Crouzon Syndrome Genetic and Intervention Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2018 Etiologies by Frequencies
2018 Etiologies in Order of Frequency by Category Hereditary Syndromes and Disorders Count CHARGE Syndrome 958 Down syndrome (Trisomy 21 syndrome) 308 Usher I syndrome 252 Stickler syndrome 130 Dandy Walker syndrome 119 Cornelia de Lange 102 Goldenhar syndrome 98 Usher II syndrome 83 Wolf-Hirschhorn syndrome (Trisomy 4p) 68 Trisomy 13 (Trisomy 13-15, Patau syndrome) 60 Pierre-Robin syndrome 57 Moebius syndrome 55 Trisomy 18 (Edwards syndrome) 52 Norrie disease 38 Leber congenital amaurosis 35 Chromosome 18, Ring 18 31 Aicardi syndrome 29 Alstrom syndrome 27 Pfieffer syndrome 27 Treacher Collins syndrome 27 Waardenburg syndrome 27 Marshall syndrome 25 Refsum syndrome 21 Cri du chat syndrome (Chromosome 5p- synd) 16 Bardet-Biedl syndrome (Laurence Moon-Biedl) 15 Hurler syndrome (MPS I-H) 15 Crouzon syndrome (Craniofacial Dysotosis) 13 NF1 - Neurofibromatosis (von Recklinghausen dis) 13 Kniest Dysplasia 12 Turner syndrome 11 Usher III syndrome 10 Cockayne syndrome 9 Apert syndrome/Acrocephalosyndactyly, Type 1 8 Leigh Disease 8 Alport syndrome 6 Monosomy 10p 6 NF2 - Bilateral Acoustic Neurofibromatosis 6 Batten disease 5 Kearns-Sayre syndrome 5 Klippel-Feil sequence 5 Hereditary Syndromes and Disorders Count Prader-Willi 5 Sturge-Weber syndrome 5 Marfan syndrome 3 Hand-Schuller-Christian (Histiocytosis X) 2 Hunter Syndrome (MPS II) 2 Maroteaux-Lamy syndrome (MPS VI) 2 Morquio syndrome (MPS IV-B) 2 Optico-Cochleo-Dentate Degeneration 2 Smith-Lemli-Opitz (SLO) syndrome 2 Wildervanck syndrome 2 Herpes-Zoster (or Hunt) 1 Vogt-Koyanagi-Harada -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Generalized Hypertrichosis
Letters to the Editor case of female. Ambras syndrome is a type of universal Generalized hypertrichosis affecting the vellus hair, where there is uniform overgrowth of hair over the face and external hypertrichosis ear with or without dysmorphic facies.[3] Patients with Gingival fi bromaatosis also have generalized hypertrichosis Sir, especially on the face.[4] Congenital hypertrichosis can A 4-year-old girl born out of non-consanguinous marriage occur due to fetal alcohol syndrome and fetal hydentoin presented with generalized increase in body hair noticed syndrome.[5] Prepubertal hypertrichosis is seen in otherwise since birth. None of the other family members were healthy infants and children. There is involvement of affected. Hair was pigmented and soft suggesting vellus hair. face back and extremities Distribution of hair shows an There was generalized increase in body hair predominantly inverted fi r-tree pattern on the back. More commonly seen affecting the back of trunk arms and legs [Figures 1 and 2]. in Mediterranean and South Asian descendants.[6] There is Face was relatively spared except for fore head. Palms and soles were spared. Scalp hair was normal. Teeth and nail usually no hormonal alterations. Various genodermatosis were normal. There was no gingival hypertrophy. No other associated with hypertrichosis as the main or secondary skeletal or systemic abnormalities were detected clinically. diagnostic symptom are: Routine blood investigations were normal. Hormonal Lipoatrophy (Lawrernce Seip syndrome) study was within normal limit for her age. With this Cornelia de Lange syndrome clinical picture of generalized hypertrichosis with no other Craniofacial dysostosis associated anomalies a diagnosis of universal hypertrichosis Winchester syndrome was made. -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -

Possible Causes of Deaf-Blindness
1 Nebraska Deaf-Blind Project Fact Sheet, December 2014 Possible Causes of Combined Hearing and Vision Losses (Dual Sensory Impairments/Deaf-Blindness) By Teresa Coonts, Project Director Aicardi Syndrome Marfan Syndrome Alport Syndrome Marshall Syndrome Alstrom Syndrome Maroteaux-Lamy Syndrome Apert Syndrome Maternal Drug Use Asphyxia Meningitis Bardet-Biedl Syndrome Microcephaly Batten Disease Moebius Syndrome CHARGE Syndrome Mohr-Tranebjaerg Chromosome 18 Monosomy 10p Cockayne Syndrome Morquio Syndrome Cogan’s Syndrome Neonatal Herpes Simplex (HSV) Congenital rubella syndrome NF1-Neurofibromatosis (von Cornelia de Lange Syndrome (CdLs) Recklinghausen disease) Craniosynostosis (Aipert, Crouzon and NF2-Bilateral Acoustic Neurofibromatosis Pfeiffer) Norrie Disease Cri du Chat Syndrome Optico-Cochleo-Dentate Degeneration Crigler-Najjar syndrome Pallister Killian Mosaic Syndrome Crouzon Syndrome Peroxisomal disorders (including Refsum Cytomegalovirus (CMV) Disease, Zellweger syndrome, and Dandy-Walker Syndrome Infantile Adrenoleukodystrophy) Direct Trauma to the Eye and Ear Pfieffer Syndrome Down Syndrome Prader-Willi Syndrome Duane Syndrome Pierre-Robin Syndrome Encephalitis Scheie Syndrome Fetal Alcohol Syndrome Severe Head/Brain Injury Flynn Aird Syndrome Smith-Lemli-Opitz (SLO) Syndrome or Friedreich’s Ataxia (Spinocerebellar (SLOS) degeneration) Stickler Syndrome Goldenhar Syndrome Stroke Hand-Schuller-Christian disease (also Sturge-Weber Syndrome 1 2 known as Histiocytosis) Congenital Syphillis Herpes zoster (not at birth or childhood -

Improving Diagnosis and Treatment of Craniofacial Malformations Utilizing Animal Models
CHAPTER SEVENTEEN From Bench to Bedside and Back: Improving Diagnosis and Treatment of Craniofacial Malformations Utilizing Animal Models Alice F. Goodwin*,†, Rebecca Kim*,†, Jeffrey O. Bush*,{,},1, Ophir D. Klein*,†,},},1 *Program in Craniofacial Biology, University of California San Francisco, San Francisco, California, USA †Department of Orofacial Sciences, University of California San Francisco, San Francisco, California, USA { Department of Cell and Tissue Biology, University of California San Francisco, San Francisco, California, USA } Department of Pediatrics, University of California San Francisco, San Francisco, California, USA } Institute for Human Genetics, University of California San Francisco, San Francisco, California, USA 1Corresponding authors: e-mail address: [email protected]; [email protected] Contents 1. Models to Uncover Genetics of Cleft Lip and Palate 460 2. Treacher Collins: Proof of Concept of a Nonsurgical Therapeutic for a Craniofacial Syndrome 467 3. RASopathies: Understanding and Developing Treatment for Syndromes of the RAS Pathway 468 4. Craniosynostosis: Pursuing Genetic and Pharmaceutical Alternatives to Surgical Treatment 473 5. XLHED: Developing Treatment Based on Knowledge Gained from Mouse and Canine Models 477 6. Concluding Thoughts 481 Acknowledgments 481 References 481 Abstract Craniofacial anomalies are among the most common birth defects and are associated with increased mortality and, in many cases, the need for lifelong treatment. Over the past few decades, dramatic advances in the surgical and medical care of these patients have led to marked improvements in patient outcomes. However, none of the treat- ments currently in clinical use address the underlying molecular causes of these disor- ders. Fortunately, the field of craniofacial developmental biology provides a strong foundation for improved diagnosis and for therapies that target the genetic causes # Current Topics in Developmental Biology, Volume 115 2015 Elsevier Inc. -
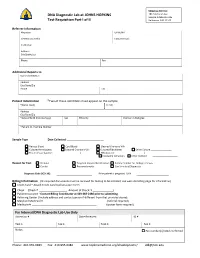
DNA Diagnostic Lab at JOHNS HOPKINS Test Requisition Part I of II
Shipping Address: DNA Diagnostic Lab at JOHNS HOPKINS 1812 Ashland Ave Sample Intake Rm 245 Test Requisition Part I of II Baltimore, MD 21205 Referrer Information Physician UPIN /NPI Genetic Counselor Contact Email: Institution Address City/State/Zip Phone Fax Additional Reports to Name /Institution Address City/State/Zip Phone Fax Patient Information *Two of these identifiers must appear on the sample *Name (Last) (First) Address City/State/Zip *Date of Birth (mm/dd/yyyy) Sex Ethnicity Position in Pedigree *Patient ID / Sample Number Sample Type Date Collected: _________________________ Venous Blood Cord Blood Cleaned Chorionic Villi Cultured Amniocytes Cultured Chorionic Villi Cultured Fibroblasts Other Culture ________________ Frozen tissue (source: _____________________) DNA (source: ______________________) PureGene Extraction Other method Reason for Test Prenatal Targeted Variant Identification Family member for Linkage analysis Carrier Presymptomatic Confirmatory/Diagnostic Diagnosis Code (ICD‐10): If the patient is pregnant: LMP Billing Information (All required documents must be received for testing to be initiated; see web site billing page for information) Credit Card – Attach Credit Card Authorization Form Check (Check # Amount of Check: $ ) Patient Insurance ‐ Contact Billing Coordinator at 443‐287‐2486 prior to submitting. Referring Center (Include address and contact person if different from that provided above) Maryland Medicaid # __________________________________ (referral required) Medicare # ____________________________________________ -

Table I. Genodermatoses with Known Gene Defects 92 Pulkkinen
92 Pulkkinen, Ringpfeil, and Uitto JAM ACAD DERMATOL JULY 2002 Table I. Genodermatoses with known gene defects Reference Disease Mutated gene* Affected protein/function No.† Epidermal fragility disorders DEB COL7A1 Type VII collagen 6 Junctional EB LAMA3, LAMB3, ␣3, 3, and ␥2 chains of laminin 5, 6 LAMC2, COL17A1 type XVII collagen EB with pyloric atresia ITGA6, ITGB4 ␣64 Integrin 6 EB with muscular dystrophy PLEC1 Plectin 6 EB simplex KRT5, KRT14 Keratins 5 and 14 46 Ectodermal dysplasia with skin fragility PKP1 Plakophilin 1 47 Hailey-Hailey disease ATP2C1 ATP-dependent calcium transporter 13 Keratinization disorders Epidermolytic hyperkeratosis KRT1, KRT10 Keratins 1 and 10 46 Ichthyosis hystrix KRT1 Keratin 1 48 Epidermolytic PPK KRT9 Keratin 9 46 Nonepidermolytic PPK KRT1, KRT16 Keratins 1 and 16 46 Ichthyosis bullosa of Siemens KRT2e Keratin 2e 46 Pachyonychia congenita, types 1 and 2 KRT6a, KRT6b, KRT16, Keratins 6a, 6b, 16, and 17 46 KRT17 White sponge naevus KRT4, KRT13 Keratins 4 and 13 46 X-linked recessive ichthyosis STS Steroid sulfatase 49 Lamellar ichthyosis TGM1 Transglutaminase 1 50 Mutilating keratoderma with ichthyosis LOR Loricrin 10 Vohwinkel’s syndrome GJB2 Connexin 26 12 PPK with deafness GJB2 Connexin 26 12 Erythrokeratodermia variabilis GJB3, GJB4 Connexins 31 and 30.3 12 Darier disease ATP2A2 ATP-dependent calcium 14 transporter Striate PPK DSP, DSG1 Desmoplakin, desmoglein 1 51, 52 Conradi-Hu¨nermann-Happle syndrome EBP Delta 8-delta 7 sterol isomerase 53 (emopamil binding protein) Mal de Meleda ARS SLURP-1 -

Date Due Date Due Date Due
PLACE ll RETURN BOX to roman this chockout from your mood. TO AVOID FINES Mom on or baton dd. duo. DATE DUE DATE DUE DATE DUE MSU In An Affirmative Action/Equal Opponfirmy Inflation mm: SCREENING FOR MUTATIONS IN PAX3 AND MITF IN WAARDENBURG SYNDROME AND WAARDENBURG SYNDROME-LIKE INDIVIDUALS By Melisa Lynn Carey A THESIS Submitted to Michigan State University in partial fulfillment of the requirements for a degree of MASTER OF SCIENCE Department of Zoology 1 996 ABSTRACT SCREENING FOR MUTATIONS IN PAX3 AND MITF IN WAARDENBURG SYNDROME AND WAARDENBURG SYNDROME-LIKE INDIVIDUALS BY Melisa L. Carey Waardenburg Syndrome (WS) is an autosomal dominant disorder characterized by pigmentary and facial anomalies and congenital deafness. Mutations causing WS have been reported in PAX3 and MITF. The goal of this study was to characterize the molecular defects in 33 unrelated WS individuals. Mutation detection was performed using Single Strand Conformational Polymorphism (SSCP) analysis and sequencing methods. Among the 33 WS individuals, a total of eight mutations were identified, seven in PAX3 and one in MITF. In this study, one of the eight mutations was identified and characterized in PAX3 exon seven in a WSI family (UoM1). The proband of UoM1 also has Septo-Optic Dysplasia. In a large family (MSU22) with WS-Iike dysmorphology and additional craniofacial anomalies, linkage was excluded to PAX3 and no mutations were identified in MITF. Herein I review the status of mutation detection in our proband screening set and add to the understanding of the role of PAX3 and MITF in development by exploring new phenotypic characteristics associated with WS. -

Crouzono-Dermo-Skeletal Syndrome, Crouzon Syndrome with Acanthosis Nigricans Syndrome
Journal of Perinatology (2014) 34, 164–165 & 2014 Nature America, Inc. All rights reserved 0743-8346/14 www.nature.com/jp IMAGING CASE REPORT Crouzono-dermo-skeletal syndrome, Crouzon syndrome with acanthosis nigricans syndrome TE Herman, K Sargar and MJ Siegel Journal of Perinatology (2014) 34, 164–165; doi:10.1038/jp.2013.139 CASE PRESENTATION mutation-associated conditions include five skeletal dysplasias: A 3495 g infant girl was born at 39 weeks gestation to a 17-year- achondroplasia, hypochondroplasia, thanatophoric dysplasia type 1 old gravida 1, para 0 mother. The mother had Crouzon syndrome 1, thanatophoric dysplasia type 2 and SADDAM syndrome. and hydrocephalus. She had undergone 11 craniofacial and plastic surgical procedures. The mother previously had genetic testing, which demonstrated a mutation in exon 10 of the FGFR3 (fibroblast growth factor receptor number 3) gene consistent with Crouzon syndrome with acanthosis nigricans (AN), also called Crouzono-dermo-skeletal syndrome (CDSS). No sonographic abnormalities were detected in the fetus during the pregnancy. At delivery, the infant had Apgars of 1 at 1 min, 6 at 5 min and 7 at 10 min. A nasogastric tube could not be passed. The patient was noted to have proptosis, depressed nasal bridge, hypertelorism, an anterior ectopic anus and normal appearing skin. Craniofacial computed tomography (CT) scan was performed (Figures 1 and 2) and plain radiographs of the pelvis and lumbar spine obtained (Figure 3). DENOUEMENT AND DISCUSSION The craniofacial CT scan demonstrates bicoronal synostosis with marked midface hypoplasia, with exophthalmos and hypertelor- ism. In addition, there was bilateral marked choanal stenosis. The pelvis (Figure 3) demonstrates squared-off iliac wings with small sciatic notches and narrowing of the lumbar interpediculate distances. -

EUROCAT Syndrome Guide
JRC - Central Registry european surveillance of congenital anomalies EUROCAT Syndrome Guide Definition and Coding of Syndromes Version July 2017 Revised in 2016 by Ingeborg Barisic, approved by the Coding & Classification Committee in 2017: Ester Garne, Diana Wellesley, David Tucker, Jorieke Bergman and Ingeborg Barisic Revised 2008 by Ingeborg Barisic, Helen Dolk and Ester Garne and discussed and approved by the Coding & Classification Committee 2008: Elisa Calzolari, Diana Wellesley, David Tucker, Ingeborg Barisic, Ester Garne The list of syndromes contained in the previous EUROCAT “Guide to the Coding of Eponyms and Syndromes” (Josephine Weatherall, 1979) was revised by Ingeborg Barisic, Helen Dolk, Ester Garne, Claude Stoll and Diana Wellesley at a meeting in London in November 2003. Approved by the members EUROCAT Coding & Classification Committee 2004: Ingeborg Barisic, Elisa Calzolari, Ester Garne, Annukka Ritvanen, Claude Stoll, Diana Wellesley 1 TABLE OF CONTENTS Introduction and Definitions 6 Coding Notes and Explanation of Guide 10 List of conditions to be coded in the syndrome field 13 List of conditions which should not be coded as syndromes 14 Syndromes – monogenic or unknown etiology Aarskog syndrome 18 Acrocephalopolysyndactyly (all types) 19 Alagille syndrome 20 Alport syndrome 21 Angelman syndrome 22 Aniridia-Wilms tumor syndrome, WAGR 23 Apert syndrome 24 Bardet-Biedl syndrome 25 Beckwith-Wiedemann syndrome (EMG syndrome) 26 Blepharophimosis-ptosis syndrome 28 Branchiootorenal syndrome (Melnick-Fraser syndrome) 29 CHARGE