OITE Foot and Ankle Review Anatomy and Biomechanics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chief Complaint
Chief Complaint Please choose the primary reason you are coming to our office. Complaints are listed alphabetically. Please do not select more than 5 complaints. Upper Back: Thigh/Hip: Calf: o Asthma o Arterial insufficiency o Left calf pain o Bronchitis o Left hip pain o Left leg cramps o Emphysema o Left hip tendonitis o Left leg numbness o Left Flank Pain o Left leg cramps o Left leg pain o Midback pain o Left leg numbness o Left leg weakness o Left leg pain o Leg cramps Lower Back: o Left leg weakness o Leg numbness o Fatigue o Left post. thigh pain o Leg weakness o Left flank pain o Left thigh pain o Varicose veins o Low back pain o Sciatica o Venous insufficiency o Low back spasm o Venous insufficiency o Arterial insufficiency o Lumbar arthritis o Right hip pain o Right calf pain o Menstrual cramps o Right hip tendonitis Right leg o Right leg cramps o Nervousness cramps o Right leg numbness o Pain during BM o Right leg numbness o Right leg pain o Right flank pain o Right leg pain o Right leg weakness o Sacroiliac pain o Right leg weakness o Sciatica o Right post. thigh pain Neck: o Stiffness o Right thigh pain o Bronchitis o Whole body pain o Clavicular pain Head: Buttocks: o Cold o Agitation o Bleeding during BM o Coughing o Anxiety attack o Bursitis of hip o Dysphagia o Cold o Gluteal pain o Goiter o Diminished concentration o Hemorrhoids o Hoarseness o Dizziness o Left gluteal pain o Neck pain o Dysphagia o Left hip pain o Neck spasm o Ear pain o Left post. -

Skeletal Foot Structure
Foot Skeletal Structure The disarticulated bones of the left foot, from above (The talus and calcaneus remain articulated) 1 Calcaneus 2 Talus 3 Navicular 4 Medial cuneiform 5 Intermediate cuneiform 6 Lateral cuneiform 7 Cuboid 8 First metatarsal 9 Second metatarsal 10 Third metatarsal 11 Fourth metatarsal 12 Fifth metatarsal 13 Proximal phalanx of great toe 14 Distal phalanx of great toe 15 Proximal phalanx of second toe 16 Middle phalanx of second toe 17 Distal phalanx of second toe Bones of the tarsus, the back part of the foot Talus Calcaneus Navicular bone Cuboid bone Medial, intermediate and lateral cuneiform bones Bones of the metatarsus, the forepart of the foot First to fifth metatarsal bones (numbered from the medial side) Bones of the toes or digits Phalanges -- a proximal and a distal phalanx for the great toe; proximal, middle and distal phalanges for the second to fifth toes Sesamoid bones Two always present in the tendons of flexor hallucis brevis Origin and meaning of some terms associated with the foot Tibia: Latin for a flute or pipe; the shin bone has a fanciful resemblance to this wind instrument. Fibula: Latin for a pin or skewer; the long thin bone of the leg. Adjective fibular or peroneal, which is from the Greek for pin. Tarsus: Greek for a wicker frame; the basic framework for the back of the foot. Metatarsus: Greek for beyond the tarsus; the forepart of the foot. Talus (astragalus): Latin (Greek) for one of a set of dice; viewed from above the main part of the talus has a rather square appearance. -

Total HIP Replacement Exercise Program 1. Ankle Pumps 2. Quad
3 sets of 10 reps (30 ea) 2 times a day Total HIP Replacement Exercise Program 5. Heel slides 1. Ankle Pumps Bend knee and pull heel toward buttocks. DO NOT GO Gently point toes up towards your nose and down PAST 90* HIP FLEXION towards the surface. Do both ankles at the same time or alternating feet. Perform slowly. 2. Quad Sets Slowly tighten thigh muscles of legs, pushing knees down into the surface. Hold for 10 count. 6. Short Arc Quads Place a large can or rolled towel (about 8”diameter) under the leg. Straighten knee and leg. Hold straight for 5 count. 3. Gluteal Sets Squeeze the buttocks together as tightly as possible. Hold for a 10 count. 7. Knee extension - Long Arc Quads Slowly straighten operated leg and try to hold it for 5 sec. Bend knee, taking foot under the chair. 4. Abduction and Adduction Slide leg out to the side. Keep kneecap pointing toward ceiling. Gently bring leg back to pillow. May do both legs at the same time. Copywriter VHI Corp 3 sets of 10 reps (30 ea) 2 times a day Total HIP Replacement Exercise Program 8. Standing Stair/Step Training: Heel/Toe Raises: 1. The “good” (non-operated) leg goes Holding on to an immovable surface. UP first. Rise up on toes slowly 2. The “bad” (operated) leg goes for a 5 count. Come back to foot flat and lift DOWN first. toes from floor. 3. The cane stays on the level of the operated leg. Resting positions: To Stretch your hip to neutral position: 1. -
Evaluation of the Inferior Calcaneal Spurs Influence on Plantar Fascia
Evaluation of the Inferior Calcaneal Spurs Influence on Plantar Fascia Thickness Clint Jiroux, PMS-II ; Kyle Schwickerath, PMS-II; Frank Felix, PMS-II; Chad Smith, PMS-II; Matt Greenblatt, PMS-II Arizona School of Podiatric Medicine – Midwestern University Printing: This poster is 48” wide by 36” high. It’s STATEMENT OF PURPOSE ANALYSIS & DISCUSSION designed to be printed on a large • Plantar fasciitis is a common pathology associated with plantar heel pain. It is Through ultrasound, our research revealed the spur does not show a reported that in the United States, two million patients are treated for plantar relationship to the thickness of the plantar fascia. Thus, based on our data, printer. fasciitis annually, and accounts for 15% of all foot disorders (1). A frequent diagnostic measurements of the fascia band thickness should not take into association with plantar fasciitis is the presence of an inferior calcaneal heel consideration the presence of a heel spur. This data is supportive to the spur. Often debated by medical professionals; Is the heel spur an incidental or consensus of 4mm being the diagnostic value for plantar fasciitis. Additionally, causation of plantar fasciitis (2-4)? Using ultrasound imaging, the plantar fascia this strengthens support of the heel spur being an incidental finding with plantar Figure 1. Type A inferior calcaneal spur that extends above the plantar fascia. (A) Type B inferior calcaneal Figure 2. Longitudinal ultrasound of the plantar fascia with the presence of an inferior calcaneal spur. (A) A fasciitis. thickness can be quantifiably measured to determine plantar fasciitis. An spur that extends into the plantar fascia. -

Human Functional Anatomy 213 the Ankle and Foot In
2 HUMAN FUNCTIONAL ANATOMY 213 JOINTS OF THE FOOT THE ANKLE AND FOOT IN LOCOMOTION THE HINDFOOT -(JOINTS OF THE TALUS) THIS WEEKS LAB: Forearm and hand TROCHLEAR The ankle, and distal tibiofibular joints READINGS BODY The leg and sole of foot Subtalar joint (Posterior talocalcaneal) 1. Stern – Core concepts – sections 99, 100 and 101 (plus appendices) HEAD 2. Faiz and Moffat – Anatomy at a Glance – Sections 50 and 51 Talocalcaneonavicular 3. Grants Method:- The bones and sole of foot & Joints of the lower limb & Transverse tarsal joints or any other regional textbook - similar sections IN THIS LECTURE I WILL COVER: Joints related to the talus Ankle Subtalar Talocalcaneonavicular THE MID FOOT Transverse tarsal Other tarsal joints THE FOREFOOT Toe joints METATARSAL AND PHALANGEAL Ligaments of the foot JOINTS (same as in the hand) Arches of the foot Except 1st metatarsal and Hallux Movements of the foot & Compartments of the leg No saddle joint at base is 1st metatarsal The ankle in Locomotion Metatarsal head is bound by deep Ankle limps transverse metatarsal ligament 1. Flexor limp Toes are like fingers 2. Extensor limp Same joints, Lumbricals, Interossei, Extensor expansion Axis of foot (for abduction-adduction) is the 2nd toe. 3 4 JOINTS OF THE FOOT JOINTS OF THE FOOT (2 joints that allow inversion and eversion) DISTAL TIBIOFIBULAR SUBTALAR (Posterior talocalcaneal) JOINT Syndesmosis (fibrous joint like interosseous membrane) Two (or three) talocalcaneal joints Posterior is subtalar Fibres arranged to allow a little movement Anterior (and middle) is part of the talocalcaneonavicular. With a strong interosseus ligament running between them (tarsal sinus) THE TALOCALCANEONAVICULAR JOINT The head of the talus fits into a socket formed from the: The anterior talocalcaneal facets. -
Arthroscopic and Open Anatomy of the Hip 11
CHAPTER Arthroscopic and o'pen Anatomy of the Hip Michael B. Gerhardt, Kartik Logishetty, Morteza lV1eftah, and Anil S. Ranawat INTRODUCTION movements that they induce at the joint: 1) flexors; 2) extensors; 3) abductors; 4) adductors; 5) external rotators; and 6) interI12 I The hip joint is defined by the articulation between the head rotators. Although some muscles have dual roles, their primary of the femur and the aeetahulum of the pelvis. It is covered by functions define their group placem(:)nt, and they all have ullique :l large soft-tissue envelope and a complex array of neurovascu- neurovascular supplies (TIt ble 2-1). lar and musculotendinous structures. The joint's morphology The vascular supply of tbe hip stems from the external and anu orientation are complex, and there are wide anatomi c varia- internal iLiac ancries. An understanding of the course of these tions seen among individuals. The joint's deep location makes vessels is critical fo r ,lVo iding catasu"ophic vascular injury. fn both arthroscopic and open access challenging. To avoid iatro- addition, the blood supply to the fel11()ra l head is vulnerahle to genic injury while establishing functional and efficient access, both traumatic and iatrogenic injury; the disruption of this sup- the hip surgeon should possess a sound ana tomic knowledge of ply can result in avascular necrosis (Figure 2-2). the hip. T he human "hip" can be subdivided into three categories: I) the superficial surface anatomy; 2) the deep femoroacetabu- la r Joint and capsule; and 3) the associated structures, including the muscles, nerves, and vasculature, all of which directly affeet HIP MUSCULATURE its function. -
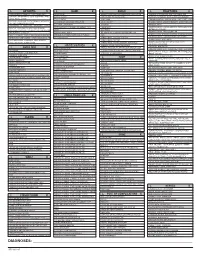
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Bioarchaeological Implications of Calcaneal Spurs in the Medieval Nubian Population of Kulubnarti
Bioarchaeological Implications of Calcaneal Spurs in the Medieval Nubian Population of Kulubnarti Lindsay Marker Department of Anthropology Primary Thesis Advisor Matthew Sponheimer, Department of Anthropology Defense Committee Members Douglas Bamforth, Department of Anthropology Patricia Sullivan, Department of English University of Colorado at Boulder April 2016 1 Table of Contents List of Figures ............................................................................................................................. 4 Abstract …................................................................................................................................... 6 Chapter 1: Introduction …........................................................................................................... 8 Chapter 2: Anatomy …................................................................................................................ 11 2.1 Chapter Overview …................................................................................................. 11 2.2 Bone Composition …................................................................................................ 11 2.3 Plantar Foot Anatomy …........................................................................................... 12 2.4 Posterior Foot Anatomy …........................................................................................ 15 Chapter 3: Literature Review and Background of Calcaneal Enthesophytes ............................. 18 3.1 Chapter Overview …................................................................................................ -

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

ICD-9CM Coding Achilles Bursitis Or Tendinitis 726.71 Adhesive
ICD-9CM CODING OF COMMON CHIROPRACTIC CONDITIONS CONDITION ICD-9CM coding Achilles bursitis or tendinitis 726.71 Adhesive capsulitis of shoulder 726 Anklyosing Spondylitis (spine only) 720 Anterior cruciate ligament (old disruption) 717.83 Bicipital tenosynovitis 726.12 Boutonniere deformity 736.21 Brachial neuritis or radiculitis 723.4 Bunion 727.1 Bursitis of knee 726.6 Calcaneal spur 726.73 Carpal tunnel syndrome 354 Cervical radiculitis 723.4 Cervical spondylosis with myelopathy 721.1 Cervical spondylosis without myelopathy 721 Cervicalgia 723.1 Chondromalacia of patella 717.7 Claw hand (acquired) 736.06 Claw toe (acquired) 735.5 Coccygodynia 724.79 Coxa plana 732.1 Coxa valga (acquired) 736.31 Coxa vara (acquired) 736.32 de Quervain's disease 727.04 Degeneration of cervical intervertebral disc 722.4 Degeneration of thoracic or lumbar intervertebral disc 722.5 Disc Degeneration (Cervical with myelopathy) 722.71 Disc Degeneration (Lumbar with myelopathy) 722.73 Disc Degeneration (Thoracic) 722.51 Disc Degeneration (Cervical) 722.4 Disc Degeneration (Lumbar) 722.52 Disc Degeneration (Thoracic with myelopathy) 722.72 Disc displacement without myelopathy (Thoracic) 722.11 Disc displacement of without myelopathy (Cervical ) 722 Disc displacement without myelopathy (Lumbar) 722.1 Dupuytren's contracture 728.6 Entrapment syndromes 354.0-355.9 Epicondylitis (Lateral) 726.32 Epicondylitis (Medial) 726.31 Flat foot-Pes planus (acquired) 734 Fracture (Lumbar) 805.4 Ganglion of tendon sheath 727.42 Genu recurvatum (acquired) 736.5 Genu valgum -

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -

A Case Report on Charcot-Marie-Tooth Disease with a Novel Periaxin Gene Mutation
Open Access Case Report DOI: 10.7759/cureus.5111 A Case Report on Charcot-Marie-Tooth Disease with a Novel Periaxin Gene Mutation Sorabh Datta 1 , Saurabh Kataria 1 , Raghav Govindarajan 1 1. Neurology, University of Missouri, Columbia, USA Corresponding author: Sorabh Datta, [email protected] Abstract Charcot-Marie-Tooth (CMT) disease is one of the most common primary hereditary neuropathies causing peripheral neuropathies. More than 60 different gene mutations are causing this disease. The PRX gene codes for Periaxin proteins that are expressed by Schwann cells and are necessary for the formation and maintenance of myelination of peripheral nerves. Dejerine-Sottas neuropathy and Charcot-Marie-Tooth type 4F (CMT4F) are the two different clinical phenotypes observed in association with PRX gene mutation. This article describes a case of an elderly male with a novel mutation involving the PRX gene. Categories: Genetics, Internal Medicine, Neurology Keywords: neurology, sensorimotor neuropathy, congenital, gene expression, genetic mutation, protein, pes cavus, demyelinating diseases, charcot-marie-tooth, autosomal recessive disorder Introduction As per the Dyck classification in the year 1970, primary hereditary neuropathies are divided into hereditary motor sensory neuropathy (HMSN) and hereditary sensory autonomic neuropathy (HSAN) [1]. Charcot- Marie-Tooth (CMT) disease is a type of HMSN with an estimated prevalence of 1 in 2,500 [2]. CMT can follow autosomal recessive (ARCMT), X-linked recessive, and also an autosomal dominant pattern. CMT type 4 is a rapidly increasing ARCMT disease form in HMSN, although CMT type 1 and 2 still account for the most substantial proportion of the patient population [3]. CMT4F is a severe, demyelinating subtype of CMT type 4 and is characterized by childhood onset of slowly progressing weakness in the distal muscles associated with atrophy.