Keratoconus and Cone-Rod Dystrophy Among Brothers: Clinical Case Study and Genetic Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Challenges in Ophthalmic Pathology: the Vitreoretinal Membrane Biopsy
Challenges in PAUL HISCOTT, DAVID WONG, IAN GRIERSON ophthalmic pathology: The vitreoretinal membrane biopsy Abstract detachment.s Sheets or strands crossing the vitreous are sometimes called transvitreous The introduction of vitreoretinal microsurgery membranes. Anteriorly, membranes can arise has produced a new type of biopsy; that of the in, or be continuous with, the vitreous base and vitreoretinal membrane. This review even extend as far as the posterior iris surface or investigates methods by which these scar-like pupil. tissues are handled in the laboratory and Biopsies of pathological tissue are usually explores the implications of the results of such undertaken to establish a diagnosis. evaluations. The study of vitreoretinal Vitreoretinal biopsies also may be for diagnostic membrane biopsies has provided much purposes as, for example, in the case of information concerning the pathobiology of intraocular lymphoma, but such conditions are the various conditions which may give rise to rare and tend not to produce membranes. the tissue as well as insights into how Conversely, in the conditions which do produce membranes themselves develop. Moreover, membranes the diagnosis is seldom in doubt. the application of new laboratory techniques Why, then, attempt laboratory studies of is expected to enhance our understanding of vitreoretinal membranes? Laboratory findings the formation of vitreoretinal membranes, and from the membranes may have a number of lead to further advances in their surgical and uses, for example providing 'feed-back' to the medical management. surgeon concerning surgical dissection planes Key words Age-related macular degeneration, (see below). However, the principal objective of Epiretinal membrane, Proliferative diabetic these investigations is to improve our retinopathy, Proliferative vitreoretinopathy, understanding of the pathogenesis of P Hiscott D. -

SHOULD YOU OPEN a DRY-EYE CLINIC? Experts Help You Weigh the Pros and Cons
RETINAL PHOTOS ON THE GO P. 16 • CHANGES TO MEDICARE ABN FORMS P. 20 ENSURING A HAPPY CATARACT PATIENT P. 22 • MANAGING GLAUCOMA IN KPRO PATIENTS P. 58 THE CURRENT STATE OF VITREORETINAL EDUCATION P. 64 • WILLS EYE RESIDENT CASE REPORT P. 70 September 2020 reviewofophthalmology.com SHOULD YOU OPEN A DRY-EYE CLINIC? Experts help you weigh the pros and cons. P. 28 ALSO INSIDE: • The Latest Treatments for Dry Eye P. 38 • Comprehensive Ophthalmologists and Anti-VEGF Injections P. 48 • How to Manage Ocular Herpes P. 54 SHE MAY NEED MORE THAN ARTIFICIAL TEARS TO DISRUPT INFLAMMATION IN DRY EYE DISEASE1,2 Her eyes deserve a change. Choose twice-daily Xiidra for lasting relief that can start as early as 2 weeks.3*† Not an actual patient. *In some patients with continued daily use. One drop in each eye, twice daily (approximately 12 hours apart).3 †XiidraisanLFA-1antagonistforthetreatmentofdryeyedisease.Pivotaltrialdata:ThesafetyandefficacyofXiidrawereassessedinfour Important Safety Information (cont) 12-week,randomized,multicenter,double-masked,vehicle-controlledstudies(N=2133).Patientsweredosedtwicedaily.Useofartificial • I n clinicaltrials,themostcommonadversereactionsreportedin5-25%ofpatientswereinstillationsite tearswasnotallowedduringthestudies.Thestudyendpointsincludedassessmentofsigns(basedonInferiorfluoresceinCornealStaining irritation,dysgeusiaandreducedvisualacuity.Otheradversereactionsreportedin1%to5%ofthepatients Score [ICSS] on a scale of 0 to 4) and symptoms (based on patient-reported Eye Dryness Score [EDS] on a visual analogue scale of 0 to 100).3 were blurred vision, conjunctival hyperemia, eye irritation, headache, increased lacrimation, eye discharge, A larger reduction in EDS favoring Xiidra was observed in all studies at day 42 and day 84. Xiidra reduced symptoms of eye dryness at eye discomfort, eye pruritus and sinusitis. 2 weeks (based on EDS) compared to vehicle in 2 out of 4 clinical trials. -

Exploring Topical Anti-Glaucoma Medication Effects on the Ocular Surface in the Context of the Current Understanding of Dry Eye
The Ocular Surface 16 (2018) 289e293 Contents lists available at ScienceDirect The Ocular Surface journal homepage: www.theocularsurface.com Original Research Exploring topical anti-glaucoma medication effects on the ocular surface in the context of the current understanding of dry eye Aaron B.C. Wong, Michael T.M. Wang, Kevin Liu, Zak J. Prime, Helen V. Danesh-Meyer, * Jennifer P. Craig Department of Ophthalmology, New Zealand National Eye Centre, The University of Auckland, New Zealand article info abstract Article history: Purpose: To assess tear film parameters, ocular surface characteristics, and dry eye symptomology in Received 11 November 2017 patients receiving topical anti-glaucoma medications. Received in revised form Methods: Thirty-three patients with a diagnosis of open angle glaucoma or ocular hypertension, 26 February 2018 receiving unilateral topical anti-glaucoma medication for at least 6 months, were recruited in a cross- Accepted 2 March 2018 sectional, investigator-masked, paired-eye comparison study. Tear film parameters, ocular surface characteristics, and dry eye symptomology of treated and fellow eyes were evaluated and compared. Keywords: Results: The mean ± SD age of the participants was 67 ± 12 years, and the mean ± SD treatment duration Glaucoma ± fi ¼ fi Prostaglandin analogue was 5.3 4.4 years. Treated eyes had poorer non-invasive tear lm breakup time (p 0.03), tear lm ¼ ¼ Tear film osmolarity (p 0.04), bulbar conjunctival hyperaemia (p 0.04), eyelid margin abnormality grade Ocular surface (p ¼ 0.01), tear meniscus height (p ¼ 0.03), and anaesthetised Schirmer value (p ¼ 0.04) than fellow eyes. Dry eye There were no significant differences in dry eye symptomology, meibomian gland assessments, and Meibomian gland ocular surface staining between treated and fellow eyes (all p > 0.05). -

Rod-Cone Dystrophy Associated with the Gly167asp Variant in PRPH2
Rod-cone dystrophy associated with the Gly167Asp variant in PRPH2 Rola Ba-Abbad, FRCS, PhD1,2, Anthony G. Robson, PhD1,2, Becky MacPhee, BSc2, Andrew R. Webster, MD(Res), FRCOpth1,2, Michel Michaelides, MD(Res), FRCOphth 1,2 1. UCL Institute of Ophthalmology, University College London, London, UK 2. Moorfields Eye Hospital, London, UK Declaration of interest statement: the authors report no conflict of interest. Corresponding Author: Professor Michel Michaelides, MD(Res), FRCOphth UCL Institute of Ophthalmology, London, EC1V 9EL, United Kingdom Email: [email protected] Phone number: +44 (0) 20 7608 6800 Peripherin 2-associated retinopathies are phenotypically heterogenous and can present as autosomal dominant retinitis pigmentosa, cone-rod dystrophy, various forms of macular and pattern dystrophy, or recessive retinopathy1,2. We report a case of rod-cone dystrophy associated with the variant c.500G>A, p.(Gly167Asp) in PRPH2 (OMIM 179605), which was previously reported to cause autosomal dominant butterfly-shaped pigment dystrophy of the fovea in a three-generation pedigree (MIM 169150)3. A 66-year old British woman of European ancestry was referred to the inherited retinal disorders clinic with bilateral pigmentary retinopathy, and a 5-year history of nyctalopia. There were no knowingly affected family members; her late father and mother had normal vision in their sixties and eighties respectively, and the patient’s two children had no symptoms in their third decade of life. Previously, she underwent laser refractive surgery for myopia, bilateral cataract extraction and laser posterior capsulotomy. On examination, the Snellen visual acuity was 20/30 in the right eye, and 20/80 in the left eye; and color vision (Ishihara plates) was normal bilaterally. -

DJO Macular Dystrophy in a Post LASIK Patient
DJO Vol. 30, No. 3, January-March 2020 Case Report Macular Dystrophy in a Post LASIK Patient Sanjana Vatsa, Shana Sood Dr. Agarwal Eye Hospital, Chennai, Tamil Nadu, India LASIK (Laser Assisted Insitu keratomileusis) is the most commonly performed refractive surgery worldwide. A detailed pre operative and post operative evaluation of the anterior and posterior segment is a must. A 35 year old male patient with a history of LASIK surgery done 13 years back presented to us with complaint of painless, progressive diminution of vision in both eyes from past Abstract 2 years. Dilated retinal examination showed bulls eye maculopathy in both eyes. Macular OCT showed gross reduction in central foveal thickness. ERG showed marked reduction in photopic responses suggestive of a cone dystrophy. Treatment aims at alleviating the symptoms and use of low vision aids. Genetic counselling may be of benefit for affected individuals and their families. Delhi J Ophthalmol 2020;30;60-62; Doi http://dx.doi.org/10.7869/djo.529 Keywords: LASIK, Bulls eye maculopathy, cone dystrophy, genetic counselling. Introduction LASIK is the most popular and commonly performed refractive surgery worldwide.1 Along with anterior segment, a detailed evaluation of the posterior segment is a must on follow up visits to rule out any retinal lesions such as degenerations, dystrophies, maculopathy etc; as these can occur irrespective of any procedure performed. Case Report A 35 year old male patient came to us with a history of LASIK surgery done 13 years back in both eyes for a power of -7.0D sphere. Patient was comfortable with his vision after surgery and had no complaints for 11 years, after which he noticed blurring of vision in both eyes (more in the left eye). -

Macular Hole Formation Following Choroidal Neovascularization
Yoshida et al., Int J Ophthalmol Clin Res 2015, 2:1 International Journal of ISSN: 2378-346X Ophthalmology and Clinical Research Case Report: Open Access Macular Hole Formation Following Choroidal Neovascularization Treatment in A High Myopic Eye with Epiretinal Membrane Yusaku Yoshida*, Manabu Yamamoto, Takeya Kohno and Kunihiko Shiraki Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, Japan *Corresponding author: Yusaku Yoshida, MD, Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan, Fax:+81-666-343- 873, E-mail: [email protected] macular hole development where post-treatment regression of CNV Abstract seemed to have played a major role in a high myopic eye with ERM. Purpose: To report on the development of macular hole after treatment of choroidal neovascularization (CNV) in a patient with Case high myopia and epiretinal membrane (ERM). A 60-year-old man was examined in the Department of Methods: Retrospective single case report. Ophthalmology of Osaka City University Hospital for reduced vision Patients: A 60-year-old man presented with reduced vision in his in his right eye in January 2009. On initial examination, decimal best- right eye. On the initial examination, the right eye was high myopic corrected visual acuity (BCVA) was 0.3 in the right eye and 1.5 in with decimal best-corrected visual acuity (BCVA) of 0.3. the left eye, while intraocular pressures were 13 and 14 mmHg in the right and left eye, respectively. His previous medical and family Results: A subretinal grayish-white lesion was seen at the macula with hemorrhage, and optical coherence tomography showed a histories included nothing of note. -
Epiretinal Membrane
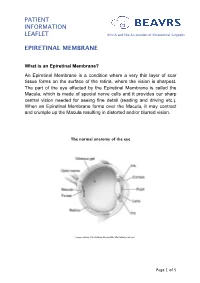
PATIENT INFORMATION LEAFLET British and Eire Association of Vitreoretinal Surgeons EPIRETINAL MEMBRANE What is an Epiretinal Membrane? An Epiretinal Membrane is a condition where a very thin layer of scar tissue forms on the surface of the retina, where the vision is sharpest. The part of the eye affected by the Epiretinal Membrane is called the Macula, which is made of special nerve cells and it provides our sharp central vision needed for seeing fine detail (reading and driving etc.). When an Epiretinal Membrane forms over the Macula, it may contract and crumple up the Macula resulting in distorted and/or blurred vision. The normal anatomy of the eye *Image courtesy of the National Eye Institute http://www.nei.nih.gov Page 1 of 5 PATIENT INFORMATION British and Eire Association of Vitreoretinal Surgeons LEAFLET EPIRETINAL MEMBRANE Why do I have an Epiretinal Membrane? In most cases the development of an Epiretinal Membrane appears to be related to normal aging changes inside the eye. In some cases it can be related to other conditions such as diabetes, blockage of blood vessel, inflammation or following retinal surgery. Epiretinal membranes are not related to Macular Degeneration. Epiretinal Membranes do not usually affect the other eye. They are quite common and affect up to 8% of people in later years. Cross-section of a healthy macula Cross-section of a macula with an epiretinal membrane Assessment for Epiretinal Membrane Your eye doctor is able to detect an Epiretinal Membrane during an eye examination following the use of eye drops that temporarily make your pupils large. -

The Role of Erg/Vep and Eye Movement Recordings in Children with Ocular Motor Apraxia
THE ROLE OF ERG/VEP AND EYE MOVEMENT RECORDINGS IN CHILDREN WITH OCULAR MOTOR APRAXIA FATIMA S. SHAWKAT, CHRISTOPHER M. HARRIS, DAVID S. I. TAYLOR and ANTHONY KRISS London SUMMARY several reports of OMA or saccade failure occurring Ocular motor apraxia (OMA) is characterised by an congenitally, with no other clinical entity?-5 How intermittent inability to initiate voluntary sacca des, and ever, it can also occur as part of a wider neurological a failure to produce optokinetic and vestibular quick disorder: for example with structural brain abnorm phases. Some patients have no other abnormalities alities, such as agenesis of the corpus callosum6 and (idiopathic OMA), whereas in others it appears vermis hypoplasia;7 with neurodegenerative condi associated with a variety of neurological conditions tions;8 and with acquired neurological disease such as which may affect the sensory visual pathway. Electro posterior fossa tumours,9 ataxia telangiectasia,lO retinograms (ERGs), flash and pattern visual evoked fronto-parietal lesions,l1.l2 occipital cortex lesions,13 potentials (VEPs) and eye movements were assessed in cerebellar and brains tern neoplasm14 and olivoponto 53 children with OMA (age range 17 days to 14 years) cerebellar degeneration. 15.16 The inability to gener to determine their efficacy in helping to distinguish ate saccades often leads to the development of between idiopathic and non-idiopathic cases. Seven patients (13.2%) had idiopathic OMA and the remain compensatory behaviour to shift direction of gaze; ing 46 (86.8%) had other associated clinical conditions. this includes headthrusting, blinking and tilted head All patients had episodes of absent quick phases ('lock posture, which enables the use of vertical eye up') during optokinetic nystagmus (OKN) and/or movements that are usually unaffected. -

Progressive Cone and Cone-Rod Dystrophies
Br J Ophthalmol: first published as 10.1136/bjophthalmol-2018-313278 on 24 January 2019. Downloaded from Review Progressive cone and cone-rod dystrophies: clinical features, molecular genetics and prospects for therapy Jasdeep S Gill,1 Michalis Georgiou,1,2 Angelos Kalitzeos,1,2 Anthony T Moore,1,3 Michel Michaelides1,2 ► Additional material is ABSTRact proteins involved in photoreceptor structure, or the published online only. To view Progressive cone and cone-rod dystrophies are a clinically phototransduction cascade. please visit the journal online (http:// dx. doi. org/ 10. 1136/ and genetically heterogeneous group of inherited bjophthalmol- 2018- 313278). retinal diseases characterised by cone photoreceptor PHOTORECEPTION AND THE degeneration, which may be followed by subsequent 1 PHOTOTRANSDUCTION CASCADE UCL Institute of rod photoreceptor loss. These disorders typically present Rod photoreceptors contain rhodopsin phot- Ophthalmology, University with progressive loss of central vision, colour vision College London, London, UK opigment, whereas cone photoreceptors contain 2Moorfields Eye Hospital NHS disturbance and photophobia. Considerable progress one of three types of opsin: S-cone, M-cone or Foundation Trust, London, UK has been made in elucidating the molecular genetics L-cone opsin. Disease-causing sequence variants 3 Ophthalmology Department, and genotype–phenotype correlations associated with in the genes encoding the latter two cone opsins University of California San these dystrophies, with mutations in at least 30 genes -

2015 Scheidecker Bardet Biedt
Predominantly Cone-System Dysfunction as Rare Form of Retinal Degeneration in Patients With Molecularly Confirmed Bardet-Biedl Syndrome SOPHIE SCHEIDECKER, SARAH HULL, YAUMARA PERDOMO, FOUZIA STUDER, VALE´RIE PELLETIER, JEAN MULLER, CORINNE STOETZEL, ELISE SCHAEFER, SABINE DEFOORT-DHELLEMMES, ISABELLE DRUMARE, GRAHAM E. HOLDER, CHRISTIAN P. HAMEL, ANDREW R. WEBSTER, ANTHONY T. MOORE, BERNARD PUECH, AND HE´LE`NE J. DOLLFUS PURPOSE: To describe a series of patients with Bardet- with Bardet-Biedl syndrome. (Am J Ophthalmol Biedl syndrome (BBS) and predominantly retinal cone 2015;160(2):364–372. Ó 2015 by Elsevier Inc. All dysfunction, a previously only rarely reported association. rights reserved.) DESIGN: Retrospective observational case series. METHODS: Seven patients with clinically proven Bardet-Biedl syndrome had undergone detailed ocular ARDET-BIEDL SYNDROME IS AN EMBLEMATIC CILIOP- phenotyping, which included fundus examination, Gold- athy associated with severe and early-onset retinal mann visual fields, fundus autofluorescence imaging dystrophy, postaxial polydactyly, early obesity, renal B 1 (FAF), optical coherence tomography (OCT), and elec- dysfunction, hypogonadism, and learning difficulties. It is troretinography (ERG). Mutational screening in the genetically heterogeneous, with 20 BBS genes identified BBS genes was performed either by direct Sanger (BBS1 to BBS20)todate,2,3 all of which encode proteins sequencing or targeted next-generation sequencing. involved in the development and the maintenance of the RESULTS: All 7 patients had proven BBS mutations; 1 primary cilium. had a cone dystrophy phenotype on ERG and 6 had a The retinal dystrophy associated with Bardet-Biedl syn- cone-rod pattern of dysfunction. Macular atrophy was drome is usually severe but expression can be variable. -

Case Report Sarah Burgett, OD Primary Care/Low Vision Resident Marion VAMC Marion, IL
Case Report Sarah Burgett, OD Primary Care/Low Vision Resident Marion VAMC Marion, IL Abstract A 52 year-old African American male has experienced a gradual decrease in visual acuity from 2008 to present. Ocular exams are unremarkable aside from the decrease in visual acuity. Grossly abnormal ERG results confirm progressive cone-rod dystrophy. I. Case History -Patient demographics: 52 year-old African American male -Chief complaint: Vision continues to slowly decline OU. Patient reports increased difficulty reading the Bible and other small print. -Ocular history: Myasthenia gravis x 25 years s/p thymectomy 1985. binding antibody (+), blocking/modulating antibody (-). Presented with ocular symptoms, but has become systemic. Mestinon was tried for his ocular symptoms, but it didn’t help. The patient has been on prednisone since. Doing well on prednisone 10mg QOD x many years. Diplopia/ptosis well controlled at this point. Further tapering (below 5mg/day or 10mg QOD) has been unsuccessful. Patient is follow by Neurology at Marion VA. -Medical history: Hypertension, elevated cholesterol, and pulmonary problems -Medications: 1) Colestipol HCl 1GM TAB to lower cholesterol 2) Diltiazem 180MG SA CAP for heart and blood pressure 3) Fenofibrate 145MG TAB to lower cholesterol and triglycerides 4) Hydrochlorothiazide 25MG TAB for fluid and blood pressure 5) Hydrocodone 5/Acetaminophen 500MG TAB PRN for pain 6) Lisinopril 20MG TAB to lower blood pressure 7) Prednisone 10MG TAB for myasthenia gravis - Allergies: Niacin, Zocor, Pravastatin, Crestor, Zetia 10MG TAB, Lopid 600MG TAB II. Pertinent findings -Clinical: Progressively declining BCVA OU 08/2003 20/20 OD, 20/20 OS 11/2008 20/20 OD, 20/20 OS 04/2009 20/25 OD, 20/30 NIPH OS 06/2010 20/40 OD, 20/50 OS 09/2010 20/30 OD, 20/50-2 12/2010 20/30 OD, 20/60-2 Entrance testing, slit lamp, intraocular pressure, dilated fundus examination all within normal limits OU; no ocular manifestations of myasthenia gravis. -

The Primate Model for Understanding and Restoring Vision
The primate model for understanding and restoring vision Serge Picauda,1, Deniz Dalkaraa,1, Katia Marazovaa, Olivier Goureaua, Botond Roskab,c,d,2, and José-Alain Sahela,e,f,g,2 aInstitut de la Vision, INSERM, CNRS, Sorbonne Université, F-75012 Paris, France; bInstitute of Molecular and Clinical Ophthalmology Basel, CH-4031 Basel, Switzerland; cFaculty of Medicine, University of Basel, 4056 Basel, Switzerland; dFriedrich Miescher Institute, 4058 Basel, Switzerland; eDepartment of Ophthalmology, The University of Pittsburgh School of Medicine, Pittsburgh, PA 15213; fINSERM-Centre d’Investigation Clinique 1423, Centre Hospitalier National d’Ophtalmologie des Quinze-Vingts, F-75012 Paris, France; and gDépartement d’Ophtalmologie, Fondation Ophtalmologique Rothschild, F-75019 Paris, France Edited by Tony Movshon, New York University, New York, NY, and approved October 18, 2019 (received for review July 8, 2019) Retinal degenerative diseases caused by photoreceptor cell death provide highly responsive and reliable models for in-depth are major causes of irreversible vision loss. As only primates have a functional studies. Furthermore, brain-imaging studies de- macula, the nonhuman primate (NHP) models have a crucial role scribing visual cortex activity aid our understanding of the vi- not only in revealing biological mechanisms underlying high-acuity sual system and its functions and also serve as important tools vision but also in the development of therapies. Successful trans- for studying the brain (5–8). lation of basic research findings into clinical trials and, moreover, approval of the first therapies for blinding inherited and age- Uniqueness of the Primate Model for Human Vision related retinal dystrophies has been reported in recent years.