Hereditary/Chromosomal Syndromes and Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Crouzon Syndrome Genetic and Intervention Review
Journal of Oral Biology and Craniofacial Research 9 (2019) 37–39 Contents lists available at ScienceDirect Journal of Oral Biology and Craniofacial Research journal homepage: www.elsevier.com/locate/jobcr Crouzon syndrome: Genetic and intervention review ∗ T N.M. Al-Namnama, , F. Haririb, M.K. Thongc, Z.A. Rahmanb a Department of Oral Biology, Faculty of Dentistry, University of MAHSA, 42610, Jenjarum, Selangor, Malaysia b Department of Oro-Maxillofacial Clinical Science, Faculty of Dentistry, University of Malaya, 50603, Kuala Lumpur, Malaysia c Department of Paediatrics, Faculty of Medicine, University of Malaya, 50603, Kuala Lumpur, Malaysia ARTICLE INFO ABSTRACT Keywords: Crouzon syndrome exhibits considerable phenotypic heterogeneity, in the aetiology of which genetics play an Crouzon syndrome important role. FGFR2 mediates extracellular signals into cells and the mutations in the FGFR2 gene cause this Molecular pathology syndrome occurrence. Activated FGFs/FGFR2 signaling disrupts the balance of differentiation, cell proliferation, Genetic phenotype and apoptosis via its downstream signal pathways. However, very little is known about the cellular and mole- cular factors leading to severity of this phenotype. Revealing the molecular pathology of craniosynostosis will be a great value for genetic counselling, diagnosis, prognosis and early intervention programs. This mini-review summarizes the fundamental and recent scientific literature on genetic disorder of Crouzon syndrome and presents a graduated strategy for the genetic approach, diagnosis and the management of this complex cra- niofacial defect. 1. Introduction known. CS commonly starts at the first three years of life.4 Craniosy- nostosis can be suspected during antenatal stage via ultrasound scan Craniosynostosis is a birth defect characterized by premature fusion otherwise is often detected at birth from its classic crouzonoid features of one or more of the calvarial sutures before the completion of brain of the newborn. -
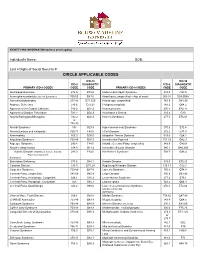
Circle Applicable Codes
IDENTIFYING INFORMATION (please print legibly) Individual’s Name: DOB: Last 4 Digits of Social Security #: CIRCLE APPLICABLE CODES ICD-10 ICD-10 ICD-9 DIAGNOSTIC ICD-9 DIAGNOSTIC PRIMARY ICD-9 CODES CODE CODE PRIMARY ICD-9 CODES CODE CODE Abetalipoproteinemia 272.5 E78.6 Hallervorden-Spatz Syndrome 333.0 G23.0 Acrocephalosyndactyly (Apert’s Syndrome) 755.55 Q87.0 Head Injury, unspecified – Age of onset: 959.01 S09.90XA Adrenaleukodystrophy 277.86 E71.529 Hemiplegia, unspecified 342.9 G81.90 Arginase Deficiency 270.6 E72.21 Holoprosencephaly 742.2 Q04.2 Agenesis of the Corpus Callosum 742.2 Q04.3 Homocystinuria 270.4 E72.11 Agenesis of Septum Pellucidum 742.2 Q04.3 Huntington’s Chorea 333.4 G10 Argyria/Pachygyria/Microgyria 742.2 Q04.3 Hurler’s Syndrome 277.5 E76.01 or 758.33 Aicardi Syndrome 333 G23.8 Hyperammonemia Syndrome 270.6 E72.4 Alcohol Embryo and Fetopathy 760.71 F84.5 I-Cell Disease 272.2 E77.0 Anencephaly 655.0 Q00.0 Idiopathic Torsion Dystonia 333.6 G24.1 Angelman Syndrome 759.89 Q93.5 Incontinentia Pigmenti 757.33 Q82.3 Asperger Syndrome 299.8 F84.5 Infantile Cerebral Palsy, unspecified 343.9 G80.9 Ataxia-Telangiectasia 334.8 G11.3 Intractable Seizure Disorder 345.1 G40.309 Autistic Disorder (Childhood Autism, Infantile 299.0 F84.0 Klinefelter’s Syndrome 758.7 Q98.4 Psychosis, Kanner’s Syndrome) Biotinidase Deficiency 277.6 D84.1 Krabbe Disease 333.0 E75.23 Canavan Disease 330.0 E75.29 Kugelberg-Welander Disease 335.11 G12.1 Carpenter Syndrome 759.89 Q87.0 Larsen’s Syndrome 755.8 Q74.8 Cerebral Palsy, unspecified 343.69 G80.9 -

2018 Etiologies by Frequencies
2018 Etiologies in Order of Frequency by Category Hereditary Syndromes and Disorders Count CHARGE Syndrome 958 Down syndrome (Trisomy 21 syndrome) 308 Usher I syndrome 252 Stickler syndrome 130 Dandy Walker syndrome 119 Cornelia de Lange 102 Goldenhar syndrome 98 Usher II syndrome 83 Wolf-Hirschhorn syndrome (Trisomy 4p) 68 Trisomy 13 (Trisomy 13-15, Patau syndrome) 60 Pierre-Robin syndrome 57 Moebius syndrome 55 Trisomy 18 (Edwards syndrome) 52 Norrie disease 38 Leber congenital amaurosis 35 Chromosome 18, Ring 18 31 Aicardi syndrome 29 Alstrom syndrome 27 Pfieffer syndrome 27 Treacher Collins syndrome 27 Waardenburg syndrome 27 Marshall syndrome 25 Refsum syndrome 21 Cri du chat syndrome (Chromosome 5p- synd) 16 Bardet-Biedl syndrome (Laurence Moon-Biedl) 15 Hurler syndrome (MPS I-H) 15 Crouzon syndrome (Craniofacial Dysotosis) 13 NF1 - Neurofibromatosis (von Recklinghausen dis) 13 Kniest Dysplasia 12 Turner syndrome 11 Usher III syndrome 10 Cockayne syndrome 9 Apert syndrome/Acrocephalosyndactyly, Type 1 8 Leigh Disease 8 Alport syndrome 6 Monosomy 10p 6 NF2 - Bilateral Acoustic Neurofibromatosis 6 Batten disease 5 Kearns-Sayre syndrome 5 Klippel-Feil sequence 5 Hereditary Syndromes and Disorders Count Prader-Willi 5 Sturge-Weber syndrome 5 Marfan syndrome 3 Hand-Schuller-Christian (Histiocytosis X) 2 Hunter Syndrome (MPS II) 2 Maroteaux-Lamy syndrome (MPS VI) 2 Morquio syndrome (MPS IV-B) 2 Optico-Cochleo-Dentate Degeneration 2 Smith-Lemli-Opitz (SLO) syndrome 2 Wildervanck syndrome 2 Herpes-Zoster (or Hunt) 1 Vogt-Koyanagi-Harada -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Generalized Hypertrichosis
Letters to the Editor case of female. Ambras syndrome is a type of universal Generalized hypertrichosis affecting the vellus hair, where there is uniform overgrowth of hair over the face and external hypertrichosis ear with or without dysmorphic facies.[3] Patients with Gingival fi bromaatosis also have generalized hypertrichosis Sir, especially on the face.[4] Congenital hypertrichosis can A 4-year-old girl born out of non-consanguinous marriage occur due to fetal alcohol syndrome and fetal hydentoin presented with generalized increase in body hair noticed syndrome.[5] Prepubertal hypertrichosis is seen in otherwise since birth. None of the other family members were healthy infants and children. There is involvement of affected. Hair was pigmented and soft suggesting vellus hair. face back and extremities Distribution of hair shows an There was generalized increase in body hair predominantly inverted fi r-tree pattern on the back. More commonly seen affecting the back of trunk arms and legs [Figures 1 and 2]. in Mediterranean and South Asian descendants.[6] There is Face was relatively spared except for fore head. Palms and soles were spared. Scalp hair was normal. Teeth and nail usually no hormonal alterations. Various genodermatosis were normal. There was no gingival hypertrophy. No other associated with hypertrichosis as the main or secondary skeletal or systemic abnormalities were detected clinically. diagnostic symptom are: Routine blood investigations were normal. Hormonal Lipoatrophy (Lawrernce Seip syndrome) study was within normal limit for her age. With this Cornelia de Lange syndrome clinical picture of generalized hypertrichosis with no other Craniofacial dysostosis associated anomalies a diagnosis of universal hypertrichosis Winchester syndrome was made. -

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

CHARGE Syndrome
orphananesthesia Anaesthesia recommendations for CHARGE syndrome Disease name: CHARGE syndrome ICD 10: Q87.8 Synonyms: CHARGE association; Hall-Hittner syndrome Disease summary: CHARGE syndrome was initially defined as a non-random association of anomalies: - Coloboma - Heart defect - Atresia choanae (choanal atresia) - Retarded growth and development - Genital hypoplasia - Ear anomalies/deafness In 1998, an expert group defined the major (the classical 4C´s: Choanal atresia, Coloboma, Characteristic ear and Cranial nerve anomalies) and minor criteria of CHARGE syndrome [1]. In 2004, mutations in the CHD7 gene were identified as the major cause. The inheritance pattern is autosomal dominant with variable expressivity. Almost all mutations occurs de novo, but parent-to-child transmission has occasionally been reported [2]. Clinical criteria for CHARGE syndrome [1] Major criteria: • Coloboma • Choanal Atresia • Cranial nerve anomalies • Abnormalities of the inner, middle, or external ear Minor criteria: • Cardiaovascular malformations • Genital hypoplasia or delayed pubertal development • Cleft lip and/or palate • Tracheoesophageal defects • Distinctive CHARGE facies • Growth retardation • Developmental delay Occasional: • Renal anomalies: duplex system, vesicoureteric reflux • Spinal anomalies: scoliosis, osteoporosis • Hand anomalies 1 • Neck/shoulder anomalies • Immune system disorders Individuals with all four major characteristics or three major and three minor characteristics are highly likely to have CHARGE syndrome [1]. CHARGE syndrome -

CHARGE Factsheet 3 Clinical Diagnosis and Features
The Information Pack CHARGE for Practitioners Factsheet 3 CHARGE syndrome: major and minor medical diagnostic criteria plus later onset features DR JEREMY KIRK, MD, FRCP, FRCPCH, Consultant Paediatric Endocrinologist, Birmingham Children’s Hospital Original diagnostic criteria The initial association of coloboma and choanal atresia with other congenital abnormalities was first described by Hall and separately Hittner et al. in 1979 (Hall, 1979; Hittner et al., 1979). In 1981 there was further description and expansion of the condition (Pagon et al., 1981). It was at this stage that the acronym CHARGE (C–coloboma, H–heart disease, A–atresia choanae, R–retarded growth and retarded development and/or CNS anomalies, G–genital hypoplasia, and E–ear anomalies and/or deafness) was made. In order to make the diagnosis of CHARGE syndrome, historically four out of six of the features of the acronym needed to be fulfilled, although one should be either choanal atresia or a coloboma (Pagon et al., 1981). From association to syndrome been several attempts to refine the diagnostic criteria, Initially CHARGE was described as an association; namely by Blake et al. (1998) and Verloes (2005). Both a nonrandom collection of birth defects, rather than of these use major features which are very specific for a syndrome, which is a more recognisable pattern of CHARGE syndrome, along with other minor features. birth defects (often with a known genetic cause). With the identification of the gene CHD7 in 2004 (Vissers The criteria suggested by Blake et al. consist of four et al., 2004) it has now been renamed a syndrome, major ‘C’s: as CHD7 is mutated in at least 60% of patients with 1. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause. -

Duchenne Muscular Dystrophy (DMD)
Pediatric Residents Review Session A bit of a hodge podge to keep you guessing December 20, 2018 Natarie Liu, FRCPC, Pediatric Neurology Email me for resources (OSCE handbook, etc) Thanks to Dr. K. Smyth and Dr. K Murias for inspiration for some of the slides Case 3mo girl with hypotonia, hypotonic facies, 1+ symmetric DTR. What is the most likely diagnosis? a. Congenital muscular dystrophy b. Myotonic dystrophy c. SMA1 d. Nemaline rod Stem not giving this picture OR this picture What is this? Dystrophinopathies Duchenne Muscular Dystrophy Becker Muscular Dystrophy Dystrophinopathies By convention, if boy stops walking before age 12, this is Duchenne Muscular Dystrophy (DMD) If they remain ambulatory after their 16th birthday, are typically considered to have Becker Muscular Dystrophy (BMD) Anything in between is an intermediate phenotype Some centres transition to using Dystrophinopathies as the term Dystrophinopathies are X-linked disorders Dystrophinopathies: Epidemiology Duchenne Muscular Dystrophy 1:3500 live male births but newborn screening places the incidence closer to 1:5000 live male births Mean lifespan 19 years traditionally, now greater than 25 years (with multidisciplinary team management and corticosteroid use) Becker Muscular Dystrophy Incidence 1/10th-1/5th of DMD Prevalence 60-90% more than DMD DMD: Clinical Features Boys often present between 3-5 years of age Delayed motor milestones and falls, difficulty running and jumping Gain motor milestones through 6-7 years of age, progressive weakness after Wheelchair before age 12, historically Examination Calf hypertrophy Mild lordotic posture Waddling of gait Poor hip excursion during running Head lag when pulled from sitting from supine Partial Gower maneuver when rising from floor. -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome -

Congenital Ocular Anomalies in Newborns: a Practical Atlas
www.jpnim.com Open Access eISSN: 2281-0692 Journal of Pediatric and Neonatal Individualized Medicine 2020;9(2):e090207 doi: 10.7363/090207 Received: 2019 Jul 19; revised: 2019 Jul 23; accepted: 2019 Jul 24; published online: 2020 Sept 04 Mini Atlas Congenital ocular anomalies in newborns: a practical atlas Federico Mecarini1, Vassilios Fanos1,2, Giangiorgio Crisponi1 1Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy 2Department of Surgery, University of Cagliari, Cagliari, Italy Abstract All newborns should be examined for ocular structural abnormalities, an essential part of the newborn assessment. Early detection of congenital ocular disorders is important to begin appropriate medical or surgical therapy and to prevent visual problems and blindness, which could deeply affect a child’s life. The present review aims to describe the main congenital ocular anomalies in newborns and provide images in order to help the physician in current clinical practice. Keywords Congenital ocular anomalies, newborn, anophthalmia, microphthalmia, aniridia, iris coloboma, glaucoma, blepharoptosis, epibulbar dermoids, eyelid haemangioma, hypertelorism, hypotelorism, ankyloblepharon filiforme adnatum, dacryocystitis, dacryostenosis, blepharophimosis, chemosis, blue sclera, corneal opacity. Corresponding author Federico Mecarini, MD, Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy; tel.: (+39) 3298343193; e-mail: [email protected].