Toxic Anterior Segment Syndrome After an Uncomplicated Vitrectomy with Epiretinal Membrane Peeling
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Is This Important? Phone Triage) and Physical Exam
Goals Diagnostic Dilemmas Learn which features of the history and 1. What is the cause of this patient’s red eye? physical examination are most useful 2. Does this patient have a pathologic headache? Use risk scores and clinical decision tools 3. Does this patient have endocarditis? Distinguish benign from potentially serious 4. What is the cause of this patient’s back pain? conditions Identify clinical pearls and pitfalls What is the Cause of this Patient’s Mr. Ira Tatedi Red Eye? 32 year old man with one day h/o mild redness of OD, pain, and photophobia. Physical exam shows circumcorneal injection, and visual acuity is 20/80. Key Elements of History (including Why is this Important? Phone Triage) and Physical Exam Most cases of red eye are caused by viral History and Triage Physical Examination conjunctivitis, which does not generally Is vision affected? Visual acuity require any treatment Is there a foreign Pupil size/reactivity Some cases are caused by bacterial or allergic body sensation? Discharge conjunctivitis, for which specific treatment is Is there Pattern of redness indicated photophobia? Foreign body A minority of cases are caused by other Was there trauma? Hypopyon/hyphema conditions, which require urgent or emergent Are patient a contact referral to an ophthalmologist lens wearer? It is essential to be able to distinguish them Is there discharge from one another throughout the day? Anatomy/Differential Diagnosis Conjunctivitis Viral Conjunctivitis – Erythema with co-existing URI – Watery, serous discharge -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Challenges in Ophthalmic Pathology: the Vitreoretinal Membrane Biopsy
Challenges in PAUL HISCOTT, DAVID WONG, IAN GRIERSON ophthalmic pathology: The vitreoretinal membrane biopsy Abstract detachment.s Sheets or strands crossing the vitreous are sometimes called transvitreous The introduction of vitreoretinal microsurgery membranes. Anteriorly, membranes can arise has produced a new type of biopsy; that of the in, or be continuous with, the vitreous base and vitreoretinal membrane. This review even extend as far as the posterior iris surface or investigates methods by which these scar-like pupil. tissues are handled in the laboratory and Biopsies of pathological tissue are usually explores the implications of the results of such undertaken to establish a diagnosis. evaluations. The study of vitreoretinal Vitreoretinal biopsies also may be for diagnostic membrane biopsies has provided much purposes as, for example, in the case of information concerning the pathobiology of intraocular lymphoma, but such conditions are the various conditions which may give rise to rare and tend not to produce membranes. the tissue as well as insights into how Conversely, in the conditions which do produce membranes themselves develop. Moreover, membranes the diagnosis is seldom in doubt. the application of new laboratory techniques Why, then, attempt laboratory studies of is expected to enhance our understanding of vitreoretinal membranes? Laboratory findings the formation of vitreoretinal membranes, and from the membranes may have a number of lead to further advances in their surgical and uses, for example providing 'feed-back' to the medical management. surgeon concerning surgical dissection planes Key words Age-related macular degeneration, (see below). However, the principal objective of Epiretinal membrane, Proliferative diabetic these investigations is to improve our retinopathy, Proliferative vitreoretinopathy, understanding of the pathogenesis of P Hiscott D. -

SHOULD YOU OPEN a DRY-EYE CLINIC? Experts Help You Weigh the Pros and Cons
RETINAL PHOTOS ON THE GO P. 16 • CHANGES TO MEDICARE ABN FORMS P. 20 ENSURING A HAPPY CATARACT PATIENT P. 22 • MANAGING GLAUCOMA IN KPRO PATIENTS P. 58 THE CURRENT STATE OF VITREORETINAL EDUCATION P. 64 • WILLS EYE RESIDENT CASE REPORT P. 70 September 2020 reviewofophthalmology.com SHOULD YOU OPEN A DRY-EYE CLINIC? Experts help you weigh the pros and cons. P. 28 ALSO INSIDE: • The Latest Treatments for Dry Eye P. 38 • Comprehensive Ophthalmologists and Anti-VEGF Injections P. 48 • How to Manage Ocular Herpes P. 54 SHE MAY NEED MORE THAN ARTIFICIAL TEARS TO DISRUPT INFLAMMATION IN DRY EYE DISEASE1,2 Her eyes deserve a change. Choose twice-daily Xiidra for lasting relief that can start as early as 2 weeks.3*† Not an actual patient. *In some patients with continued daily use. One drop in each eye, twice daily (approximately 12 hours apart).3 †XiidraisanLFA-1antagonistforthetreatmentofdryeyedisease.Pivotaltrialdata:ThesafetyandefficacyofXiidrawereassessedinfour Important Safety Information (cont) 12-week,randomized,multicenter,double-masked,vehicle-controlledstudies(N=2133).Patientsweredosedtwicedaily.Useofartificial • I n clinicaltrials,themostcommonadversereactionsreportedin5-25%ofpatientswereinstillationsite tearswasnotallowedduringthestudies.Thestudyendpointsincludedassessmentofsigns(basedonInferiorfluoresceinCornealStaining irritation,dysgeusiaandreducedvisualacuity.Otheradversereactionsreportedin1%to5%ofthepatients Score [ICSS] on a scale of 0 to 4) and symptoms (based on patient-reported Eye Dryness Score [EDS] on a visual analogue scale of 0 to 100).3 were blurred vision, conjunctival hyperemia, eye irritation, headache, increased lacrimation, eye discharge, A larger reduction in EDS favoring Xiidra was observed in all studies at day 42 and day 84. Xiidra reduced symptoms of eye dryness at eye discomfort, eye pruritus and sinusitis. 2 weeks (based on EDS) compared to vehicle in 2 out of 4 clinical trials. -

Exploring Topical Anti-Glaucoma Medication Effects on the Ocular Surface in the Context of the Current Understanding of Dry Eye
The Ocular Surface 16 (2018) 289e293 Contents lists available at ScienceDirect The Ocular Surface journal homepage: www.theocularsurface.com Original Research Exploring topical anti-glaucoma medication effects on the ocular surface in the context of the current understanding of dry eye Aaron B.C. Wong, Michael T.M. Wang, Kevin Liu, Zak J. Prime, Helen V. Danesh-Meyer, * Jennifer P. Craig Department of Ophthalmology, New Zealand National Eye Centre, The University of Auckland, New Zealand article info abstract Article history: Purpose: To assess tear film parameters, ocular surface characteristics, and dry eye symptomology in Received 11 November 2017 patients receiving topical anti-glaucoma medications. Received in revised form Methods: Thirty-three patients with a diagnosis of open angle glaucoma or ocular hypertension, 26 February 2018 receiving unilateral topical anti-glaucoma medication for at least 6 months, were recruited in a cross- Accepted 2 March 2018 sectional, investigator-masked, paired-eye comparison study. Tear film parameters, ocular surface characteristics, and dry eye symptomology of treated and fellow eyes were evaluated and compared. Keywords: Results: The mean ± SD age of the participants was 67 ± 12 years, and the mean ± SD treatment duration Glaucoma ± fi ¼ fi Prostaglandin analogue was 5.3 4.4 years. Treated eyes had poorer non-invasive tear lm breakup time (p 0.03), tear lm ¼ ¼ Tear film osmolarity (p 0.04), bulbar conjunctival hyperaemia (p 0.04), eyelid margin abnormality grade Ocular surface (p ¼ 0.01), tear meniscus height (p ¼ 0.03), and anaesthetised Schirmer value (p ¼ 0.04) than fellow eyes. Dry eye There were no significant differences in dry eye symptomology, meibomian gland assessments, and Meibomian gland ocular surface staining between treated and fellow eyes (all p > 0.05). -

CAUSES, COMPLICATIONS &TREATMENT of A“RED EYE”
CAUSES, COMPLICATIONS & TREATMENT of a “RED EYE” 8 Most cases of “red eye” seen in general practice are likely to be conjunctivitis or a superficial corneal injury, however, red eye can also indicate a serious eye condition such as acute angle glaucoma, iritis, keratitis or scleritis. Features such as significant pain, photophobia, reduced visual acuity and a unilateral presentation are “red flags” that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features to know which patients require referral to an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? inflammation of the choroid (choroiditis). Complications include glaucoma, cataract and macular oedema. The most likely cause of a red eye in patients who present to 4. Scleritis is inflammation of the sclera. This is a very rare general practice is conjunctivitis. However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease, e.g. rheumatoid arthritis. treatment due to a missed diagnosis can result in permanent 5. Penetrating eye injury or embedded foreign body; red visual loss. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes to antimicrobial 6. Acid or alkali burn to the eye resistance. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access to specialised or chemical burn to the eye, but further assessment may be equipment for eye examination, e.g. -
UVEITIS Eye74 (1)
UVEITIS Eye74 (1) Uveitis Last updated: May 9, 2019 Classification .................................................................................................................................... 1 Etiologic categories .......................................................................................................................... 2 Treatment ......................................................................................................................................... 2 Complications ................................................................................................................................... 2 COMMON UVEITIC SYNDROMES ............................................................................................................. 2 Masquerade Syndromes ................................................................................................................... 3 UVEITIS - heterogenous ocular diseases - inflammation of any component of uveal tract (iris, ciliary body, choroid). CLASSIFICATION ANTERIOR UVEITIS (most common uveitis) - localized to anterior segment - iritis and iridocyclitis. IRITIS - white cells confined solely to anterior chamber. IRIDOCYCLITIS - cellular activity also involves retrolental vitreous. etiology (most do not have underlying systemic disease): 1) idiopathic postviral syndrome (most commonly 38-60%) 2) HLA-B27 syndromes, many arthritic syndromes (≈ 17%) 3) trauma (5.7%) 4) herpes simplex, herpes zoster disease (1.9-12.4%) 5) iatrogenic (postoperative). tends to -

Macular Hole Formation Following Choroidal Neovascularization
Yoshida et al., Int J Ophthalmol Clin Res 2015, 2:1 International Journal of ISSN: 2378-346X Ophthalmology and Clinical Research Case Report: Open Access Macular Hole Formation Following Choroidal Neovascularization Treatment in A High Myopic Eye with Epiretinal Membrane Yusaku Yoshida*, Manabu Yamamoto, Takeya Kohno and Kunihiko Shiraki Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, Japan *Corresponding author: Yusaku Yoshida, MD, Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan, Fax:+81-666-343- 873, E-mail: [email protected] macular hole development where post-treatment regression of CNV Abstract seemed to have played a major role in a high myopic eye with ERM. Purpose: To report on the development of macular hole after treatment of choroidal neovascularization (CNV) in a patient with Case high myopia and epiretinal membrane (ERM). A 60-year-old man was examined in the Department of Methods: Retrospective single case report. Ophthalmology of Osaka City University Hospital for reduced vision Patients: A 60-year-old man presented with reduced vision in his in his right eye in January 2009. On initial examination, decimal best- right eye. On the initial examination, the right eye was high myopic corrected visual acuity (BCVA) was 0.3 in the right eye and 1.5 in with decimal best-corrected visual acuity (BCVA) of 0.3. the left eye, while intraocular pressures were 13 and 14 mmHg in the right and left eye, respectively. His previous medical and family Results: A subretinal grayish-white lesion was seen at the macula with hemorrhage, and optical coherence tomography showed a histories included nothing of note. -
Epiretinal Membrane
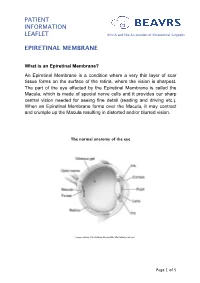
PATIENT INFORMATION LEAFLET British and Eire Association of Vitreoretinal Surgeons EPIRETINAL MEMBRANE What is an Epiretinal Membrane? An Epiretinal Membrane is a condition where a very thin layer of scar tissue forms on the surface of the retina, where the vision is sharpest. The part of the eye affected by the Epiretinal Membrane is called the Macula, which is made of special nerve cells and it provides our sharp central vision needed for seeing fine detail (reading and driving etc.). When an Epiretinal Membrane forms over the Macula, it may contract and crumple up the Macula resulting in distorted and/or blurred vision. The normal anatomy of the eye *Image courtesy of the National Eye Institute http://www.nei.nih.gov Page 1 of 5 PATIENT INFORMATION British and Eire Association of Vitreoretinal Surgeons LEAFLET EPIRETINAL MEMBRANE Why do I have an Epiretinal Membrane? In most cases the development of an Epiretinal Membrane appears to be related to normal aging changes inside the eye. In some cases it can be related to other conditions such as diabetes, blockage of blood vessel, inflammation or following retinal surgery. Epiretinal membranes are not related to Macular Degeneration. Epiretinal Membranes do not usually affect the other eye. They are quite common and affect up to 8% of people in later years. Cross-section of a healthy macula Cross-section of a macula with an epiretinal membrane Assessment for Epiretinal Membrane Your eye doctor is able to detect an Epiretinal Membrane during an eye examination following the use of eye drops that temporarily make your pupils large. -

View Returned the Following Day, Less Than OR
s s CONSEQUENTIAL CASES CASES THAT CHANGED THE WAY WE PRACTICE Three retina specialists share stories of patient encounters that left lasting impressions. LET THERE BE LIGHT By Ninel Z. Gregori, MD vision requires daily practice and hard my career in the direction of other A 52-year-old patient work. The patient had an intense innovative surgeries and clinical trials who had seen nothing rehabilitation process ahead of her at Bascom Palmer. but weak light for to help her to make sense of the And it did much more: It helped me 19 years since devel- lights. She is now able to identify light truly understand and appreciate the oping end-stage retinitis pigmentosa objects against dark backgrounds, value of careful preoperative counsel- (RP) came into my care. Then, in 2013, sort light and dark clothes, see light ing and setting realistic expectations the long-awaited promise of artificial coming in the windows, identify the for patients undergoing new treat- vision became a reality because the handle on the refrigerator, and even ments. After observing the experiences US FDA had approved the first retinal identify some letters, numbers, and of my patient receiving an Argus II prosthesis for patients with RP. I dis- simple words on a computer screen. implant, I now make sure to carefully cussed the Argus II Retinal Prosthesis She cannot, however, recognize explain the risks and limitations of System (Second Sight) with the objects and people in the environ- artificial vision options to patients who patient, and we agreed that she was a ment consistently, see faces, or read. -

Ocular Inflammation Associated with Systemic Infection
Byung Gil Moon, et al. • Ocular Inflammation Associated with Systemic Infection HMR Review Ocular Inflammation Associated with Systemic Infection Hanyang Med Rev 2016;36:192-202 http://dx.doi.org/10.7599/hmr.2016.36.3.192 pISSN 1738-429X eISSN 2234-4446 Byung Gil Moon, Joo Yong Lee Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea Systemic infections that are caused by various types of pathogenic organisms can be spread Correspondence to: Joo Yong Lee Department of Ophthalmology, Asan to the eyes as well as to other solid organs. Bacteria, parasites, and viruses can invade the Medical Center, University of Ulsan eyes via the bloodstream. Despite advances in the diagnosis and treatment of systemic in- College of Medicine, 88 Olympic-ro fections, many patients still suffer from endogenous ocular infections; this is particularly 43-gil, Songpa-gu, Seoul 05505, Korea Tel: +82-2-3010-3976 due to an increase in the number of immunosuppressed patients such as those with hu- Fax: +82-2-470-6440 man immunodeficiency virus infection, those who have had organ transplantations, and E-mail: [email protected] those being administered systemic chemotherapeutic and immunomodulating agents, which may increase the chance of ocular involvement. In this review, we clinically evalu- Received 2 July 2016 Revised 21 July 2016 ated posterior segment manifestations in the eye caused by hematogenous penetration Accepted 27 July 2016 of systemic infections. We focused on the conditions that ophthalmologists encounter This is an Open Access article distributed under most often and that require cooperation with other medical specialists. -

Endophthalmitis
RETINA HEALTH SERIES | Facts from the ASRS The Foundation American Society of Retina Specialists Committed to improving the quality of life of all people with retinal disease. Endophthalmitis is an infection inside the eye SIGNS AND SYMPTOMS that can either be acute or chronic, meaning that it can develop very rapidly which is most common, or develop Endophthalmitis causes the white slowly and persist for long periods of time of the eye to be inflamed. There may be a white or yellow discharge on or inside the eyelid, and the cornea may show a white cloud- iness. There may also be a layer of white cells (hypopyon) present within the anterior chamber of the eye between the iris and the cornea. (Figure 1) Endophthalmitis is usually a very serious problem and prompt examination by an ophthalmologist is essential to make an appropriate diagnosis and initiate treatment. Other symptoms include: • Eye pain and redness • Decreased vision • Trouble looking at bright lights (photophobia), usually sudden onset Figure 1 Hypopyon is an accumulation of white blood cells in the anterior chamber of the eye and corneal WHAT IS THE RETINA? infiltrate associated with infectious endophthalmitis. Image courtesy of ©Retina Image Bank, contributed by Aleksandra V. Rachitskay, MD, Cole Eye Institute, Cleveland Clinic. 2014. Image 16250. Causes: Acute cases of endophthalmitis are caused by gram-positive (or less frequently gram-negative) bacteria and are most often seen within 6 weeks after surgery or trauma to the eye. Chronic cases that occur outside of the 6-week window are often related to a previous surgery and are commonly caused by slowly progressive infections such as Propionibacterium acnes or fungus.