Program Book
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Radical Pacifism, Civil Rights, and the Journey of Reconciliation
09-Mollin 12/2/03 3:26 PM Page 113 The Limits of Egalitarianism: Radical Pacifism, Civil Rights, and the Journey of Reconciliation Marian Mollin In April 1947, a group of young men posed for a photograph outside of civil rights attorney Spottswood Robinson’s office in Richmond, Virginia. Dressed in suits and ties, their arms held overcoats and overnight bags while their faces carried an air of eager anticipation. They seemed, from the camera’s perspective, ready to embark on an exciting adventure. Certainly, in a nation still divided by race, this visibly interracial group of black and white men would have caused people to stop and take notice. But it was the less visible motivations behind this trip that most notably set these men apart. All of the group’s key organizers and most of its members came from the emerging radical pacifist movement. Opposed to violence in all forms, many had spent much of World War II behind prison walls as conscientious objectors and resisters to war. Committed to social justice, they saw the struggle for peace and the fight for racial equality as inextricably linked. Ardent egalitarians, they tried to live according to what they called the brotherhood principle of equality and mutual respect. As pacifists and as militant activists, they believed that nonviolent action offered the best hope for achieving fundamental social change. Now, in the wake of the Second World War, these men were prepared to embark on a new political jour- ney and to become, as they inscribed in the scrapbook that chronicled their traveling adventures, “courageous” makers of history.1 Radical History Review Issue 88 (winter 2004): 113–38 Copyright 2004 by MARHO: The Radical Historians’ Organization, Inc. -

What Made Nonviolent Protest Effective During the Civil Rights Movement?
NEW YORK STATE SOCIAL STUDIES RESOURCE TOOLKIT 5011th Grade Civil Rights Inquiry What Made Nonviolent Protest Effective during the Civil Rights Movement? © Bettmann / © Corbis/AP Images. Supporting Questions 1. What was tHe impact of the Greensboro sit-in protest? 2. What made tHe Montgomery Bus Boycott, BirmingHam campaign, and Selma to Montgomery marcHes effective? 3. How did others use nonviolence effectively during the civil rights movement? THIS WORK IS LICENSED UNDER A CREATIVE COMMONS ATTRIBUTION- NONCOMMERCIAL- SHAREALIKE 4.0 INTERNATIONAL LICENSE. 1 NEW YORK STATE SOCIAL STUDIES RESOURCE TOOLKIT 11th Grade Civil Rights Inquiry What Made Nonviolent Protest Effective during the Civil Rights Movement? 11.10 SOCIAL AND ECONOMIC CHANGE/DOMESTIC ISSUES (1945 – PRESENT): Racial, gender, and New York State socioeconomic inequalities were addressed By individuals, groups, and organizations. Varying political Social Studies philosophies prompted debates over the role of federal government in regulating the economy and providing Framework Key a social safety net. Idea & Practices Gathering, Using, and Interpreting Evidence Chronological Reasoning and Causation Staging the Discuss tHe recent die-in protests and tHe extent to wHicH tHey are an effective form of nonviolent direct- Question action protest. Supporting Question 1 Supporting Question 2 Supporting Question 3 Guided Student Research Independent Student Research What was tHe impact of tHe What made tHe Montgomery Bus How did otHers use nonviolence GreensBoro sit-in protest? boycott, the Birmingham campaign, effectively during tHe civil rights and tHe Selma to Montgomery movement? marcHes effective? Formative Formative Formative Performance Task Performance Task Performance Task Create a cause-and-effect diagram tHat Detail tHe impacts of a range of actors Research the impact of a range of demonstrates the impact of the sit-in and tHe actions tHey took to make tHe actors and tHe effective nonviolent protest by the Greensboro Four. -

Community Foundation of Jackson Hole Annual
COMMUNITY FOUNDATION OF JACKSON HOLE ANNUAL REPORT / 2018 TA B L E Welcome Letter 3 OF CONTENTS About Us 4 Donor Story 6 Professional Development & Resources 8 Competitive Grants 10 Youth Philanthropy 12 Micro Grants 16 Opportunities Fund 18 Collective Impact 20 Legacy Society 24 1 Fund Highlights 24-25 Key Financial Indicators 26 Donor Story 28 The Foundation Circle 30 Community Foundation Funds 34 Old Bill’s Fun Run 36 Co-Challengers 38 Friends of the Match 42 Gifts to Funds 44 Community Foundation of Teton Valley 46 Behind the Scenes 48 In Memoriam 50 Community Foundation of Jackson Hole / Annual Report 2018 2 Fund & Program Highlight HELLO, Mr. and Mrs. Old Bill say it best. They have always led with the question, “How can we help?” Their initial vision was to inspire “we” to become “all of us.” And it has. In 2018, you raised an astonishing amount, bringing Old Bill’s Fun Run’s 22-year total to more than $159 million for local nonprofits. Inside these pages, you will see the impact of our remarkable community’s generosity. In fact, one out of every three families in Teton County takes part in Old Bill’s—an event that has become a national model for collaborative fundraising. Old Bill’s lasts only a morning, but because of your support, we are touching lives and working for the community 3 every day. Nonprofits rely on us for professional workshops and resources and receive critical funding through our Competitive and Capacity Building grant opportunities. We convene Community Conversations to find collaborative solutions to local problems. -

June/July 2010 Education Coordinator by Rosalie Nagler I N T H I S I S S U E As We Move Into Summer in East Tennessee, We Look Forward to New Beginnings
Heska Amuna Welcomes New Rabbi, Volume 2 ♦ Issue 6 ♦ June/July 2010 Education Coordinator By Rosalie Nagler I N T H I S I S S U E As we move into summer in East Tennessee, we look forward to new beginnings. We welcome a new rabbi who Heska Amuna HaShofar starts in August with the the arrival of Rabbi Alon Ferency From the Rabbi’s Desk……………...1 and his wife, Karen. They come to us from Los Angeles, where Rabbi Ferency graduated in May from the Ziegler From the Chair...………………..….1 School of Rabbinic Studies. By birth, Rabbi Ferency is from Kitchen & Kiddush News………......3 the northeast, having grown up in Massachusetts. He HARS News………………..…..….….4 attended Harvard and has traveled extensively. We anticipate welcoming him to ―Volunteer Country‖ with typical southern hospitality. Among Our Members…………...….6 Anna Iroff will be our religious school coordinator. Anna comes to us as one of our Contributions……………………......6 ―kids‖ who grew up at Heska Amuna and went on to study at the Albert A. List College of Jewish Studies, an undergraduate program of the Jewish Theological Seminary in New York. While studying there, Anna also worked as a religious school teacher and is very Temple Beth El Times excited to guide our religious school. She has taught the Confirmation class the past two years and and adult education classes. We look forward to her collaborating with Rabbi From the Rabbi’s Study….………..11 Ferency to create a bright future for the next generation of Heska Amuna ―kids!‖ President’s Message…………..…...12 As you can see, Heska Amuna Synagogue has many opportunities open to us for a renewal in our congregation. -

Papers of the Naacp
A Guide to the Microfilm Edition of BLACK STUDIES RESEARCH SOURCES Microfilms from Major Archival and Manuscript Collections General Editors: John H. Bracey, Jr., Sharon Harley, and August Meier PAPERS OF THE NAACP Part Selected Branch Files, 27 1956-1965 Series B: The Northeast UNIVERSITY PUBLICATIONS OF AMERICA A Guide to the Microfilm Edition of BLACK STUDIES RESEARCH SOURCES Microfilms from Major Archival and Manuscript Collections General Editors: John H. Bracey, Jr., Sharon Harley, and August Meier PAPERS OF THE NAACP Part 27: Selected Branch Files, 1956-1965 Series B: The Northeast Edited by John H. Bracey, Jr., Sharon Harley, and August Meier Project Coordinator Randolph Boehm Guide compiled by Daniel Lewis A microfilm project of UNIVERSITY PUBLICATIONS OF AMERICA An Imprint of CIS 4520 East-West Highway * Bethesda, MD 20814-3389 Library of Congress Cataloging-in-Publication Data National Association for the Advancement of Colored People. Papers of the NAACP. [microform] Accompanied by printed reel guides. Contents: pt. 1. Meetings of the Board of Directors, records of annual conferences, major speeches, and special reports, 1909-1950 / editorial adviser, August Meier; edited by Mark Fox--pt. 2. Personal correspondence of selected NAACP officials, 1919-1939 --[etc.]--pt. 27. Selected Branch Files, 1956-1965. 1. National Association for the Advancement of Colored People--Archives. 2. Afro-Americans--Civil Rights--History--20th century--Sources. 3. Afro- Americans--History--1877-1964--Sources. 4. United States--Race relations--Sources. I. Meier, August, 1923-. II. Boehm, Randolph. III. Title. E185.61 [Microfilm] 973'.0496073 86-892185 ISBN 1-55655-760-4 (microfilm: pt. 27, series B) Copyright © 2001 by University Publications of America. -

Freedom Riders Democracy in Action a Study Guide to Accompany the Film Freedom Riders Copyright © 2011 by WGBH Educational Foundation
DEMOCRACY IN ACTION A STUDY GUIDE TO ACCOMPANY THE FILM FREEDOM RIDERS DEMOCRACY IN ACTION A STUDY GUIDE TO ACCOMPANY THE FILM FREEDOM RIDERS Copyright © 2011 by WGBH Educational Foundation. All rights reserved. Cover art credits: Courtesy of the Birmingham Civil Rights Institute. Back cover art credits: Bettmann/CORBIS. To download a PDF of this guide free of charge, please visit www.facinghistory.org/freedomriders or www.pbs.org/freedomriders. ISBN-13: 978-0-9819543-9-4 ISBN-10: 0-9819543-9-1 Facing History and Ourselves Headquarters 16 Hurd Road Brookline, MA 02445-6919 ABOUT FACING HISTORY AND OURSELVES Facing History and Ourselves is a nonprofit and the steps leading to the Holocaust—the educational organization whose mission is to most documented case of twentieth-century engage students of diverse backgrounds in an indifference, de-humanization, hatred, racism, examination of racism, prejudice, and antisemitism antisemitism, and mass murder. It goes on to in order to promote a more humane and explore difficult questions of judgment, memory, informed citizenry. As the name Facing History and legacy, and the necessity for responsible and Ourselves implies, the organization helps participation to prevent injustice. Facing History teachers and their students make the essential and Ourselves then returns to the theme of civic connections between history and the moral participation to examine stories of individuals, choices they confront in their own lives, and offers groups, and nations who have worked to build a framework and a vocabulary for analyzing the just and inclusive communities and whose stories meaning and responsibility of citizenship and the illuminate the courage, compassion, and political tools to recognize bigotry and indifference in their will that are needed to protect democracy today own worlds. -

Charles A. Person Was Born September 27, 1942 and Educated in Atlanta
Charles A. Person was born September 27, 1942 and educated in Atlanta. He graduated in 1960 from David T. Howard High School as Class Salutatorian. Mr. Person is a veteran of the Vietnam War and also of the Civil Rights Movement. He saw action in Da Nang; Chu Lai, Okinawa; Washington DC; Charlotte North Carolina; New Orleans, Louisiana and Atlanta, Georgia. During his days in the Civil Rights Movement, the Klu Klux Klan savagely beat him in Anniston, Alabama and, again, in Birmingham, Alabama. Numerous medals and ribbons have been awarded to Mr. Person for his hard work and dedication. He retired from the United States Marine Corps in 1981 on the island of Cuba. He remained at Guantanamo Bay Navy Base where he managed an electronic maintenance company for three years. After his retirement from the Marine Corps, Mr. Person continued his career with the Atlanta Public School System as an Electronic Technician. Today, Mr. Person and his wife reside in his hometown Atlanta and are the parents of five children. He is an activist within the community and the NAACP. “LOOK AROUND... WHAT CHANGE NEEDS TO HAPPEN? GET ON THE BUS. MAKE IT HAPPEN.” – CHARLES PERSON A firsthand exploration of the cost of boarding the bus of change to move America forward – written by one of the Civil Rights Movement’s pioneers. At 18, Charles Person was the youngest of the original Freedom Riders. This mix of activists – including future Congressman John Lewis, Congress of Racial Equality Director James Farmer, Reverend Benjamin Elton Cox, journalist and pacifist James Peck, and CORE field secretary Genevieve Hughes – set out by bus in 1961 to discover whether America would abide by a Supreme Court decision that ruled segregation unconstitutional in bus depots, waiting areas, restaurants and restrooms nationwide. -

Introduction
Introduction And those people who are working to bring into being the dream of democracy are not the agitators. They are not the dangerous people in America. They are not the un-American people. They are people who are doing more for America than anybody that we can point to. And I submit to you that it may well be that the Negro is God’s instrument to save the soul of America. Martin Luther King, Jr. 2 January 1961 When forty-three-year-old John F. Kennedy took office on 20 January 1961 as the youngest elected American president, Martin Luther King Jr. had just turned thirty- two but had already risen to national prominence as a result of his leadership role in the Montgomery bus boycott that ended four years earlier. Early in 1957 he had become founding president of the Southern Christian Leadership Conference (SCLC) and subsequently was in great demand as a speaker throughout the nation. His understanding of Gandhian principles had deepened as a result of his 1959 trip to India, but, during the following year, college student sit-in protesters, rather than King, became the vanguard of a sustained civil disobedience campaign. Having already weathered a near-fatal stabbing and six arrests, King was uncertain about how best to support the new militancy. Moving to Atlanta to be near SCLC head- quarters and to serve as co-pastor with his father at Ebenezer Baptist Church, he had assumed a wide range of responsibilities. He relied on his wife, Coretta Scott, to take the lead role of raising their two small children with a third due any day. -

Freedom Rider Correspondence, Publicity Flyers, and Study, 1961-1964
vv7E. L. C OME: HOM RALLY F'OR OUR OWN BERGE"-1 FREEDOM RIDERS Barbara Kay, Byron Baer, Rabbi Herm n TIME: SPO~SORS - (Partial List) • . SAT. OCT. 21, 8 P.M. Charles c. Parlin Sr., Chairman Father Gabriel Ashle, Englewood Rev. G.L. Blackewll, Hackensack ~l,ACf,;: . Rabbi Irwin M. Blank, Tenafly UNITARIAN Arnold Brown, Englewood · CHVR~H ~ev. Harry E. Chase, Englewood 156 Forest Avenue, Rev. John Dexheimer, Hillsdale Paramus, near Rt. 4 Monroe Dowling, Exec. Plr.Orban League Fred Ferber, Mahwah · ' Rev. c. D. Follansbee, Demarest Augustus Harrison, ~res.Berg. Co. PROGRAM: Rev. George Howard, faramus Rev. James A. Mitchell, ~nglewood *MEET AND HEAR THE Rev. Charies Post. Leonia FREEDOM RIDERS The Promethians, Englewood · *SPEAKERS Howard R~dest, Fairlawn *ENTERTAINMENT ilabbt Selig Salkowitzt Fairl$wn *SONGS FROM PRISON Rabbi Louts Sletel, Teatlec~ llev. Mshlon ·"· ~mlth,Jr·.. , l.>ai.-amus ~ev. Walter Taylor, Englewood ~a\:>bi ¥tdr~ Qngar, Westwoo~ kabbl Judah Washer. teaneck jADf1ISSl0N fREE~ Women·'s ~n\•~ ~a~ue foi;- t>eac~ & .Freedom [ ,l vJE. L. C OME: HOM RALLY FOR OUR OWN BERGE~f . FREEDOM RIDERS. Barbara Kay, Byron Baer, TIME: SPOJ.'..JSORS - (Partial List) • . · SAT.OCT. 2 t 8 P.M. Charles c. Parlin Sr., Chairman Father Gabriel Ashie, Englewood .Rev. G.L. Blackewll, Hackensack ~l,,ACE: . Rabbi Irwin M. Blank, Tenafly UNlTARlAN Arnold Brown, Englew~od . CHVR~H Rev. Harry E. C~ase, Englewood John Dexheimer, Hillsdale 156 Forest Avenue, Rev. Monroe Dowling, Exec. Olr.Vrban League Paramus, near Rt. 4 Fred Ferber, Mahwah · ' Rev. c. D. Follansbee, Demarest Augustus Harri~o~, ~res.Berg. -

Oral History Interview – JFK#2, 4/25/1979 Administrative Information
James Farmer Oral History Interview – JFK#2, 4/25/1979 Administrative Information Creator: James Farmer Interviewer: Sheldon Stern Date of Interview: April 25, 1979 Place of Interview: Washington, D.C. Length: 27 pages Biographical Note Farmer, (1920 - 1999); Founder and director, Congress of Racial Equality, 1961 – 1966, discusses the Freedom Rides, the JFK administration and civil rights legislation, and Farmer’s support for RFK in New York, among other issues. Access Open. Usage Restrictions Copyright of these materials have passed to the United States Government upon the death of the interviewee. Users of these materials are advised to determine the copyright status of any document from which they wish to publish. Copyright The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be “used for any purpose other than private study, scholarship, or research.” If a user makes a request for, or later uses, a photocopy or reproduction for purposes in excesses of “fair use,” that user may be liable for copyright infringement. This institution reserves the right to refuse to accept a copying order if, in its judgment, fulfillment of the order would involve violation of copyright law. The copyright law extends its protection to unpublished works from the moment of creation in a tangible form. Direct your questions concerning copyright to the reference staff. -

Visual Narratives of the Portrait Busts of Edmonia Lewis
VISUAL NARRATIVES AND THE PORTRAIT BUSTS OF EDMONIA LEWIS A THESIS IN Art History Presented to the Faculty of the University of Missouri-Kansas City in partial fulfillment of the requirements for the degree MASTER OF ARTS by SUSAN CROWE B.A., University of Missouri-St. Louis, 2006 B.A., St. Louis University, 1997 Kansas City, Missouri 2010 © 2010 SUSAN CROWE ALL RIGHTS RESERVED VISUAL NARRATIVES AND THE PORTRAIT BUSTS OF EDMONIA LEWIS Susan Elizabeth Crowe, Candidate for the Master of Arts Degree University of Missouri-Kansas City, 2010 ABSTRACT This study considers the social and historical significance of the extant portrait busts sculpted by Edmonia Lewis. The Afro-Native American artist is best known for her thematic sculptures such as Forever Free (1867), Hagar (1875), and Death of Cleopatra (1876). The academic attention paid to these works obscures the fact that portrait busts account for over a third of her artistic output. Consequently, Lewis’s portrait busts have not received a concentrated analysis. Who were the individuals portrayed? What were their relationships to the artist? Using Lewis's bust of James Peck Thomas (1874), her only existing portrait of an African-American patron as a case study, this study explores these two questions in depth. Drawing primarily from unpublished court documents, Thomas’s autobiography as well as newspaper articles, this examination opens a unique window into the individual lives of Lewis's subjects, thereby expanding our knowledge of nineteenth-century American visual and cultural history. ii The faculty listed below, appointed by the Dean of the College of Arts and Sciences have examined a thesis titled “Visual Narratives and the Portrait Busts of Edmonia Lewis,” presented by Susan Crowe, candidate for the Master of Arts degree, and certify that in their opinion it is worthy of acceptance. -
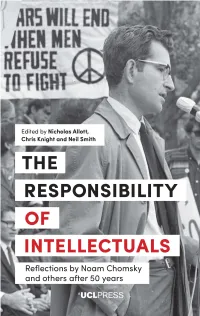
The Responsibility of Intellectuals
The Responsibility of Intellectuals EthicsTheCanada Responsibility and in the FrameAesthetics ofofCopyright, TranslationIntellectuals Collections and the Image of Canada, 1895– 1924 ExploringReflections the by Work Noam of ChomskyAtxaga, Kundera and others and Semprún after 50 years HarrietPhilip J. Hatfield Hulme Edited by Nicholas Allott, Chris Knight and Neil Smith 00-UCL_ETHICS&AESTHETICS_i-278.indd9781787353008_Canada-in-the-Frame_pi-208.indd 3 3 11-Jun-1819/10/2018 4:56:18 09:50PM First published in 2019 by UCL Press University College London Gower Street London WC1E 6BT Available to download free: www.ucl.ac.uk/ucl-press Text © Contributors, 2019 Images © Copyright holders named in captions, 2019 The authors have asserted their rights under the Copyright, Designs and Patents Act 1988 to be identified as authors of this work. A CIP catalogue record for this book is available from The British Library. This book is published under a Creative Commons Attribution Non-commercial Non-derivative 4.0 International license (CC BY-NC-ND 4.0). This license allows you to share, copy, distribute and transmit the work for personal and non-commercial use providing author and publisher attribution is clearly stated. Attribution should include the following information: Allott, N., Knight, C. and Smith, N. (eds). The Responsibility of Intellectuals: Reflections by Noam Chomsky and others after 50 years. London: UCL Press, 2019. https://doi.org/10.14324/ 111.9781787355514 Further details about CC BY licenses are available at http://creativecommons.org/licenses/ Any third-party material in this book is published under the book’s Creative Commons license unless indicated otherwise in the credit line to the material.