Sub-District Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Constituency-Wise Information on Inclusion and Deletions in Current Electoral Over Previous Roll
ELECTION COMMISSION OF INDIA Format 4B Format 4B (With CEO) Constituency-wise Information on Inclusion and Deletions in Current Electoral Over Previous Roll Name of State: BIHAR Net % Total claims lodged in Total Objections Lodged in Suo-moto Deletion Electors as per proposed Final change Change Electors as per Draft Roll w.r.t. Total Deletions subsequent Assembly Constituency Form 6 after draft Total Claims admitted Form 7 after draft publication Total Objections admitted subsenquent to last Number of Deletions Due to Roll w.r.t. 01.01.2021 as the over over 01.01.2021 as the qualifying date to last publication of roll publication of roll of roll pulication of roll qualifying date previous previuos Final roll Final roll Third Third Third Third Third Third Third Third No Name Male Female Male Female Male Female Male Female Male Female Male Female Male Female Expired Shifted Repeated Male Female (+/-) (+/-) Gender Gender Gender Gender Gender Gender Gender Gender 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 1 Valmiki Nagar 178264 153489 34 6317 5476 3 85 60 0 0 0 0 85 60 0 85 60 0 184499 158902 37 11651 3.39 2 Ramnagar (SC) 155977 139899 10 3372 2676 0 46 28 0 0 0 0 46 28 0 0 1 62 159305 142545 10 5974 1.98 3 Narkatiaganj 141813 123638 16 3340 2798 1 345 296 0 0 0 0 345 296 0 468 80 70 144815 126133 17 5498 2.03 4 Bagaha 162404 142895 15 4055 3721 1 142 155 0 0 0 0 142 155 0 147 25 121 166316 146462 16 7480 2.39 5 Lauriya 137451 118586 11 1999 1647 0 87 68 0 0 0 0 87 68 0 96 28 29 139363 120165 11 3491 -

Revised Centre List of TDC Part
Revised Centre List of T.D.C. Part - IInd & IIIrd Practical Examination - 2016 Date of Examination: From 22.04.2017 onwards Sl. Name of Centre Subjects Name of Colleges No. 1. L.S. College, PHY, CHE, BOT, ZOO, 1. L.S. College, Muzaffarpur Muzaffarpur ELECTRONICS and 2. R.B.B.M. College, Muzaffarpur only Sc. PSY. 3. J.B.S.D. College, Bakuchi only Sc. & PSY 4. All Const. & Affiliated Colleges under the jurisdiction of BRABU, Muzaffarpur only Elect. 2. R.D.S. College, PHY, CHE, BOT, ZOO, 1. R.D.S. College, Muzaffarpur Muzaffarpur PSY and, GEO. 2. R.C. College, Sakra only GEO 3. R.S. College, Muz only GEO 4. L.N.T. College, Muz.- SC, PSY & GEO 5. S.R.P.S. College, Jaitpur – PSY & SC 6. Remaining all Coll. of Muz., Sitamarhi District only GEO. 3 M.D.D.M. College, PHY, CHE, BOT, ZOO, 1. M.D.D.M. College, Muz. Muzaffarpur PSY, HSC, GEO & 2. M.S.K.B. College, Muz. Only Sc. MUSIC. 3. L.N.T. College, Muz. Only HSC. 4. All Constituent & Affiliated Colleges of Muzaffarpur, Sitamarhi, Vaishali Distt. only Music, 4 R.B.B.M., College, PSY, HSC 1. R.B.B.M. College, Muz. Muzaffarpur 2. J. College, Motipur, only HSC. 3. C.N. College Sahebganj only HSC 5. M.S.K.B. College, PSY, HSC 1. M.S.K.B. College, Muzaffarpur Muzaffarpur 6. Niteshwar College, PHY, CHE, BOT, ZOO, 1. Niteshwar College, Muzaffarpur Muzaffarpur PSY, HSC, GEO 2. Dr. R.M.L.S. College, Muz only SC. -

District Health Society, Sheohar Sadar Hospital Campus, Sheohar (Bihar) Pin – 843329, Phone : 06222 - 259292 0
District Health Action Plan 2012-2013 District Health Society, Sheohar Sadar Hospital Campus, Sheohar (Bihar) Pin – 843329, Phone : 06222 - 259292 0 Table of contents Foreword About the Profile CHAPTER 1- INTRODUCTION - Page 4 to 7 1.1 Background 1.2 Objectives of the process 1.3 Process of Plan Development 1.3.1 Preliminary Phase 1.3.2 Main Phase - Horizontal Integration of Vertical Programmes 1.3.3 Preparation of DHAP CHAPTER 2- DISTRICT PROFILE - Page 8 to 31 2.1 History 2.2 Geographic Location 2.3 Demographics 2.4 Administrative Units & Towns 2.5 Population at a Glance 2.6 Comparative Population 2.7 District Profile 2.8 Health Facilities in the District 2.9 Human Resource & Infrastructure 2.10 Equipments 2.11 Rogi Kalyan Samiti 2.12 Support System 2.13 Health Services 2.14 Community Participation 2.15 Training Activities 2.16 BCC Campaigns 2.17 District and Block Level Management 2.18 Health Care Institutions in the District CHAPTER 3- SITUATION ANALYSIS- Page 32 to 40 3.1 Gaps in infrastructure 3.2 Health Sub Centre (HSC) 3.3 Additional PHC (APHC) 3.4 Primary Health Centre 3.5 Sadar Hospital CHAPTER 4 – Setting Objectives and suggested plan of Action – Page -41 to 82 4.1 Introduction 4.2 Targeted objective and suggested strategies 4.3 Meternal Health 4.4 Child Health 4.5 Family Planning 4.6 Institutional strengthening Part- A Programme wise Budget Part- B Programme wise Budget Part- C Programme wise Budget Vitamin A Mamta IDD IDSP VBDCP (Kala-Azar) 1 Foreword Recognizing the importance of Health in the process of economic and social development and improving the quality of life of our citizens, the Government of India has resolved to launch the National Rural Health Mission to carry out necessary architectural correction in the basic health care delivery system . -

Access-Of-Muslims-And-Other-Religious-Minorities-To-Rights-And-Freedoms-Bihar.Pdf
Access of Muslims and Other Religious Minorities to Rights and Freedoms – Bihar This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Provided they acknowledge the source, users of this content are allowed to remix, tweak, build upon and share for noncommercial purposes under the same original license terms. Some rights reserved Published by: Misaal - Centre for Equity Studies 24, Khazan Singh Building Adhchini, Aurobindo Marg New Delhi - 110 017, India Tel: +91 (0)11-26535961 / 62 Email: [email protected] Web : www.misaal.ngo Facebook: https://www.facebook.com/misaalfellowship Credits: This report has been produced with the assistance of the Swedish International Development Cooperation Agency. Minority Rights Group International provided technical help. The contents of this report are the sole responsibility of Misaal-CES, and can in no way be taken to reflect the views of the Swedish International Development Cooperation Agency or of Minority Rights Group International. December 2016 Access of Muslims and Other Religious Minorities to Rights and Freedoms Bihar December 2016 i Executive Summary 1. This study aims to examine the access of religious minorities in the state of Bihar to minority rights - including to freedom of religion, life and security, and social, economic and cultural rights. The focus of the study is Muslims - by far the largest religious minority in Bihar, and India as a whole. We try to measure access to rights by mapping poor Muslims’ conditions as well as by examining the quality of state provisioning for them. This examination is based on (i) primary data on micro evidence on the condition of poor Muslims, collected from 5 sample sites of Muslim habitations in UP (Patna, Vaishali, Sitamarhi, Darbhanga and Madhubani districts) using household surveys (sample of 100 poor Muslim households at each site) and interviews and focus group discussions, as methods. -

Sheohar District, Bihar State
भूजल सूचना पुस्तिका शिवहर स्जला, बिहार Ground Water Information Booklet Sheohar District, Bihar State 85° 15' INDEX MAP N SHEOHAR DISTRICT, BIHAR Baghmati R. 0 1 2 3 4 5 Km PURNAHIA Scale Rajwa Nadi PIPRAHI Baghmati R. Kola Nadi SHEOHAR 26° 26° 30' Baisundar Nala 30' DUMRI KATSARI Baghmati R. Baghmati LEGEND DISTRICT BOUNDARY TARIYANI BLOCK BOUNDARY ROAD RIVER DISTRICT HEADQUARTER BLOCK HEADQUARTER 85° 15' के न्द्रीय भशू िजल िो셍 ड Central Ground water Board Ministry of Water Resources जल संसाधन िंत्रालय (Govt. of India) (भारि सरकार) Mid-Eastern Region िध्य-पूवी क्षेत्र Patna पटना शसिंिर 2013 September 2013 1 Prepared By - Dr. Rakesh Singh, Scientist – ‘B’ 2 SHEOHAR (BIHAR) S. No CONTENTS PAGE NO. 1.0 Introduction 6 - 9 1.1 Administrative details 1.2 Basin/sub-basin, Drainage 1.3 Irrigation Practices 1.4 Studies/Activities by CGWB 2.0 Climate and Rainfall 9 - 10 3.0 Geomorphology and Soils 10 - 11 4.0 Ground Water Scenario 11 – 16 4.1 Hydrogeology 4.2 Ground Water Resources 4.3 Ground Water Quality 4.4 Status of Ground Water Development 5.0 Ground Water Management Strategy 16 5.1 Ground Water Development 5.2 Water Conservation and Artificial Recharge 6.0 Ground Water related issue and problems 16 – 16 7.0 Mass Awareness and Training Activity 16 – 16 8.0 Area Notified by CGWB/SGWA 16 – 16 9.0 Recommendations 17 - 17 FIGURES 1.0 Index map of Sheohar district 2.0 Month wise rainfall plot for the district 3.0 Hydrogeological map of Sheohar district 4.0 Depth to Water Level map (May 2011) 5.0 Depth to Water Level map (November 2011) 6.0 Block wise Dynamic Ground Water (GW) Resource of Sheohar district TABLES 1.0 Boundary details of Sheohar district 2.0 Administrative details of Sheohar district 3.0 Land use pattern in Sheohar district 4.0 Geological succession of the Quaternary deposit of Sheohar district 5.0 Block wise Dynamic Ground Water Resource of Sheohar District (2008-09) 6.0 Chemical quality of water found in Sheohar district, Bihar 3 SHEOHAR DISTRICT AT A GLANCE 1 GENERAL INFORMATION Geographical Area (Sq. -
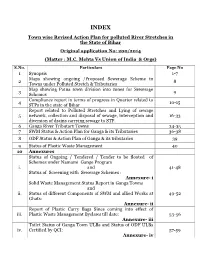
Town Wise Revised Action Plan for Polluted River Stretches in the State of Bihar Original Application No: 200/2014 (Matter : M.C
INDEX Town wise Revised Action Plan for polluted River Stretches in the State of Bihar Original application No: 200/2014 (Matter : M.C. Mehta Vs Union of India & Orgs) S.No. Particulars Page No 1 Synopsis 1-7 Maps showing ongoing /Proposed Sewerage Scheme in 2 8 Towns under Polluted Stretch & Tributaries Map showing Patna town division into zones for Sewerage 3 9 Schemes Compliance report in terms of progress in Quarter related to 4 10-15 STPs in the state of Bihar Report related to Polluted Stretches and Lying of sewage 5 network, collection and disposal of sewage, interception and 16-33 diversion of drains carrying sewage to STP. 6 Ganga River Tributary Towns 34-35 7 SWM Status & Action Plan for Ganga & its Tributaries 36-38 8 ODF Status & Action Plan of Ganga & its tributaries 39 9 Status of Plastic Waste Management 40 10 Annexures Status of Ongoing / Tendered / Tender to be floated of Schemes under Namami Gange Program i. and 41-48 Status of Screening with Sewerage Schemes : Annexure- i Solid Waste Management Status Report in Ganga Towns and ii. Status of different Components of SWM and allied Works at 49-52 Ghats: Annexure- ii Report of Plastic Carry Bags Since coming into effect of iii. Plastic Waste Management Byelaws till date: 53-56 Annexure- iii Toilet Status of Ganga Town ULBs and Status of ODF ULBs iv. Certified by QCI: 57-59 Annexure- iv 60-68 and 69 11 Status on Utilization of treated sewage (Column- 1) 12 Flood Plain regulation 69 (Column-2) 13 E Flow in river Ganga & tributaries 70 (Column-4) 14 Assessment of E Flow 70 (Column-5) 70 (Column- 3) 15 Adopting good irrigation practices to Conserve water and 71-76 16 Details of Inundated area along Ganga river with Maps 77-90 17 Rain water harvesting system in river Ganga & tributaries 91-96 18 Letter related to regulation of Ground water 97 Compliance report to the prohibit dumping of bio-medical 19 98-99 waste Securing compliance to ensuring that water quality at every 20 100 (Column- 5) point meets the standards. -

Master Plan for Patna - 2031
IMPROVING DRAFT MASTER PLAN FOR PATNA - 2031 FINAL REPORT Prepared for, Department of Urban Development & Housing, Govt. of Bihar Prepared by, CEPT, Ahmadabad FINAL REPORT IMPROVING DRAFT MASTER PLAN FOR PATNA-2031 FINAL REPORT IMPROVING DRAFT MASTER PLAN FOR PATNA - 2031 Client: Urban Development & Housing Department Patna, Bihar i Prepared by: Center for Environmental Planning and Technology (CEPT) University Kasturbhai Lalbhai Campus, University Road, Navrangpura, Ahmedabad – 380 009 Gujarat State Tel: +91 79 2630 2470 / 2740 l Fax: +91 79 2630 2075 www.cept.ac.in I www.spcept.ac.in CEPT UNIVERSITY I AHMEDABAD i FINAL REPORT IMPROVING DRAFT MASTER PLAN FOR PATNA-2031 TABLE OF CONTENTS TABLE OF CONTENTS i LIST OF TABLES v LIST OF FIGURES vii LIST OF MAPS viii LIST of ANNEXURE ix 1 INTRODUCTION 10 1.1 Introduction 11 1.2 Planning Significance of Patna as a City 12 1.3 Economic Profile 14 1.4 Existing Land Use – Patna Municipal Corporation Area 14 1.5 Previous Planning Initiatives 16 1.5.1 Master Plan (1961-81) 16 1.5.2 Plan Update (1981-2001) 17 1.5.3 Master Plan 2001-21 18 1.6 Need for the Revision of the Master Plan 19 1.7 Methodology 20 1.7.1 Stage 1: Project initiation 20 1.7.2 Stage 02 and 03: Analysis of existing situation & Future projections and Concept Plan 21 1.7.3 Stage 04: Updated Base Map and Existing Land Use Map 21 1.7.4 Stage 5: Pre-final Master Plan and DCR 24 2 DELINEATION OF PATNA PLANNING AREA 25 i 2.1 Extent of Patna Planning Area (Project Area) 26 2.2 Delineation of Patna Planning Area (Project Area) 27 2.3 Delineated -

Eci Format (1-8)
FORMAT 7 Information on Service Voters AC No. and Name Service Voters as on De-Novo date Enrolled Service Voter According to Service Voter Portal (28.01.2019) Armed Govt. Of which Total force of Total Names Names Names Total SVs Armed Person CSVs No. of Service States Service Form 2 Form 2A Form 3 added in added added added No. Name Forces of employed (Voter CSVs Voters posted Voters Recd Recd Recd roll thru thru thru (Col. the Union outside with added outside Form 2 Form 2A Form 3 11+12+13) country proxy) state 1 2 3 4 5 6 7 8 9 10 11 1213 14 1516 1 Valmiki Nagar 0 0 0 0 0253 0 0 - - - 232 0 232 2 Ramnagar (SC) 0 0 0 0 0282 0 2 - - - 261 0 261 3 Narkatiaganj 0 0 0 0 0142 0 0 - - - 129 0 129 4 Bagaha 0 0 0 0 0281 0 1 - - - 259 0 259 5 Lauriya 0 0 0 0 0191 0 0 - - - 186 0 186 6 Nautan 0 0 0 0 0260 0 0 - - - 251 0 251 7 Chanpatia 0 0 0 0 0607 0 0 - - - 576 0 576 8 Bettiah 0 0 0 0 0467 0 2 - - - 459 0 459 9 Sikta 0 0 0 0 0197 0 0 - - - 189 0 189 West Champaran District Total 0 0 0 0 0 2680 0 5 --- 2542 0 2542 10 Raxaul 0 0 0 0 0309 0 0 - - - 290 0 290 11 Sugauli 0 0 0 0 0608 0 0 - - - 586 0 586 12 Narkatia 0 0 0 0 0198 0 0 - - - 188 0 188 13 Harsidhi (SC) 0 0 0 0 0321 0 4 - - - 305 0 305 14 Govindganj 0 0 0 0 0476 0 1 - - - 453 0 453 15Kesaria 0 0 0 0 0286 0 0 - - - 261 0 261 16Kalyanpur 0 0 0 0 0286 0 0 - - - 270 0 270 17Pipra 0 0 0 0 0279 0 0 - - - 259 0 259 18Madhuban 0 0 0 0 0173 0 0 - - - 161 0 161 19Motihari 0 0 0 0 0371 0 1 - - - 313 0 313 20 Chiraia 0 0 0 0 0235 0 2 - - - 221 0 221 21 Dhaka 0 0 0 0 0250 0 0 - - - 221 0 221 East Champaran District Total 0 0 0 0 0 3792 0 8 --- 3528 0 3528 22Sheohar 0 0 0 0 0172 0 2 - - - 153 0 153 Sheohar District Total 0 0 0 0 0 172 0 2 --- 153 0 153 AC No. -
Vaishali Introduction
DISTRICT PROFILE VAISHALI INTRODUCTION Vaishali district is one of the thirty-eight districts of the state of Bihar. It formed in 1972, separated from Muzaffarpur district. The district is surrounded by Muzaffarpur district in the North, Samastipur district in the East and Ganga River in South and Gandak River in West. The Vaishali district is a part of Tirhut division and the district headquarters are at Hajipur town. Hajipur is separated from the State’s biggest city Patna by a River Ganga. It is the second fastest growing city in the state. HISTORICAL BACKGROUND Vaishali got its name from King Vishal, a predecessor to Lord Ram. Vaishali finds reference in the Indian epics Ramayana. Vaishali was the capital of the Lichchavi State, considered as the First Republic in the World. It is said that the Lord Buddha, delivered his last semon and announced his Mahaparinirvana during his visit to Vaishali. 100 years after the Lord Buddha attained Mahaparinirvana, second Buddhist Council was held at Vaishali. Jain Tirthankar Lord Mahavir was said to be born at Vaishali to King Siddhartha and Queen Trishala. Amrapali the famous courtesan, has invited Lord Buddha to her house and Lord has visited her place. With Lord Buddha’s visit, Amrapali was purged with all impurities, she gifted her mango grove to the Sangh and joined Buddhism. Ananda, the favorite disciple of Buddha, attained Nirvana in the midst of Ganga outside Vaishali. ADMINISTRATIVE Hajipur City is the district headquarters. Vaishali district spread across 3 talukas: Mahnar, Hajipur, Mahua Vaishali district has been divided into 16 Municipal Blocks: o Mahnar o Hajipur o Chehrakala o Vaishali o Mahua o Premraj o Bidupur o Jandaha o Patedhi-Belshar o Goraul o Patepur o Desri o Raghopur o Sahadi buzurg o Lalganj o Bahgwanpur Total Number of Panchayats in Vaishali district 291. -

District Health Society Vaishali
District Health Plan 2009-2010 District Health Society Vaishali Table of contents Foreword About the Profile CHAPTER 1- INTRODUCTION 1.1 Background 1.2 Objectives of the process 1.3 Process of Plan Development 1.3.1 Preliminary Phase 1.3.2 Main Phase - Horizontal Integration of Vertical Programmes 1.3.3 Preparation of DHAP CHAPTER 2- DISTRICT PROFILE History Geographic Location Govt administrative setup Administrative units and towns. District Health Administrative setup Vaishali at a Glance Comparative Population Data 2.1 Socio economic Profile 2.2 Health Profile Indicators of Reproductive health and Child health 2.2.1 Health Status and Burden of diseases 2.2.2 Public Health Care delivery system 2.3 Map showing specialist doctors position 2.4 Map showing PHC and APHC locations 2.5 DLHS 3 data CHAPTER 3- SITUATION ANALYSIS 3.1 Gaps in infrastructure 3.1.1 HSC Infrastructure 3.1.2 Services of HSC 3.1.3 HSC Human Resource 3.2 APHC 3.3 PHC 3.4 District Hospital CHAPTER 4-Setting Objectives and suggested Plan of Action 4.1 Introduction 4.2 Targeted objectives and suggested Strategies 4.3 Maternal Health 4.4 Child Health 4.5 Family Planning 4.6 Kala-azar program 4.7 Blindness Control Program 4.8 Leprosy Eradication Program 4.9 Tuberculosis control Program 4.10 Filaria Control Prgram 4.11 Institution Strengthening 4.12 Program wise Budget 4.13 HIV/AIDS Foreword Recognizing the importance of Health in the process of economic and social development and improving the quality of life of our citizens, the Government of India has resolved to launch the National Rural Health Mission to carry out necessary architectural correction in the basic health care delivery system. -

ANSWERED ON:01.12.2014 INCLUSION of CITES in WORLD HERITAGE Singh Shri Rama Kishore
GOVERNMENT OF INDIA CULTURE LOK SABHA UNSTARRED QUESTION NO:1327 ANSWERED ON:01.12.2014 INCLUSION OF CITES IN WORLD HERITAGE Singh Shri Rama Kishore Will the Minister of CULTURE be pleased to state: (a) whether the Government proposes to take steps for inclusion of various Indian cities in the UNESCO's World Heritage list; (b) if so, the details thereof and the present status of the cities along with the criteria adopted by the UNESCO to include ancient sites/ tourist places in World Heritage List; (c) whether the Government has identified or received any proposal from various State Governments to include places including Delhi and Vaishali in Bihar in the World Heritage list; (d) if so, the details thereof and the status of the proposals along with the time by which these places are likely to be considered by the World Heritage Committee, UNESCO for inclusion in the list; (e) whether the Government has conducted any survey to study the ancient historical importance of cities including Vaishali in Bihar; and (f) if so, the details thereof? Answer MINISTER OF STATE, CULTURE AND TOURISM (INDEPENDENT CHARGE) AND MINISTER OF STATE, CIVIL AVIATION (DR.MAHESH SHARMA) (a) Yes, Madam. (b) The nomination dossiers of Delhi Imperial Capital Cities and The Victorian & Art Deco Ensemble of Mumbai have been submitted to World Heritage Centre in January, 2014. The International Council on Monuments and Sites (ICOMOS) ICOMOS mission visited in October, 2014 to evaluate the property of Delhi Imperial Capital Cities. The decision to declare Delhi as World Heritage City would be taken in the World Heritage Committee meeting 2015. -

Social Changes Among the Scheduled Caste Population of the Vaishali District: a Geographical Study
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 22, Issue 7, Ver.13 (July.2017) PP 34-41 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Social Changes among the Scheduled Caste Population of the Vaishali District: A Geographical Study. * Sanjay Kumar Corresponding Author: Sanjay Kumar *UGC (NET) Qualified Research Scholar, College of Commerce, Arts & Science (Magadh University), Patna-20 Abstract: Change in social conditions concerns; transformation of culture, behaviour, social institutions and social structure of a society over time . It has taken place in most areas but as far as the less developed areas are concerned these have recorded phenomenal changes during the recent years due to improved educational facilities, economic conditions, mass- media communication, efforts of the social reformers, government policies, etc. So also the less developed areas of the State of Bihar have experienced significant social changes. The district of Vaishali, one of the country's 250 most backward districts, as by the ministry of Panchayati Raj identified in 2006, has also recorded considerable changes in the attitudinal, behavioural and structural features of the Scheduled Castes. The present paper aims to highlight the changes which have taken place among different Scheduled Castes of the selected villages of the Vaishali district. The paper highlights the changes in the social conditions of the migrant and non-migrant Scheduled Caste people with special reference to some of the social features like family structure, housing conditions, educational development, religious activities, dress pattern, changes in food habit & socialization pattern, etc. Keywords: Social change, Migration. Social change: Social change is an alteration in the Cultural, Structural, Population or Ecological characteristics of a social system.