ICD-9 to ICD-10 Mapping Tool Courtesy Of: the Paperwork Project
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
18-0969: R.S. and DEPARTMENT of the ARMY, WALTER
United States Department of Labor Employees’ Compensation Appeals Board __________________________________________ ) R.S., Appellant ) ) and ) Docket No. 18-0969 ) Issued: March 27, 2019 DEPARTMENT OF THE ARMY, WALTER ) REED NATIONAL MILITARY MEDICAL ) CENTER, Bethesda, MD, Employer ) _________________________________________ ) Appearances: Case Submitted on the Record Appellant, pro se Office of Solicitor, for the Director DECISION AND ORDER Before: CHRISTOPHER J. GODFREY, Chief Judge PATRICIA H. FITZGERALD, Deputy Chief Judge VALERIE D. EVANS-HARRELL, Alternate Judge JURISDICTION On April 10, 2018 appellant filed a timely appeal from a December 22, 2017 merit decision of the Office of Workers’ Compensation Programs (OWCP). Pursuant to the Federal Employees’ Compensation Act1 (FECA) and 20 C.F.R. §§ 501.2(c) and 501.3, the Board has jurisdiction over the merits of this case.2 ISSUE The issue is whether appellant has met her burden of proof to establish lumbar and/or right shoulder conditions causally related to an April 7, 2016 employment incident. 1 5 U.S.C. § 8101 et seq. 2 The Board notes that following the December 22, 2017 decision, OWCP received additional evidence. However, the Board’s Rules of Procedure provides: “The Board’s review of a case is limited to the evidence in the case record that was before OWCP at the time of its final decision. Evidence not before OWCP will not be considered by the Board for the first time on appeal.” 20 C.F.R. § 501.2(c)(1). Thus, the Board is precluded from reviewing this additional evidence for the first time on appeal. Id. FACTUAL HISTORY On April 15, 2016 appellant, then a 64-year-old radiology technology supervisor, filed a traumatic injury claim (Form CA-1) alleging that on April 7, 2016 she injured her lower back and right shoulder while in the performance of duty. -

Tuberculous Spondylitis, Pyogenic Spondylitis, X-Ray and Tomographic Features
American Journal of Medicine and Medical Sciences 2021, 11(5): 398-401 DOI: 10.5923/j.ajmms.20211105.08 X-Ray and Tomographic Manifestations of Tuberculous Spondylitis Babоev Abduvakhob Sakhibnazarovich Bone and Joint Tuberculosis Department of Rebuplican Specialized Scientific Practical Medical Center of Phtiziology and Pulmonology, Tashkent, Uzbekistan Abstract X-ray and tomographic data of seventy-eight patients with spine disorders (31 patients with tuberculous spondylitis, 23 patients with pyogenic spondylitis, and 24 patients with degenerative spondylopathy) after clinical, laboratory, bacteriologic, and histologic verification of diagnosis was comparatively analyzed. Current X-ray and tomographic features of tuberculous spondylitis are relatively equal thoracic and lumbosacral spine segments localization, with more than two adjacent vertebrae involvement in 22,6±7,5% of cases, the collapse of the vertebra(s) in 35.5 ± 8.6% of cases, unclear or osteoporotic border of bone tissue around TB focus in 64.5 ± 8.6%, formation of abscesses in 74.2±7.9% and their subligamentous spread to more than two vertebrae in 25,8±7,9% of cases, intact intervertebral disc in 16.1 ± 6.6% of cases, and specific process in the lungs in 48.4 ± 9.0% of cases. Keywords Tuberculous spondylitis, Pyogenic spondylitis, X-ray and tomographic features identify differential diagnostic features of tuberculous 1. Introduction spondylitis (TS). X-ray and tomographic (MRI and CT) methods of examination play a leading role in the diagnosis of 3. Materials and Methods tuberculous (TB) lesions of the spine [1,2,3]. Features of radiological changes of spine TB depend on The study was conducted at the bone and joint TB the activity and duration of the specific process [1,2]. -

ICD-9CM Coding Achilles Bursitis Or Tendinitis 726.71 Adhesive
ICD-9CM CODING OF COMMON CHIROPRACTIC CONDITIONS CONDITION ICD-9CM coding Achilles bursitis or tendinitis 726.71 Adhesive capsulitis of shoulder 726 Anklyosing Spondylitis (spine only) 720 Anterior cruciate ligament (old disruption) 717.83 Bicipital tenosynovitis 726.12 Boutonniere deformity 736.21 Brachial neuritis or radiculitis 723.4 Bunion 727.1 Bursitis of knee 726.6 Calcaneal spur 726.73 Carpal tunnel syndrome 354 Cervical radiculitis 723.4 Cervical spondylosis with myelopathy 721.1 Cervical spondylosis without myelopathy 721 Cervicalgia 723.1 Chondromalacia of patella 717.7 Claw hand (acquired) 736.06 Claw toe (acquired) 735.5 Coccygodynia 724.79 Coxa plana 732.1 Coxa valga (acquired) 736.31 Coxa vara (acquired) 736.32 de Quervain's disease 727.04 Degeneration of cervical intervertebral disc 722.4 Degeneration of thoracic or lumbar intervertebral disc 722.5 Disc Degeneration (Cervical with myelopathy) 722.71 Disc Degeneration (Lumbar with myelopathy) 722.73 Disc Degeneration (Thoracic) 722.51 Disc Degeneration (Cervical) 722.4 Disc Degeneration (Lumbar) 722.52 Disc Degeneration (Thoracic with myelopathy) 722.72 Disc displacement without myelopathy (Thoracic) 722.11 Disc displacement of without myelopathy (Cervical ) 722 Disc displacement without myelopathy (Lumbar) 722.1 Dupuytren's contracture 728.6 Entrapment syndromes 354.0-355.9 Epicondylitis (Lateral) 726.32 Epicondylitis (Medial) 726.31 Flat foot-Pes planus (acquired) 734 Fracture (Lumbar) 805.4 Ganglion of tendon sheath 727.42 Genu recurvatum (acquired) 736.5 Genu valgum -

A Case Report on Charcot-Marie-Tooth Disease with a Novel Periaxin Gene Mutation
Open Access Case Report DOI: 10.7759/cureus.5111 A Case Report on Charcot-Marie-Tooth Disease with a Novel Periaxin Gene Mutation Sorabh Datta 1 , Saurabh Kataria 1 , Raghav Govindarajan 1 1. Neurology, University of Missouri, Columbia, USA Corresponding author: Sorabh Datta, [email protected] Abstract Charcot-Marie-Tooth (CMT) disease is one of the most common primary hereditary neuropathies causing peripheral neuropathies. More than 60 different gene mutations are causing this disease. The PRX gene codes for Periaxin proteins that are expressed by Schwann cells and are necessary for the formation and maintenance of myelination of peripheral nerves. Dejerine-Sottas neuropathy and Charcot-Marie-Tooth type 4F (CMT4F) are the two different clinical phenotypes observed in association with PRX gene mutation. This article describes a case of an elderly male with a novel mutation involving the PRX gene. Categories: Genetics, Internal Medicine, Neurology Keywords: neurology, sensorimotor neuropathy, congenital, gene expression, genetic mutation, protein, pes cavus, demyelinating diseases, charcot-marie-tooth, autosomal recessive disorder Introduction As per the Dyck classification in the year 1970, primary hereditary neuropathies are divided into hereditary motor sensory neuropathy (HMSN) and hereditary sensory autonomic neuropathy (HSAN) [1]. Charcot- Marie-Tooth (CMT) disease is a type of HMSN with an estimated prevalence of 1 in 2,500 [2]. CMT can follow autosomal recessive (ARCMT), X-linked recessive, and also an autosomal dominant pattern. CMT type 4 is a rapidly increasing ARCMT disease form in HMSN, although CMT type 1 and 2 still account for the most substantial proportion of the patient population [3]. CMT4F is a severe, demyelinating subtype of CMT type 4 and is characterized by childhood onset of slowly progressing weakness in the distal muscles associated with atrophy. -

Neurological Impairment in a Patient with Concurrent Cervical Disc Herniation and POEMS Syndrome
European Spine Journal (2019) 28 (Suppl 2):S51–S55 https://doi.org/10.1007/s00586-019-05914-5 CASE REPORT Neurological impairment in a patient with concurrent cervical disc herniation and POEMS syndrome Tingxian Ling1 · Limin Liu1 · Yueming Song1 · Shilian Zhou1 · Chunguang Zhou1 Received: 24 July 2018 / Revised: 16 December 2018 / Accepted: 9 February 2019 / Published online: 13 February 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose POEMS syndrome is a rare clonal plasma cell disease characterized by polyneuropathy, organomegaly, endocrinopa- thy, M protein, and skin changes. We report a rare case of neurological impairment in patients with concurrent cervical disc herniation and POEMS syndrome. Methods A patient presented to a local hospital with C3/4 and C4/5 disc herniation, apparent spinal cord compression con- comitant with neurological signs, and concurrent POEMS syndrome. Anterior cervical discectomy and fusion was performed. Results The limb numbness was only slightly alleviated, and 10 days postoperatively the patient complained of muscle weak- ness of the extremities and was referred to our hospital. The patients exhibited non-typical neurological signs and an enlarged liver and spleen that could not be explained. Electroneuromyography and immunofxation electrophoresis produced abnormal results. We diagnosed concurrent POEMS syndrome, for which drug therapy was prescribed. The patient’s symptoms receded. Conclusion Patients presenting with cervical spondylopathy and non-typical neurological signs and symptoms or other systemic problems should be evaluated for the presence of concurrent disease and ruled out diferential diagnoses. Keywords Neurological impairment · POMES syndrome · Cervical disc herniation · Cervical spondylosis Introduction a chronic demyelinating autoimmune disease that has symp- toms similar to those associated with myelopathy: spasticity, Cervical disc herniation is a common spinal disorder that sensory disturbances, gait ataxia, weakness. -

The Nutrition and Food Web Archive Medical Terminology Book
The Nutrition and Food Web Archive Medical Terminology Book www.nafwa. -

IN the UNITED STATES COURT of FEDERAL CLAIMS OFFICE of SPECIAL MASTERS No
IN THE UNITED STATES COURT OF FEDERAL CLAIMS OFFICE OF SPECIAL MASTERS No. 10-565V Filed: June 11, 2014 For Publication * * * * * * * * * * * * * * * * * * * * * * * * * * * * MEGAN L. GODFREY, * HPV Vaccine; Gardasil; Juvenile * Ankylosing Spondylitis; JAS; Petitioner, * Causation-in-Fact; Expert; v. * Qualifications. * SECRETARY OF HEALTH * AND HUMAN SERVICES, * * Respondent. * * * * * * * * * * * * * * * * * * * * * * * * * * * * * Milton Clay Ragsdale, IV, Ragsdale LLC, Birmingham, AL, for petitioner. Jennifer Reynaud, U.S. Department of Justice, Washington, DC, for respondent. DECISION1 Vowell, Chief Special Master: On August 20, 2010, Megan Godfrey [“petitioner”] filed a petition for compensation under the National Vaccine Injury Compensation Program, 42 U.S.C. §300aa-10, et seq.2 [the “Vaccine Act” or “Program”]. The petition alleged that the human papillomavirus [“HPV”] and meningococcal conjugate vaccines Ms. Godfrey received on August 22, 2007, caused her to develop juvenile rheumatoid arthritis. Petition at 1-2. 1 Because this decision contains a reasoned explanation for my action in this case, it will be posted on the United States Court of Federal Claims’ website, in accordance with the E-Government Act of 2002, Pub. L. No. 107-347, 116 Stat. 2899, 2913 (Dec. 17, 2002). As provided by Vaccine Rule 18(b), each party has 14 days within which to request redaction “of any information furnished by that party: (1) that is a trade secret or commercial or financial in substance and is privileged or confidential; or (2) that includes medical files or similar files, the disclosure of which would constitute a clearly unwarranted invasion of privacy.” Vaccine Rule 18(b). Otherwise, the entire decision will be available to the public. 2 National Childhood Vaccine Injury Act of 1986, Pub. -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 26, NUMBER 4 - FALL 2014 Fig. 1. Knee Inside... anatomy and • Rotator Cuff Disease ACL injury. Extended (straight) knee • Bunions and Lesser Toe Deformities Femur • Tendon Injuries of the Hand (thighbone) Patella In Perspective: (kneecap) Anterior Cruciate Ligament Tears Medial In 1992, Dr. Jack C. Hughston (1917-2004), one of the meniscus world’s most respected authorities on knee ligament surgery, MCL LCL shared some of his thoughts regarding injuries to the ACL. (medial “You tore your anterior cruciate ligament.” On hearing (lateral collateral collateral your physician speak those words, you are filled with a sense ligament) of dread. You envision the end of your athletic life, even ligament) recreational sports. Today, a torn ACL (Fig. 1) has almost become a household Tibia word. Through friends, newspapers, television, sports Fibula (shinbone) magazines, and even our physicians, we are inundated with the hype that the knee joint will deteriorate and become arthritic if the ACL is not operated on as soon as possible. You have been convinced that to save your knee you must Flexed (bent) knee have an operation immediately to repair the ligament. Your surgery is scheduled for the following day. You are scared. Patella But there is an old truism in orthopaedic surgery that says, (kneecap) “no knee is so bad that it can’t be made worse by operating Articular Torn ACL on it.” cartilage (anterior For many years, torn ACLs were treated as an emergency PCL cruciate and were operated on immediately, even before the initial (posterior ligament) pain and swelling of the injury subsided. -

Hammer Toe Information Sheet
Fitter Feet For Life Hammer toe information sheet. (ref. A15) A hammer toe is a deformity of the first small toe joint with in toes. (proximal inter-phalangeal joint) This deformity can occur in the second, third, fourth or fifth (relatively rare) toes, causing it to be permanently bent, resembling a hammer. This abnormality can create pressure on the foot when wearing shoes and cause discomfort and problems walking. The joints themselves can be arthritic and painful. There is a choice of different procedures to straighten a hammer toe. This information sheet has been written to help you choose which procedure is best for you. Fig 1 Hammer toe . Fig 2 Arthrodesis with K wires . Fig 3. Smart toe implant An arthrodesis is a surgical procedure to treat hammer toes. The deformed joint is fully removed and the apposing bone ends fused together in a corrected position. The joint will no longer move. The joint closer to the end of the toe will still move. The joint where the toe joins the foot will also continue to move. 1 Fitter Feet For life. 34 North Street. London SW40HD 0207 627 4901 Fitter Feet For Life 1. K-Wire Arthrodesis. Traditionally hammer toe correction is performed by arthrodesis surgery using K-Wires. The procedure is successful in most cases and has been performed for many years. The deformed joint is removed and the bone ends are secured together with a K-wire which protrudes though the tip of the toe. The foot must be kept dry, dressed and the k-wire protected in a post operative shoe for six weeks after the operation. -

Doctoral Thesis Effectiveness of Tumor Necrosis Factor Inhibitors in Patients
Bente Glintborg 2018 Glintborg Bente UNIVERSITY OF COPENHAGEN FACULTY OF HEALTH AND MEDICAL SCIENCES Effectiveness of Effectiveness Doctoral thesis Doctoral thesis Bente Glintborg, 2018 Bente Glintborg, 2018 tumor Effectiveness of tumor necrosis factor inhibitors in patients necrosis factor inhibitors in patients with psoriatic arthritis and arthritiswithaxial psoriatic inhibitorsin patients factor necrosis with psoriatic arthritis and axial spondyloarthritis – treatment response, drug retention and predictors thereof Results from the nationwide DANBIO registry Copenhagen Center for Arthritis Research (COPECARE) Center for Rheumatology and Spine Diseases Centre of Head and Orthopaedics Rigshospitalet, Glostrup spondyloarthritis ISBN 978-87-970989-0-5 Doctoral thesis Effectiveness of tumor necrosis factor inhibitors in patients with psoriatic arthritis and axial spondyloarthritis – treatment response, drug retention and predictors thereof Results from the nationwide DANBIO registry Bente Glintborg, MD, PhD 2018 The DANBIO registry and Copenhagen Center for Arthritis Research, COPECARE Center for Rheumatology and Spine Diseases Centre of Head and Orthopedics Rigshospitalet 1 © Bente Glintborg 2018 ISBN 978-87-970989-0-5 All rights reserved. No parts of this publication may be reproduced or transmitted, in any form or by any means, without permission The Faculty of Health and Medical Sciences at the University of Copenhagen has accepted this dissertation, which consists of the already published dissertations listed below, for public defence -

Low Back Pain: a Pathway to Prioritisation
National Health Committee – Low Back Pain: A Pathway to Prioritisation National Health Committee Low Back Pain: A Pathway to Prioritisation Page 1 National Health Committee – Low Back Pain: A Pathway to Prioritisation National Health Committee (NHC) The National Health Committee (NHC) is an independent statutory body charged with prioritising new and existing health technologies and making recommendations to the Minister of Health. It was reformed in 2011 to establish evaluation systems that would provide the New Zealand people and the health sector with greater value for money invested in health. The NHC Executive is the secretariat that supports the Committee. The NHC Executive’s primary objective is to provide the Committee with sufficient information for it to make decisions regarding prioritisation and reprioritisation of interventions and services. They do this through a range of evidence-based products chosen according to the nature of the decision required and timeframe within which decisions need to be made. The New Zealand Government has asked that all new diagnostic and treatment (non-pharmaceutical) services, and significant expansions of existing services, are to be referred to the NHC. In August 2011 the NHC was appointed with new Terms of Reference and a mandate to establish the capacity to assess new and existing health technologies. Its objectives (under Section 4.2 of its Terms of Reference – www.nhc.health.govt.nz) include contributing to improved value for money and fiscal sustainability in the health and disability sector by: providing timely advice and recommendations about relative cost-effectiveness based on the best available evidence; providing advice and recommendations which influence the behaviour of decision makers including clinicians and other health professionals; providing advice and recommendations which are reflected in resource allocation at national, regional and local levels; and contributing to tangible reductions in the use of ineffective interventions and improved targeting to those most likely to benefit. -
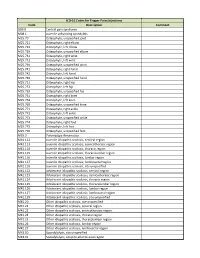
ICD-10 Codes for Trigger Point Injections
ICD-10 Codes for Trigger Point Injections Code Description Comment G89.0 Central pain syndrome M08.1 Juvenile ankylosing spondylitis M25.70 Osteophyte, unspecified joint M25.721 Osteophyte, right elbow M25.722 Osteophyte, left elbow M25.729 Osteophyte, unspecified elbow M25.731 Osteophyte, right wrist M25.732 Osteophyte, left wrist M25.739 Osteophyte, unspecified wrist M25.741 Osteophyte, right hand M25.742 Osteophyte, left hand M25.749 Osteophyte, unspecified hand M25.751 Osteophyte, right hip M25.752 Osteophyte, left hip M25.759 Osteophyte, unspecified hip M25.761 Osteophyte, right knee M25.762 Osteophyte, left knee M25.769 Osteophyte, unspecified knee M25.771 Osteophyte, right ankle M25.772 Osteophyte, left ankle M25.773 Osteophyte, unspecified ankle M25.774 Osteophyte, right foot M25.775 Osteophyte, left foot M25.776 Osteophyte, unspecified foot M35.3 Polymyalgia rheumatica M41.112 Juvenile idiopathic scoliosis, cervical region M41.113 Juvenile idiopathic scoliosis, cervicothoracic region M41.114 Juvenile idiopathic scoliosis, thoracic region M41.115 Juvenile idiopathic scoliosis, thoracolumbar region M41.116 Juvenile idiopathic scoliosis, lumbar region M41.117 Juvenile idiopathic scoliosis, lumbosacral region M41.119 Juvenile idiopathic scoliosis, site unspecified M41.122 Adolescent idiopathic scoliosis, cervical region M41.123 Adolescent idiopathic scoliosis, cervicothoracic region M41.124 Adolescent idiopathic scoliosis, thoracic region M41.125 Adolescent idiopathic scoliosis, thoracolumbar region M41.126 Adolescent idiopathic