthy oral cavity, maintaining a healthy microbiome is essential. However, data on healthy microbiomes are not sufficient. To determine the nature of the core microbiome, the oral-microbiome structure was analyzed using pyrosequencing data. Saliva samples were obtained from healthy 90-year-old participants who attended the 20-year follow-up Niigata cohort study. A total of 85 people participated in the health checkups. The study population consisted of 40 male and 45 female participants. Stimulated saliva samples were obtained by chewing paraffin wax for 5 min. The V3–V4 hypervariable regions of the 16S ribosomal RNA (rRNA) gene were amplified by PCR. -
The Comparison of Metronidazole, Clindamycin, and Amoxicillin Againts Streptococcus Sanguinis
Indonesian Dental Association Journal of Indonesian Dental Association http://jurnal.pdgi.or.id/index.php/jida ISSN: 2621-6183 (Print); ISSN: 2621-6175 (Online) The Comparison of Metronidazole, Clindamycin, and Amoxicillin Againts Streptococcus sanguinis Kevin Lim1, Armelia Sari Widyarman2§ 1 Undergraduate student, Faculty of Dentistry, Trisakti University, Indonesia 2 Department of Microbiology, Faculty of Dentistry, Trisakti University, Indonesia Received date: August 15, 2018. Accepted date: September 27, 2018. Published date: October 19, 2018 KEYWORDS ABSTRACT amoxicillin; Introduction: Viridans streptococci group such as Streptococcus sanguinis (S. sanguinis), an clindamycin; anaerobic Gram-positive bacteria is a well-known for its involvement in dry socket (alveolar metronidazole; Streptococcus sanguinis osteitis)-associated infection. Systemic amoxicillin, clindamycin and metronidazole have all been shown to be effective to inhibit this bacterium. However, there has been a lack of studies identifying which are the most effective amongst these antibiotics toward Streptococcus sanguinis. Objectives: The purpose of this study is to evaluate the effectiveness of metronidazole, clindamycin, and amoxicillin in inhibiting the growth of Streptococcus sanguinis in vitro. Methods: This effectiveness was done by using agar well diffusion methods. S. sanguinis ATCC 10556 were cultured in Brain Heart Infusion (BHI) broth at 37°C under anaerobic condition. After 48h, bacterial cells were harvested and counted using microplate reader (490 nm) to achieve optical density of 0.25-0.30 (107 CFU/mL). Subsequently, 100 μL of bacterial suspension was cultured on BHI agar and each antibiotic suspension was added into each agar well, incubated for 72h at 37°C. The inhibition zone diameters were measured with electronic caliper. -

Table S5. the Information of the Bacteria Annotated in the Soil Community at Species Level
Table S5. The information of the bacteria annotated in the soil community at species level No. Phylum Class Order Family Genus Species The number of contigs Abundance(%) 1 Firmicutes Bacilli Bacillales Bacillaceae Bacillus Bacillus cereus 1749 5.145782459 2 Bacteroidetes Cytophagia Cytophagales Hymenobacteraceae Hymenobacter Hymenobacter sedentarius 1538 4.52499338 3 Gemmatimonadetes Gemmatimonadetes Gemmatimonadales Gemmatimonadaceae Gemmatirosa Gemmatirosa kalamazoonesis 1020 3.000970902 4 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas indica 797 2.344876284 5 Firmicutes Bacilli Lactobacillales Streptococcaceae Lactococcus Lactococcus piscium 542 1.594633558 6 Actinobacteria Thermoleophilia Solirubrobacterales Conexibacteraceae Conexibacter Conexibacter woesei 471 1.385742446 7 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas taxi 430 1.265115184 8 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas wittichii 388 1.141545794 9 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas sp. FARSPH 298 0.876754244 10 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sorangium cellulosum 260 0.764953367 11 Proteobacteria Deltaproteobacteria Myxococcales Polyangiaceae Sorangium Sphingomonas sp. Cra20 260 0.764953367 12 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas panacis 252 0.741416341 -

Common Commensals
Common Commensals Actinobacterium meyeri Aerococcus urinaeequi Arthrobacter nicotinovorans Actinomyces Aerococcus urinaehominis Arthrobacter nitroguajacolicus Actinomyces bernardiae Aerococcus viridans Arthrobacter oryzae Actinomyces bovis Alpha‐hemolytic Streptococcus, not S pneumoniae Arthrobacter oxydans Actinomyces cardiffensis Arachnia propionica Arthrobacter pascens Actinomyces dentalis Arcanobacterium Arthrobacter polychromogenes Actinomyces dentocariosus Arcanobacterium bernardiae Arthrobacter protophormiae Actinomyces DO8 Arcanobacterium haemolyticum Arthrobacter psychrolactophilus Actinomyces europaeus Arcanobacterium pluranimalium Arthrobacter psychrophenolicus Actinomyces funkei Arcanobacterium pyogenes Arthrobacter ramosus Actinomyces georgiae Arthrobacter Arthrobacter rhombi Actinomyces gerencseriae Arthrobacter agilis Arthrobacter roseus Actinomyces gerenseriae Arthrobacter albus Arthrobacter russicus Actinomyces graevenitzii Arthrobacter arilaitensis Arthrobacter scleromae Actinomyces hongkongensis Arthrobacter astrocyaneus Arthrobacter sulfonivorans Actinomyces israelii Arthrobacter atrocyaneus Arthrobacter sulfureus Actinomyces israelii serotype II Arthrobacter aurescens Arthrobacter uratoxydans Actinomyces meyeri Arthrobacter bergerei Arthrobacter ureafaciens Actinomyces naeslundii Arthrobacter chlorophenolicus Arthrobacter variabilis Actinomyces nasicola Arthrobacter citreus Arthrobacter viscosus Actinomyces neuii Arthrobacter creatinolyticus Arthrobacter woluwensis Actinomyces odontolyticus Arthrobacter crystallopoietes -
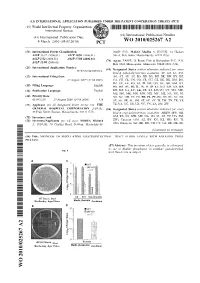
Wo 2010/025267 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 4 March 2010 (04.03.2010) WO 2010/025267 A2 (51) International Patent Classification: 02459 (US). MALO, Madhu S. [US/US]; 14 Hudson A61K 33/42 (2006.01) A61P 19/02 (2006.01) Street, Watertown, Massachusetts 02474 (US). A61P 1/12 (2006.01) A61P 37/08 (2006.01) (74) Agent: FASSE, J. Peter; Fish & Richardson P.C., P.O. A61P 31/04 (2006.01) Box 1022, Minneapolis, Minnesota 55440-1022 (US). (21) International Application Number: (81) Designated States (unless otherwise indicated, for every PCT/US2009/055216 kind of national protection available): AE, AG, AL, AM, (22) International Filing Date: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, 27 August 2009 (27.08.2009) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (25) Filing Language: English HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (26) Publication Language: English KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (30) Priority Data: NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, 61/093,129 29 August 2008 (29.08.2008) US SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (71) Applicant (for all designated States except US): THE TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

Oxygen Dependent Pyruvate Oxidase Expression and Production in Streptococcus Sanguinis
Int J Oral Sci (2011) 3: 82-89. www.ijos.org.cn ORIGINAL ARTICLE Oxygen dependent pyruvate oxidase expression and production in Streptococcus sanguinis Lan-yan Zheng1, 2*, Andreas Itzek1, Zhi-yun Chen1, Jens Kreth1, 3 1Department of Microbiology and Immunology, University of Oklahoma Health Sciences Center, Oklahoma 73104, USA; 2China Medical University, Department of Microbiology and Parasitology, Shenyang 110001, China; 3Department of Oral Biology, College of Dentistry, University of Oklahoma Health Sciences Center, Oklahoma 73104, USA The objective of this study was to characterize the oxygen dependent regulation of pyruvate oxidase (SpxB) gene expression and protein production in Streptococcus sanguinis (S. sanguinis). SpxB is responsible for the generation of growth-inhibiting amounts of hydrogen peroxide (H2O2) able to antagonize cariogenic Strepto- coccus mutans (S. mutans). Furthermore, the ecological consequence of H2O2 production was investigated in its self-inhibiting ability towards the producing strain. Expression of spxB was determined with quantitative Real-Time RT-PCR and a fluorescent expression reporter strain. Protein abundance was investigated with FLAG epitope engineered in frame on the C-terminal end of SpxB. Self inhibition was tested with an antagonism plate assay. The expression and protein abundance decreased in cells grown under anaerobic conditions. S. sanguinis was resistant against its own produced H2O2, while cariogenic S. mutans was inhibited in its growth. The results suggest that S. sanguinis produces H2O2 as antimicrobial substance to inhibit susceptible niche competing species like S. mutans during initial biofilm formation, when oxygen availability allows for spxB expression and Spx production. Keywords: Streptococcus sanguinis; pyruvate oxidase; oxygen dependent International Journal of Oral Science (2011) 3: 82-89. -

From Genotype to Phenotype: Inferring Relationships Between Microbial Traits and Genomic Components
From genotype to phenotype: inferring relationships between microbial traits and genomic components Inaugural-Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakult¨at der Heinrich-Heine-Universit¨atD¨usseldorf vorgelegt von Aaron Weimann aus Oberhausen D¨usseldorf,29.08.16 aus dem Institut f¨urInformatik der Heinrich-Heine-Universit¨atD¨usseldorf Gedruckt mit der Genehmigung der Mathemathisch-Naturwissenschaftlichen Fakult¨atder Heinrich-Heine-Universit¨atD¨usseldorf Referent: Prof. Dr. Alice C. McHardy Koreferent: Prof. Dr. Martin J. Lercher Tag der m¨undlichen Pr¨ufung: 24.02.17 Selbststandigkeitserkl¨ arung¨ Hiermit erkl¨areich, dass ich die vorliegende Dissertation eigenst¨andigund ohne fremde Hilfe angefertig habe. Arbeiten Dritter wurden entsprechend zitiert. Diese Dissertation wurde bisher in dieser oder ¨ahnlicher Form noch bei keiner anderen Institution eingereicht. Ich habe bisher keine erfolglosen Promotionsversuche un- ternommen. D¨usseldorf,den . ... ... ... (Aaron Weimann) Statement of authorship I hereby certify that this dissertation is the result of my own work. No other person's work has been used without due acknowledgement. This dissertation has not been submitted in the same or similar form to other institutions. I have not previously failed a doctoral examination procedure. Summary Bacteria live in almost any imaginable environment, from the most extreme envi- ronments (e.g. in hydrothermal vents) to the bovine and human gastrointestinal tract. By adapting to such diverse environments, they have developed a large arsenal of enzymes involved in a wide variety of biochemical reactions. While some such enzymes support our digestion or can be used for the optimization of biotechnological processes, others may be harmful { e.g. mediating the roles of bacteria in human diseases. -

A Candidate Virulence Factor in Streptococcus Sanguinis Experimental Endocarditis
Ecto-59-Nucleotidase: A Candidate Virulence Factor in Streptococcus sanguinis Experimental Endocarditis Jingyuan Fan1¤, Yongshu Zhang1, Olivia N. Chuang-Smith2, Kristi L. Frank2, Brian D. Guenther1, Marissa Kern1, Patrick M. Schlievert2, Mark C. Herzberg1,3* 1 Department of Diagnostic and Biological Sciences, School of Dentistry, University of Minnesota, Minneapolis, Minnesota, United States of America, 2 Department of Microbiology, University of Minnesota Medical School, Minneapolis, Minnesota, United States of America, 3 Mucosal and Vaccine Research Center, Minneapolis Veterans Affairs Medical Center, Minneapolis, Minnesota, United States of America Abstract Streptococcus sanguinis is the most common cause of infective endocarditis (IE). Since the molecular basis of virulence of this oral commensal bacterium remains unclear, we searched the genome of S. sanguinis for previously unidentified virulence factors. We identified a cell surface ecto-59-nucleotidase (Nt5e), as a candidate virulence factor. By colorimetric phosphate assay, we showed that S. sanguinis Nt5e can hydrolyze extracellular adenosine triphosphate to generate adenosine. Moreover, a nt5e deletion mutant showed significantly shorter lag time (P,0.05) to onset of platelet aggregation than the wild-type strain, without affecting platelet-bacterial adhesion in vitro (P = 0.98). In the absence of nt5e, S. sanguinis caused IE (4 d) in a rabbit model with significantly decreased mass of vegetations (P,0.01) and recovered bacterial loads (log10CFU, P = 0.01), suggesting that Nt5e contributes to the virulence of S. sanguinis in vivo. As a virulence factor, Nt5e may function by (i) hydrolyzing ATP, a pro-inflammatory molecule, and generating adenosine, an immunosuppressive molecule to inhibit phagocytic monocytes/macrophages associated with valvular vegetations. -

Identification of Clinically Relevant Streptococcus and Enterococcus
pathogens Article Identification of Clinically Relevant Streptococcus and Enterococcus Species Based on Biochemical Methods and 16S rRNA, sodA, tuf, rpoB, and recA Gene Sequencing Maja Kosecka-Strojek 1,* , Mariola Wolska 1, Dorota Zabicka˙ 2 , Ewa Sadowy 3 and Jacek Mi˛edzobrodzki 1 1 Department of Microbiology, Faculty of Biochemistry, Biophysics and Biotechnology, Jagiellonian University, 30-387 Krakow, Poland; [email protected] (M.W.); [email protected] (J.M.) 2 Department of Molecular Microbiology, National Medicines Institute, 00-725 Warsaw, Poland; [email protected] 3 Department of Epidemiology and Clinical Microbiology, National Medicines Institute, 00-725 Warsaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-12-664-6365 Received: 13 October 2020; Accepted: 9 November 2020; Published: 11 November 2020 Abstract: Streptococci and enterococci are significant opportunistic pathogens in epidemiology and infectious medicine. High genetic and taxonomic similarities and several reclassifications within genera are the most challenging in species identification. The aim of this study was to identify Streptococcus and Enterococcus species using genetic and phenotypic methods and to determine the most discriminatory identification method. Thirty strains recovered from clinical samples representing 15 streptococcal species, five enterococcal species, and four nonstreptococcal species were subjected to bacterial identification by the Vitek® 2 system and Sanger-based sequencing methods targeting the 16S rRNA, sodA, tuf, rpoB, and recA genes. Phenotypic methods allowed the identification of 10 streptococcal strains, five enterococcal strains, and four nonstreptococcal strains (Leuconostoc, Granulicatella, and Globicatella genera). The combination of sequencing methods allowed the identification of 21 streptococcal strains, five enterococcal strains, and four nonstreptococcal strains. -

Incidence of Bacteriocins Produced by Food-Related Lactic Acid Bacteria Active Towards Oral Pathogens
Int. J. Mol. Sci. 2013, 14, 4640-4654; doi:10.3390/ijms14034640 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Incidence of Bacteriocins Produced by Food-Related Lactic Acid Bacteria Active towards Oral Pathogens Georgia Zoumpopoulou 1, Eudoxie Pepelassi 2, William Papaioannou 3, Marina Georgalaki 1, Petros A. Maragkoudakis 1,†, Petros A. Tarantilis 4, Moschos Polissiou 4, Effie Tsakalidou 1 and Konstantinos Papadimitriou 1,* 1 Laboratory of Dairy Research, Department of Food Science and Technology, Agricultural University of Athens, Iera Odos 75, Athens 11855, Greece; E-Mails: [email protected] (G.Z.); [email protected] (M.G.); [email protected] (P.A.M.); [email protected] (E.T.) 2 Department of Periodontology, School of Dentistry, National and Kapodistrian University of Athens, 2 Thivon Str., Athens 11527, Greece; E-Mail: [email protected] 3 Department of Preventive and Community Dentistry, School of Dentistry, National and Kapodistrian University of Athens, 2 Thivon Str., Athens 11527, Greece; E-Mail: [email protected] 4 Laboratory of Chemistry, Department of Science, Agricultural University of Athens, Iera Odos 75, Athens 11855, Greece; E-Mails: [email protected] (P.A.T.); [email protected] (M.P.) † Present address: European Commission, Joint Research Centre, via E. Fermi 2749, Ispra 21027, Varese, Italy; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +30-210-529-4661; Fax: +30-210-529-4672. Received: 8 October 2012; in revised form: 1 February 2013 / Accepted: 18 February 2013 / Published: 26 February 2013 Abstract: In the present study we investigated the incidence of bacteriocins produced by 236 lactic acid bacteria (LAB) food isolates against pathogenic or opportunistic pathogenic oral bacteria. -

Two-Component System Vicrk Regulates Functions Associated with Establishment of Streptococcus Sanguinis in Biofilms
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositorio da Producao Cientifica e Intelectual da Unicamp Two-Component System VicRK Regulates Functions Associated with Establishment of Streptococcus sanguinis in Biofilms Julianna J. Moraes, Rafael N. Stipp, Erika N. Harth-Chu, Tarsila M. Camargo, José F. Höfling, Renata O. Mattos-Graner Department of Oral Diagnosis, Piracicaba Dental School, University of Campinas, Piracicaba, Sao Paulo, Brazil Streptococcus sanguinis is a commensal pioneer colonizer of teeth and an opportunistic pathogen of infectious endocarditis. The establishment of S. sanguinis in host sites likely requires dynamic fitting of the cell wall in response to local stimuli. In this study, we investigated the two-component system (TCS) VicRK in S. sanguinis (VicRKSs), which regulates genes of cell wall bio- genesis, biofilm formation, and virulence in opportunistic pathogens. A vicK knockout mutant obtained from strain SK36 (SKvic) showed slight reductions in aerobic growth and resistance to oxidative stress but an impaired ability to form biofilms, a phenotype restored in the complemented mutant. The biofilm-defective phenotype was associated with reduced amounts of ex- tracellular DNA during aerobic growth, with reduced production of H2O2, a metabolic product associated with DNA release, and with inhibitory capacity of S. sanguinis competitor species. No changes in autolysis or cell surface hydrophobicity were detected in SKvic. Reverse transcription-quantitative PCR (RT-qPCR), electrophoretic mobility shift assays (EMSA), and promoter se- quence analyses revealed that VicR directly regulates genes encoding murein hydrolases (SSA_0094, cwdP, and gbpB) and spxB, which encodes pyruvate oxidase for H2O2 production. -

Ldentif Ication of Clinically Relevant Viridans Streptococci by Analysis of Transfer DNA Intergenic Spacer Length Polymorphism
international Journal of Systematic Bacteriology (1 999), 49, 1 59 1-1 598 Printed in Great Britain ldentif ication of clinically relevant viridans streptococci by analysis of transfer DNA intergenic spacer length polymorphism Y. De Gheldre,' P. Vandamme,213H. Goossens3and M. J. Struelens' Author for correspondence: Yves De Gheldre. Tel: + 32 2 555 4517. Fax: + 32 2 555 6459. e-mail : [email protected] 1 Department of The utility of PCR analysis of transfer DNA intergenic spacer length Microbiology, HBpital polymorphism @DNA-ILP)for the identification to the species level of clinically Erasme, Universite Libre de Bruxelles, 808 Route de relevant viridans streptococci was evaluated with a collection of reference Lennik, 1070 Brussels, strains of 15 species of the salivarius, anginosus, mitis and mutans rRNA Belgium homology groups. PCR products generated by using fluorescent, outwardly 2 Laboratory of directed, consensus tDNA primers were analysed by electrophoresis on Microbiology and denaturating polyacrylamide gels and by laser fluorescence scanning. Eleven BCCM/LMG Culture Collection, University of species showed specific and distinct tDNA patterns : Streptococcus cristatus, Ghent, Belgium Streptococcus gordonii, Streptococcus oralis, Streptococcus mitis, 3 Laboratory of Medical Streptococcus pneumoniae, Streptococcus sanguinis, Streptococcus Microbiology, University parasanguinis, Streptococcus anginosus, Streptococcus mutans, Streptococcus Hospital Antwerp, criceti and Streptococcus ratti. Indistinguishable patterns were obtained Antwerp, Belgium among two groups of species : Streptococcus vestibularis and Streptococcus salivarius on the one hand and Streptococcus constellatus and Streptococcus intermedius on the other. 5. mitis strains produced heterogeneous patterns that could be separated into three groups: a group containing S. mitis biovar 1 and two S, mitis biovar 2 groups, one of which clustered with S.