Sitamarhi District Health Society, Sitamarhi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rampur Parori
Rampur Parori Rampur Parori Weather. Bizi şurada takip edin: Oturum aç. Hindistan Hava Durumu. Rampur Parori, Hindistan. 18°C. Haritalar. Uydu. Hava Tahmin Haritaları. Rampur Parori, Hindistan. Rampur Paroriwikipedia. Rampur Parori is a native village in Dumra, Sitamarhi. Dumra. 50% (1/1). Dumra. Dumra is a town and a notified area in Sitamarhi district in Bihar, India. Dumra is the headquarter of Sitamarhi district. It has approximately 16 wards. From Meta, a Wikimedia project coordination wiki. Jump to navigation Jump to search. Adarsh bhardwaj s/o Anand kishor Singh from Rampur parori west Sitamarhi Bihar. Retrieved from "https://meta.wikimedia.org/w/index.php?title=User:Kumar_Adarsh_Bhardwaj&oldid=17983883". Navigation menu. Personal tools. English. Not logged in. Talk. Rampur Parori Road , Dumra , Sitamarhi. Fun, Masti & celebration in our hostel campus at the eve of Teacher's day. Teacher's day celebration in our school campus. Rampur Parori Road, Dumra Sitamarhi 843302. Opening Hours. Monday. Company: PAPPU PRAVIN. Address: VILL- RAMPUR PARORI EAST, POST- BANCHAURI, VIA- DUMARA,DIST- SITAMARHI, BIHAR,843302 SITAMARHI Bihar 843302 IN Phone: +91.8002685928 Email: [email protected]. Ancestral crown of Royal families of Nawabs of Rampur being auctioned in Britain. Watch complete news story of India Ki Baat for getting detailed updates! Rampur. rampur wedding video. rampur nawab video. rampur parori. Alattar visits India again in July 2014, but this time to Rampur UP ! the city where India's best parkour athletes came from. Red Bull India reunited Mohammad Rampur Bushahr Bus Stand (ISBT)Apna Himachal. 2 oy oldin. Rampur Bushahr Bus Stand (ISBT). -

Ground Water Year Book, Bihar (2015 - 2016)
का셍ााल셍 उप셍ोग हेतू For Official Use GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES CENTRAL GROUND WATER BOARD जल ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पूर्वी क्षेत्र, पटना सितंबर 2016 MID-EASTERN REGION, PATNA September 2016 ` GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES जल CENTRAL GROUND WATER BOARD ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पर्वू ी क्षेत्र, पटना MID-EASTERN REGION, PATNA सितंबर 2016 September 2016 GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) CONTENTS CONTENTS Page No. List of Tables i List of Figures ii List of Annexures ii List of Contributors iii Abstract iv 1. INTRODUCTION.............................................................................................................1 2. HYDROGEOLOGY..........................................................................................................1 3. GROUND WATER SCENARIO......................................................................................4 3.1 DEPTH TO WATER LEVEL........................................................................................8 3.1.1 MAY 2015.....................................................................................................................8 3.1.2 AUGUST 2015..............................................................................................................10 3.1.3 NOVEMBER 2015........................................................................................................12 3.1.4 JANUARY 2016...........................................................................................................14 -
Annual Report 2012-13
Government of India Ministry of Water Resources Ganga Flood Control Commission ANNUAL REPORT 2012-13 Patna Table of Contents From Chairman’s Desk (ii) Highlights of the year 2012-13 (iii) 1. Introduction 1 2. Comprehensive Plans for Flood Management 10 3. Assessment of Adequacy of Waterways Under Road and Rail Bridges 12 4. Flood Management Programme 13 5. Appraisal of Flood Management Schemes 15 6. Monitoring of Ongoing Flood Management Schemes 22 7. River Management Activities and Works related to Border Areas 26 8. Cooperation with Neighbouring Countries 33 9. Promotion of use of Hindi 37 10. Participation in Trainings, Workshops and Seminars 39 11. Representation of Ganga Flood Control Commission in Various Committees 40 i From Chairman’s Desk The Ganga basin which covers the States of Bihar, Jharkhand, Uttar Pradesh, Uttarakhand, West Bengal, Haryana, Rajasthan, Madhya Pradesh, Chhattisgarh, Himachal Pradesh, and Delhi occurrence of floods in one part or the other is an annual feature during the monsoon period. Since the Ganga is an inter-state river, it is necessary to prepare integrated plans to tackle the flood and related problems of the basin and to ensure their implementation in a co-ordinated manner. Ganga Flood Control Commission was created in 1972 as a subordinate office of Ministry of Water Resources. Since its inception, GFCC has played a vital role in assisting the States to manage the floods in the Ganga basin. As a part of its mandate it has prepared comprehensive plans of all the 23 river systems of the Ganga basin and sent the same to the State Governments for taking follow up action on the suggestions made in these plans. -

DISTRICT : Champaran-W
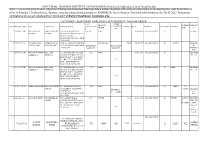
District District District District District Sl. No. Name of Husband's/Father,s AddressDate of Catego Full Marks Percent Choice-1 Choice-2 Choice-3 Choice-4 Choice-5 Candidate Name Birth ry Marks Obtained age (With Rank) (With Rank) (With Rank) (With Rank) (With Rank) DISTRICT : Champaran-W 1 PUSHPASRI NARENDRA w/o- narendra kumar 06-Feb-72 BC 900 675 75 Nawada (21) Saharsa (6) Champaran-W Patna (35) Purnia (6) KUMAR vill- jagatpur (1) post- harnaut dist- nalanda pin code- 803110 2 RENU KUMARISRI SURENDRA c/o sri surendra prasad 05-Feb-69 BC 900 672 74.67 Nalanda (32) Kaimur (3) Jahanabad (25) Gaya (24) Champaran-W (2) PRASAD SINGH singh, village+post khaddi lodipur, via- akanger sarai, district- nalanda, bihar pin 801301 3 KUMARI APARNA ASHOK KUMAR vill- bhojit pur, post- 16-Apr-83 BC 700 511 73 Champaran-E (7) Champaran-W Madhubani (2) Darbhanga (13) Muzaffarpur (23) PRIYA ekangar sarai, dist- (3) nalanda. 4RINA KUMARISRI KUMAR MAHTO d/o sri kumar mahto, 08-Dec-83 SC 500 365 73 Champaran-E (6) Champaran-W Sitamarahi (8) Madhubani (4) Patna (69) village- sakhuanwan, (4) post- gounoli, p.s. walmiki nagar, district- pachim champaran, bihar pin 845107 5RINA KUMARIMANOJ KUMAR vill- muzaffarpur, post- 28-Oct-88 BC 700 508 72.57 Champaran-E (8) Champaran-W Madhubani (5) Darbhanga (16) Samastipur (29) kathoule, disst- nalanda. (5) 6 SUCHITRA VIKASH PRASAD w/o- vikash prasad, 08-Feb-83 BC 700 507 72.43 Champaran-W Champaran-E (9) Madhubani (8) Darbhanga (18) Samastipur (32) KUMARI vill+post- ajnaura, (6) nalanda 7KUMARI SRI AMRESH musahari nagin -

District Health Society, Sheohar Sadar Hospital Campus, Sheohar (Bihar) Pin – 843329, Phone : 06222 - 259292 0
District Health Action Plan 2012-2013 District Health Society, Sheohar Sadar Hospital Campus, Sheohar (Bihar) Pin – 843329, Phone : 06222 - 259292 0 Table of contents Foreword About the Profile CHAPTER 1- INTRODUCTION - Page 4 to 7 1.1 Background 1.2 Objectives of the process 1.3 Process of Plan Development 1.3.1 Preliminary Phase 1.3.2 Main Phase - Horizontal Integration of Vertical Programmes 1.3.3 Preparation of DHAP CHAPTER 2- DISTRICT PROFILE - Page 8 to 31 2.1 History 2.2 Geographic Location 2.3 Demographics 2.4 Administrative Units & Towns 2.5 Population at a Glance 2.6 Comparative Population 2.7 District Profile 2.8 Health Facilities in the District 2.9 Human Resource & Infrastructure 2.10 Equipments 2.11 Rogi Kalyan Samiti 2.12 Support System 2.13 Health Services 2.14 Community Participation 2.15 Training Activities 2.16 BCC Campaigns 2.17 District and Block Level Management 2.18 Health Care Institutions in the District CHAPTER 3- SITUATION ANALYSIS- Page 32 to 40 3.1 Gaps in infrastructure 3.2 Health Sub Centre (HSC) 3.3 Additional PHC (APHC) 3.4 Primary Health Centre 3.5 Sadar Hospital CHAPTER 4 – Setting Objectives and suggested plan of Action – Page -41 to 82 4.1 Introduction 4.2 Targeted objective and suggested strategies 4.3 Meternal Health 4.4 Child Health 4.5 Family Planning 4.6 Institutional strengthening Part- A Programme wise Budget Part- B Programme wise Budget Part- C Programme wise Budget Vitamin A Mamta IDD IDSP VBDCP (Kala-Azar) 1 Foreword Recognizing the importance of Health in the process of economic and social development and improving the quality of life of our citizens, the Government of India has resolved to launch the National Rural Health Mission to carry out necessary architectural correction in the basic health care delivery system . -

Of India 100935 Parampara Foundation Hanumant Nagar ,Ward No
AO AO Name Address Block District Mobile Email Code Number 97634 Chandra Rekha Shivpuri Shiv Mandir Road Ward No 09 Araria Araria 9661056042 [email protected] Development Foundation Araria Araria 97500 Divya Dristi Bharat Divya Dristi Bharat Chitragupt Araria Araria 9304004533 [email protected] Nagar,Ward No-21,Near Subhash Stadium,Araria 854311 Bihar Araria 100340 Maxwell Computer Centre Hanumant Nagar, Ward No 15, Ashram Araria Araria 9934606071 [email protected] Road Araria 98667 National Harmony Work & Hanumant Nagar, Ward No.-15, Po+Ps- Araria Araria 9973299101 [email protected] Welfare Development Araria, Bihar Araria Organisation Of India 100935 Parampara Foundation Hanumant Nagar ,Ward No. 16,Near Araria Araria 7644088124 [email protected] Durga Mandir Araria 97613 Sarthak Foundation C/O - Taranand Mishra , Shivpuri Ward Araria Araria 8757872102 [email protected] No. 09 P.O + P.S - Araria Araria 98590 Vivekanand Institute Of 1st Floor Milan Market Infront Of Canara Araria Araria 9955312121 [email protected] Information Technology Bank Near Adb Chowk Bus Stand Road Araria Araria 100610 Ambedkar Seva Sansthan, Joyprakashnagar Wardno-7 Shivpuri Araria Araria 8863024705 [email protected] C/O-Krishnamaya Institute Joyprakash Nagar Ward No -7 Araria Of Higher Education 99468 Prerna Society Of Khajuri Bazar Araria Bharga Araria 7835050423 [email protected] Technical Education And ma Research 100101 Youth Forum Forbesganj Bharga Araria 7764868759 [email protected] -
AC with District Dist
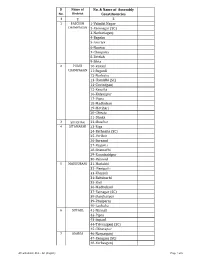
Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 1 PASCHIM 1-Valmiki Nagar CHAMPARAN 2-Ramnagar (SC) 3-Narkatiaganj 4-Bagaha 5-Lauriya 6-Nautan 7-Chanpatia 8-Bettiah 9-Sikta 2 PURVI 10-Raxaul CHAMPARAN 11-Sugauli 12-Narkatia 13-Harsidhi (SC) 14-Govindganj 15-Kesaria 16-Kalyanpur 17-Pipra 18-Madhuban 19-Motihari 20-Chiraia 21-Dhaka 3 SHEOHAR 22-Sheohar 4 SITAMARHI 23-Riga 24-Bathnaha (SC) 25-Parihar 26-Sursand 27-Bajpatti 28-Sitamarhi 29-Runnisaidpur 30-Belsand 5 MADHUBANI 31-Harlakhi 32- Benipatti 33-Khajauli 34-Babubarhi 35-Bisfi 36-Madhubani 37-Rajnagar (SC) 38-Jhanjharpur 39-Phulparas 40-Laukaha 6 SUPAUL 41-Nirmali 42-Pipra 43-Supaul 44-Triveniganj (SC) 45-Chhatapur 7 ARARIA 46-Narpatganj 47-Raniganj (SC) 48-Forbesganj AC with district Dist. - AC (English) Page 1 of 6 Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 49-Araria 50-Jokihat 51-Sikti 8 KISHANGANJ 52-Bahadurganj 53-Thakurganj 54-Kishanganj 55-Kochadhaman 9 PURNIA 56-Amour 57-Baisi 58-Kasba 59-Banmankhi (SC) 60-Rupauli 61-Dhamdaha 62-Purnia 10 KATIHAR 63-Katihar 64-Kadwa 65-Balrampur 66-Pranpur 67-Manihari (ST) 68-Barari 69-Korha (SC) 11 MADHEPURA 70-Alamnagar 71-Bihariganj 72-Singheshwar (SC) 73-Madhepura 12 SAHARSA 74-Sonbarsha (SC) 75-Saharsa 76-Simri Bakhtiarpur 77-Mahishi 13 DARBHANGA 78-Kusheshwar Asthan (SC) 79-Gaura Bauram 80-Benipur 81-Alinagar 82-Darbhanga Rural 83-Darbhanga 84-Hayaghat 85-Bahadurpur 86-Keoti 87-Jale 14 MUZAFFARPUR 88-Gaighat 89-Aurai 90-Minapur 91-Bochaha (SC) 92-Sakra (SC) 93-Kurhani 94-Muzaffarpur 95-Kanti 96-Baruraj AC with district Dist. -

S.No DISTRICT VLE Name Mobile Number ADDRESS 1 ARARIA AMIT
S.No DISTRICT VLE Name Mobile Number ADDRESS ARARIA AMIT THAKUR 8210580921 TIRASKUND ARARIA 1 ARARIA Suman Devi 7070306717 Pipra ghat tola ward no-10 2 KSHITIZ KR ARARIA 8002927600 S/o Dinesh kr chaudhary,vill+po+block palasi,gp miya pur,araria,854333 3 CHOUDHARY SHRAVAN KUMAR 9470261463 / S/o Udichand bhagat,vill - lailokhar (gariyaa),po - pahusi,block+ps - ARARIA 4 BHAGAT 9199722522 kursakaanta,Araria,854332 ARARIA SURAJ JHA 8210905501 S/O-RAJKUMAR JHA,SOGHMARG,ARARIA-854331 5 ARARIA ABUNASAR KHAN 9708226603 VILL-BAIRGACHHI CHOWK,POST-ARARIA-854311 6 ARARIA HARDEV CHOURASIA 8002908166 S/o Udranand chaourasia,vill+po Gunwanti,block Raniganj,Araria,854312 7 S/o Satrudhan pd singh,h.no - 293,vill+po - Kushjhoul,block+ps - ARARIA JITENDRA KR SINGH 9199918908 8 Bhargama,Araria,854318 ARARIA DEWAKAR KUMAR 8210000876 AT-HASANPUR RANIGANJ, PO-MARYGANJ, PS-RANIGANJ 9 S/o Dev shankar roy,vill - mathura east,po+ps+block - narpatganj,dist - Araria,pin - ARARIA Suryabhushan Roy 7979831042 10 854335 S/O MD SHABBIR ALAM CHILHANIYA WARD NO 8 BAGNAGAR GARHBANAILI ARARIA MD ALAM 9939531771 11 JOKIHAT ARARIA RAHUL THAKUR 9430083371 marwari patti,ward no-17 12 9939960471/912348986 ARARIA AJIT KUMAR YADAV MAHISHAKOL ARARIYA 13 6 S/o Chandra kumar mallik,h.no - 42,po - ghurna,block+ps - ARARIA Nigam Kumar 9661213287 14 Narpatganj,Araria,854336 ARARIA Raman Jha 9430634408 S/o Sri Nitya Nand Jha, Vill - Rahatmeena, Block - Kursakanta, Dist - Araria, 15 ARARIA MD ASLAM 9110168570 AT+P.0+P.S-JOKIHAT; DIST-ARARIA 16 RATAN PRABHA W/o Chandan kr mandal,vill - wara/maanikpur,po+block+ps - Forbisganj,Araria - ARARIA 9608725491 17 KUMARI 854318 ARARIA AFROZ ALAM 9771213243 S/O-SHAMSUDDIN,MUSLIM TOLA,WARD NO-1,ARARIA-854311 18 ARARIA ABHILASH PANDIT 7461873031 AMHARA 19 ARARIA RAJESH KUMAR 7004007692 AT-RAJABALAI; P.0-GUNWANTI; P.S-RANIGANJ; ARARIA 20 ARARIA HARE SAH 9955019540 AT BHORHAR PO BHANGHI ARARIA BIHAR 21 S/o Md Salimuddin,vill - budheshwari,po - rampur mohanpur,block+ps+dist - ARARIA MD. -
Note :- in Case of Any Clarification /Objection of Below Mentioned List
INDUSTRIAL TRAINING INSTITUTE, MUZAFFARPUR (Provisional Application List of Guest Faculty) Note :- In case of any clarification /objection of below mentioned List Please provide a written objection with necessary doccument in any working day upto 02-03-2017 at office of Principal, I.T.I Muzaffarpur, Gannipur, Near kalambag chowk, (contact no. 9504694156). No clarification/ Objection will considered after 02-03-2017. Doccument verification and viva will scheduled from 06-03-2017 of District Muzaffarpur Candidates only. CATEGORY - B (RETIRED EMPLOYEE LIST) DISTRICT - MUZAFFARPUR TECH. OTHER BRANCH/ EXPERIE REMARK Sl No. Diary No. / Date Name Father's Name Parmanant Adress QUALIFICATIO QUALIFICAT MARKS % D.OB DISTRICT CATEGORY BRANCH TRADE NCE S N ION 1 425/06-09-2016 ANIL KUMAR HARI SHANKAR VILL+PO - BISHNUPUR B TECH MMV 01-05-1969 MUZAFFARPUR B ex. Army MISHRA MISHRA BAGHANAGARI VIA- DHOLI PS- SAKRA DIST- MUZAFFARPUR 843105 MOB -9931161254 2 1709-16-09-16 SAYED KAISER SAYED AHMAD MOH -KAMRA CHANDWARA ELCTRICAL 54.33 15/08/1947 MUZAFFARPUR B MATH RETIERE IMAM KAJMI HASAN KAJMI MUZAFFARPUR 842001 MOB DIPLOMA IN DIPLOMA IN D - 9835827204 ELEC.ENG. ELEC.ENG. INSTRUC TOR 3 436/07-09-2016 REHAN AHMAD MD. ANAS AT- SIRSAIDYAD COLONEY CTI DMM 01-03-1954 MUZAFFARPUR B RETIRED SIDDIQUE SIDDIQUE NEAR DAV PUBLIC SCHOOL ITI A.S. BEHIND BMP -6 MALIGHAT PO - H.P.O. PS - AHIYAPUR ITI DIST - MUZAFFARPUR 842001 MOB- 9470601665 4 437/07-09-2016 REHAN AHMAD MD. ANAS AT- SIRSAIDYAD COLONEY CTI DMM 01-03-1954 MUZAFFARPUR B DMM RETIRED SIDDIQUE SIDDIQUE NEAR DAV PUBLIC SCHOOL ITI A.S. -

Block: Piro Class-6-8 Subject: Social Science Dist:-Bhojpur Provisional Merit List Block Teacher Niyojan-2019-20
BLOCK TEACHER NIYOJAN-2019-20 BLOCK: PIRO CLASS-6-8 SUBJECT: SOCIAL SCIENCE DIST:-BHOJPUR PROVISIONAL MERIT LIST 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 MATRIC INTER GRADUATION TRAINING FREE BTET/CT WEIG SUM OF AVG OF TAGE APPL.S. NAME OF SE D. FUL MARK ET TOTAL S.N. FATHER DOB ADDRESS CAT DIS. MARKS MARKS FULL MARKS FULL FULL PERCENT PERCEN OF REMARKS N. APPLICANT X FIGH L S MARKS MERIT OBTAI %GE OBTAIN MARK %GE OBTAINE MARK %GE MARK %GE AGE TAGE BTET/ T. MAR OBTAI % NED ED S D S S CTET KS NED MOHD ARANGI-01 NAZIA 1 1776 MONIR 18/4/1995 F USIA UR N N 457 500 91.4 434 600 72.3333 3330 4500 74 1675 2000 83.75 321.4833 80.37 62.66 2 82.371 MONIR ANSARI GHAZIPUR DAYASHAN PRAGYA KAILASHPUR 2 P/197 KAR 22/12/1996 F EWS N N 409 500 81.8 432 500 86.4 740 1000 74 762 1000 76.2 318.4 79.60 68 2 81.6 PANDEY I BUXAR PANDEY NEERAJ BHRIGUNA BIHIYA 3 976 KUMAR 02.01.1993 M UR N N 403 500 80.6 413 500 82.6 964 1500 64.2667 1064 1300 81.8462 309.3128 77.33 72.41 4 81.328 TH MISHRA BHOJPUR MISHRA SHREE DEVRADH, SUNITA 4 1785 DHAR 03.01.1986 F TIYAR, EWS N N 537 700 76.7143 683 900 75.8889 1179 1500 78.6 1054 1300 81.0769 312.2801 78.07 55.33 2 80.07 KUMARI DUBEY BHOJPUR VIPUL NAWAL GAUSGANJA 5 1770 KUMAR KISHOR 01.04.1979 M UR N N 711 900 79 693 900 77 1177 1500 78.4667 1834 2400 76.4167 310.8833 77.72 62.66 2 79.721 RA SINGH SINGH DHAMANIA, HIMANSHU RAMESHW 6 424 26/01/1996 M GARAHANI, EBC N N 419 500 83.8 350 500 70 722 1000 72.2 998 1300 76.7692 302.7692 75.69 70.67 4 79.692 SHEKHAR AR PRASAD BHOJPUR ROHAI, ASHWANI -

By Er. Narendra Kumar Tiwary (Ph.D Scholar, IIT Delhi) Professor, Research, ARP, & PIM, Water and Land Management Institute (WALMI), Patna, India Prof
By Er. Narendra Kumar Tiwary (Ph.D Scholar, IIT Delhi) Professor, Research, ARP, & PIM, Water and Land Management Institute (WALMI), Patna, India Prof. A.K.Gosain, IIT Delhi Prof.A.K.Keshari ,IIT Delhi Prof. Rakesh Khosa , IIT Delhi Dr. S. K. Srivastava, Reader, WALMI, Patna Department of Civil Engineering, IIT, Delhi Use of New Technologies & Softwares in Flood sector Drainage Map of the Bagmati Basin ± Legend Drainage lines 20 10 0 20 40 60 Km Basin boundary INTRODUCTION Flood is associated with a serious loss of life, property and damage to utilities. Climate change is going to further aggravate the scenario Strong call for action to combat the problem of flood inundation, a natural calamity induced by some super power is needed 14-10-2015 3 THREE EVENTS WHICH MOTIVATE ME TO TAKE UP THE CHALLENGING RESEARCH WORK EVENT- I In September 2014, Heavy Rainfall centered on the North Indian state of Jammu and Kashmir caused devastating floods and landslides in the country's worst natural disaster since the 1944 Kashmir Flood Disaster. More than 700 people were "presumed dead. Destruction of bridges and roads left about more than 100,000 pilgrims and tourists trapped in the valleys 14-10-2015 4 Event-2 In June 2013, a multi-day cloudburst centered on the North Indian state of Uttarakhand caused devastating floods and landslides in the country's worst natural disaster since the 200 4 tsunami more than 5,700 people were "presumed dead. Destruction of bridges and roads left about 100,000 pilgrims and tourists trapped in the valleys 14-10-2015 -

Pradhan Mantri Gram Sadak Yojana CUCPL - Comprehensive Up-Gradation Cum Consolidation Priority List
Pradhan Mantri Gram Sadak Yojana CUCPL - Comprehensive Up-gradation cum Consolidation Priority List State : Bihar District : All Districts Block : All Blocks Sr.No. State District Block Plan CN Plan Road Name Plan Road Route Educati Medical Veterin Transp Market Administ Populatio Total Score Per Avg PCI Road No. Length Priority onal Faciliti ary ort and Faciliti rative n Score Unit Services es Facilitie Commu es Centres Length s nicatio n Infrastr ucture 1 Bihar Arwal Arwal MRL01 Walidad, T01 To Khamhaini 10.835 M 12 0 0.00 0.00 0.00 1 68 81.00 7.48 1.00 2 Bihar Arwal Banshi MRL02 Manjhiyama to Khatangi 9.465 M 16 8 0.00 9.00 0.00 1 77 111.00 11.73 1.00 Surajpur 3 Bihar Arwal Banshi MRL03 Kharasi to Belaura 14.943 M 22 8 0.00 3.00 0.00 1 89 123.00 8.23 1.00 Surajpur 4 Bihar Arwal Banshi MRL01 Khatangi senari RD to Mobarakpur 10.860 M 9 4 0.00 3.00 0.00 1 42 59.00 5.43 1.00 Surajpur 5 Bihar Arwal Kaler MRL01 Sohasa Road L037 To Masadpur 21.676 M 10 6 0.00 6.00 0.00 1 54 77.00 3.55 1.00 6 Bihar Arwal Karpi MRL02 Imamganj Deokund Road,T04 To Jonha 7.365 M 22 8 3.00 11.00 9.00 2 91 146.00 19.82 1.00 7 Bihar Arwal Karpi MRL01 Karpi Barahmile Road, T03 To Salarpur 12.365 M 18 6 0.00 9.00 7.00 2 104 146.00 11.81 1.00 8 Bihar Arwal Karpi MRL03 Arwal Jehanabad Road, T02 To Aiyara 16.787 M 7 0 0.00 0.00 7.00 1 52 67.00 3.99 1.00 9 Bihar Arwal Kurtha MRL02 Salarpur L042, To Dhamaul 15.238 M 9 4 0.00 3.00 7.00 2 88 113.00 7.42 1.00 10 Bihar Arwal Kurtha MRL01 Pinjrawan to Manepaker 9.456 M 8 2 0.00 0.00 0.00 1 55 66.00 6.98 1.00 11 Bihar Aurangabad